Aetna GR 69265 Form


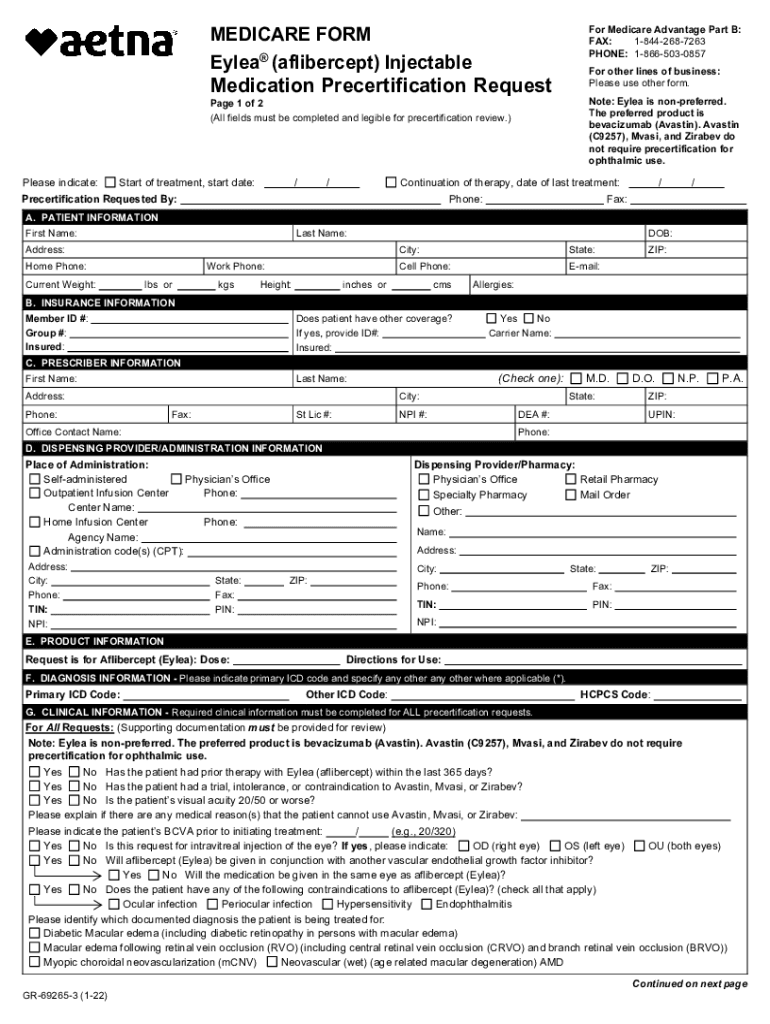
What is the Aetna Eylea Prior Authorization Form?
The Aetna Eylea prior authorization form is a document required by Aetna for patients seeking coverage for Eylea, a medication used to treat certain eye conditions. This form is essential for healthcare providers to obtain approval from Aetna before the medication can be prescribed and covered by insurance. The form includes patient information, details about the prescribed treatment, and medical necessity justification. Completing this form accurately is crucial to ensure timely approval and access to the medication.
Steps to Complete the Aetna Eylea Prior Authorization Form
Completing the Aetna Eylea prior authorization form involves several key steps to ensure that all necessary information is provided. Start by gathering patient details, including name, date of birth, and insurance information. Next, include specifics about the prescribed treatment, such as dosage and frequency. It is also important to provide clinical information that supports the medical necessity of Eylea, including previous treatments and their outcomes. Once the form is filled out, review it for accuracy before submission.
How to Obtain the Aetna Eylea Prior Authorization Form
The Aetna Eylea prior authorization form can typically be obtained through Aetna's official website or by contacting their customer service. Healthcare providers may also have access to the form through their electronic health record (EHR) systems. It is advisable to ensure that you are using the most current version of the form to avoid any delays in the authorization process.
Legal Use of the Aetna Eylea Prior Authorization Form
The Aetna Eylea prior authorization form must be used in compliance with applicable healthcare regulations and Aetna's policies. This includes ensuring that all information provided is accurate and truthful. Misrepresentation or incomplete information can lead to denial of coverage and potential legal consequences. It is vital for healthcare providers to understand the legal implications of submitting this form and to maintain patient confidentiality throughout the process.
Required Documents for Submission
When submitting the Aetna Eylea prior authorization form, certain documents may be required to support the request. These can include the patient's medical history, previous treatment records, and any relevant test results. Providing comprehensive documentation helps to substantiate the medical necessity of Eylea and can facilitate a smoother approval process. Ensure that all documents are organized and submitted alongside the authorization form.
Form Submission Methods
The Aetna Eylea prior authorization form can be submitted through multiple methods, including online submission via Aetna's provider portal, faxing the completed form, or mailing it directly to Aetna's prior authorization department. Each method has its own processing times, so it is important to choose the one that best fits the urgency of the patient's needs. Always confirm the submission method with Aetna to ensure compliance with their requirements.
