Ohio Medicaid Pa Form


What is the Ohio Medicaid Prior Authorization Form?
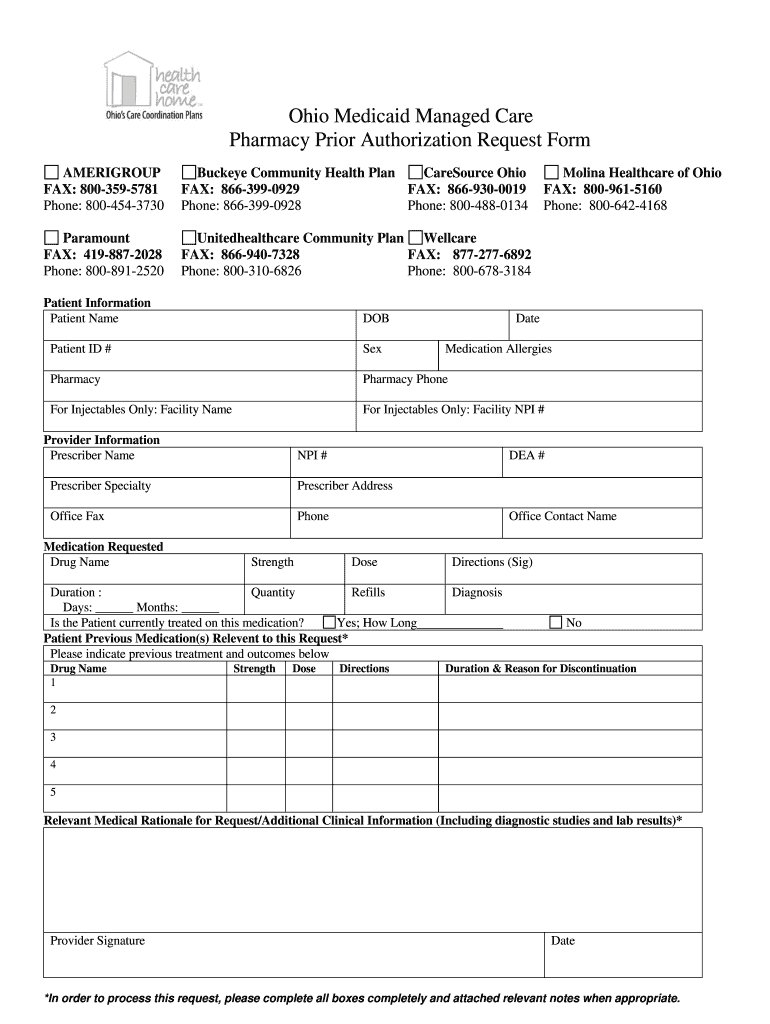
The Ohio Medicaid Prior Authorization Form, commonly referred to as the gainwell prior auth form, is a critical document used to obtain approval for specific medical services, treatments, or medications under the Ohio Medicaid program. This form ensures that the requested services are medically necessary and meet the criteria set by Medicaid. It is essential for healthcare providers to complete this form accurately to facilitate timely access to necessary care for their patients.
How to Use the Ohio Medicaid Prior Authorization Form
Using the Ohio Medicaid Prior Authorization Form involves several key steps. First, healthcare providers must gather all relevant patient information, including medical history and the specific services being requested. Next, the provider fills out the form, ensuring that all sections are completed accurately. Once completed, the form is submitted to the appropriate Medicaid office for review. Providers should keep a copy of the submitted form for their records and follow up on the status of the authorization.
Steps to Complete the Ohio Medicaid Prior Authorization Form
Completing the Ohio Medicaid Prior Authorization Form requires attention to detail. Here are the steps to follow:
- Gather patient information, including name, Medicaid number, and date of birth.
- Document the specific services, treatments, or medications being requested.
- Provide clinical justification for the request, including relevant medical history and documentation.
- Complete all required sections of the form, ensuring clarity and accuracy.
- Submit the form through the designated method, whether online, by mail, or in person.
Key Elements of the Ohio Medicaid Prior Authorization Form
The Ohio Medicaid Prior Authorization Form contains several key elements that must be included for successful processing. These elements include:
- Patient identification details, such as name and Medicaid ID.
- Provider information, including name, contact details, and NPI number.
- Description of the requested service or medication.
- Clinical rationale supporting the necessity of the request.
- Signature of the provider certifying the accuracy of the information provided.
Legal Use of the Ohio Medicaid Prior Authorization Form
The legal use of the Ohio Medicaid Prior Authorization Form is governed by state and federal regulations. It is crucial that healthcare providers adhere to these regulations to ensure compliance and avoid potential penalties. The form must be used solely for its intended purpose—seeking authorization for medically necessary services. Misuse of the form can result in legal consequences, including fines or loss of Medicaid privileges.