Quick guide on how to complete aetna gr 69265
Complete Aetna GR 69265 effortlessly on any device
Online document management has become increasingly popular among businesses and individuals. It offers an ideal environmentally-friendly alternative to traditional printed and hand-signed documents, allowing you to access the correct version and securely store it online. airSlate SignNow equips you with all the necessary tools to create, modify, and electronically sign your documents swiftly without delays. Manage Aetna GR 69265 on any device using airSlate SignNow's Android or iOS applications and simplify any document-related process today.
How to edit and eSign Aetna GR 69265 effortlessly
- Obtain Aetna GR 69265 and click Get Form to begin.
- Utilize the provided tools to fill out your form.
- Emphasize relevant sections of the documents or obscure sensitive information using tools that airSlate SignNow offers specifically for this purpose.
- Create your eSignature with the Sign feature, which takes seconds and holds the same legal validity as a conventional wet ink signature.
- Review all the details and click on the Done button to save your modifications.
- Choose how you wish to send your form, whether by email, SMS, or invite link, or download it to your computer.
Eliminate the worry of lost or misplaced documents, tedious form searching, or errors that necessitate printing new document copies. airSlate SignNow meets your document management needs in just a few clicks from your chosen device. Edit and eSign Aetna GR 69265 and ensure outstanding communication throughout your form preparation process with airSlate SignNow.
Create this form in 5 minutes or less
Create this form in 5 minutes!
People also ask
-
What is the Aetna Eylea prior authorization form?
The Aetna Eylea prior authorization form is a document required for insurance providers to grant coverage for Eylea injections. This form ensures that patients meet the medical necessity criteria set by Aetna for the treatment of specific medical conditions.
-
How can airSlate SignNow assist with the Aetna Eylea prior authorization form?
airSlate SignNow streamlines the process of completing and submitting the Aetna Eylea prior authorization form. Our eSignature solution allows you to fill out and electronically sign documents quickly, ensuring a smooth submission process that saves you time and reduces errors.
-
Is there a cost for using airSlate SignNow for the Aetna Eylea prior authorization form?
Yes, airSlate SignNow offers various pricing plans to fit different business needs. You'll find that using our platform for the Aetna Eylea prior authorization form is a cost-effective solution compared to traditional paper methods, especially when considering the increased efficiency and reduced turnaround time.
-
What features does airSlate SignNow offer for handling authorization forms?
airSlate SignNow includes features like customizable templates, automatic reminders, and secure cloud storage that are perfect for managing the Aetna Eylea prior authorization form. These tools enhance your workflow efficiency, ensuring that all forms are completed accurately and promptly.
-
Does airSlate SignNow integrate with other healthcare software?
Absolutely! airSlate SignNow integrates seamlessly with various healthcare software systems, making it easy to manage the Aetna Eylea prior authorization form alongside your existing tools. These integrations ensure that you can maintain a smooth workflow without having to switch between multiple platforms.
-
What benefits do providers gain from using airSlate SignNow for the authorization process?
Providers benefit from increased efficiency and reduced administrative burdens when using airSlate SignNow for the Aetna Eylea prior authorization form. Our eSignature solution allows for quick processing, minimizes paperwork, and helps ensure compliance with regulatory requirements, ultimately improving patient care.
-
Can patients directly access the Aetna Eylea prior authorization form through airSlate SignNow?
Yes, patients can access the Aetna Eylea prior authorization form through airSlate SignNow. This access empowers them to review, fill out, and eSign the necessary documents, making it a convenient option for both patients and providers.
Get more for Aetna GR 69265
- Legal last will and testament form for divorced person not remarried with minor children kentucky
- Legal last will and testament form for divorced person not remarried with adult and minor children kentucky
- Legal last will and testament form for married person with adult children kentucky
- Ky will form
- Legal last will and testament form for married person with minor children kentucky
- Kentucky changes form
- Mutual wills package with last wills and testaments for married couple with adult children kentucky form
- Mutual wills package with last wills and testaments for married couple with no children kentucky form
Find out other Aetna GR 69265
- eSign Alabama Real Estate Affidavit Of Heirship Simple
- eSign California Real Estate Business Plan Template Free
- How Can I eSign Arkansas Real Estate Promissory Note Template
- eSign Connecticut Real Estate LLC Operating Agreement Later
- eSign Connecticut Real Estate LLC Operating Agreement Free
- eSign Real Estate Document Florida Online
- eSign Delaware Real Estate Quitclaim Deed Easy
- eSign Hawaii Real Estate Agreement Online
- Help Me With eSign Hawaii Real Estate Letter Of Intent
- eSign Florida Real Estate Residential Lease Agreement Simple
- eSign Florida Real Estate Limited Power Of Attorney Online
- eSign Hawaii Sports RFP Safe
- eSign Hawaii Sports Warranty Deed Myself
- eSign Louisiana Real Estate Last Will And Testament Easy
- eSign Louisiana Real Estate Work Order Now
- eSign Maine Real Estate LLC Operating Agreement Simple
- eSign Maine Real Estate Memorandum Of Understanding Mobile
- How To eSign Michigan Real Estate Business Plan Template
- eSign Minnesota Real Estate Living Will Free
- eSign Massachusetts Real Estate Quitclaim Deed Myself