Form Submission Methods
The Ohio Medicaid Prior Authorization Form can be submitted through various methods to accommodate different provider preferences. These methods include:
- Online submission via the Ohio Medicaid portal.
- Mailing the completed form to the designated Medicaid office.
- In-person submission at local Medicaid offices.
Quick guide on how to complete ohio medicaid prior authorization form
Explore the simpler method for managing your Ohio Medicaid Pa Form
The traditional techniques for finalizing and endorsing documents consume an excessive amount of time compared to modern document management systems. You used to hunt for appropriate printed forms, produce hard copies, fill in all the information, and mail them. Nowadays, you can acquire, fill out, and sign your Ohio Medicaid Pa Form all in a single web browser tab with airSlate SignNow. Completing your Ohio Medicaid Pa Form has never been easier.
Steps to finalize your Ohio Medicaid Pa Form using airSlate SignNow
- Access the relevant category page and find your state-specific Ohio Medicaid Pa Form. Alternatively, utilize the search bar.
- Verify that the version of the form is accurate by previewing it.
- Click Get form to enter editing mode.
- Fill in your document with the required information using the editing features.
- Inspect the entered information and click the Sign tool to endorse your form.
- Select the most suitable method to create your signature: generate it, draw your signature, or upload an image of it.
- Click DONE to confirm changes.
- Download the document to your device or continue to Sharing settings for electronic distribution.
Efficient online platforms like airSlate SignNow ease the process of completing and submitting your forms. Give it a try to discover how quick document management and approval processes are meant to be. You will save a signNow amount of time.
Create this form in 5 minutes or less
FAQs
-
Why would a doctor send a prescription to a pharmacy, but not respond to repeated requests from the pharmacy to fill out a faxed prior authorization form?
Filling out a prior authorization is not a requirement of our practice. Most of us do this to help our patients, and it is sometimes taken for granted.Think about it. It is your insurance company that is requesting us to fill out this form, taking time away from actually treating patients, to help you save money on your medications. We understand that, and usually do our best to take care of them, but unless we have a large practice, with someone actually paid to spend all their time doing these PA’s, we have to carve out more time from our day to fill out paperwork.It’s also possible, although not likely, that the pharmacy does not have the correct fax number, the faxes have been misplaced, the doctor has some emergencies and is running behind, went on vacation, and so on.Paperwork and insurance requests have become more and more burdensome on our practices, not due to anything on the part of our patients, but a major hassle none the less.
-
How can I fill out the authorization form in Wipro's synergy?
By authorisation form I assume that you mean LOA. Just download the pdf and sign it with stylus or get a printout,sign it and scan the copy.Now upload it!If I my assumption is wrong please provide little clear picture!Thank you!Allah maalik!
-
Do we have to fill out an application form to US universities one year prior to admission?
The college application season for Fall 2019 opens in August 2018. Different colleges have different application timelines and deadlines. Find the requirements for the colleges on your list by googling “college name freshman application deadline”.
-
What does the authorization form in Wipro’s Synergy need to be filled out?
I don't exactly remember how the form was looking like in synergy portal. But I hope it is Authorizing Wipro to do background verification on all the details provided by candidate. It needs your name and signature with date.
-
Why do pharmacies need "prior authorization" to fill some prescriptions? Is the prescription itself not enough? What is prior authorization?
This is a fun answer. FIRST, Pharmacies never require prior authorizations. Do you know why? Because pharmacies don’t pay for your medication, they sell you your medications. Who, besides you, pays for your medications? That’s right, your Insurance Company. It’s completely wrong to think any Pharmacy is holding up your prescription because of a Prior Auth. Pharmacies bill in real time. Unlike Doctors offices. Doctors collect payments on the expected charge. And, if that’s wrong, they ask for more money. And, if you don’t pay them, they send your bill to collections. Pharmacies don’t utilize collection agencies. They bill in real time. That’s why people have to wait for their prescriptions, because the pharmacy has to get the billing absolutely correct at the time of service or else the Pharmacy loses money. Somebody, I don’t know who, decided it was the Pharmacies responsibility to make sure the Patient’s Insurance pays for the Patient’s medications that the Doctor prescribed. In the prior authorization process, pharmacies have essentially nothing to do with any of it, except get yelled at by angry customers.Here’s the breakdown. Insurance companies are still businesses. They are in the business of making money. To keep deductibles affordable, they can not cover every medication. So, they make what is called a formulary. Which are the medications the Insurance Company prefers to cover. This gives the Insurance company wiggle room to make money. It allows them to work contracts with drug companies, and to cover less expensive medications so that they can use their business skills to make money. There are many categories Insurance Companies place medications in, primarily for business reasons. Formulary, Non-formulary, Not covered, partially covered. Formulary is the list of medications the Insurance prefers to cover. Non-formulary are those they prefer not to pay for. If a drug is a Prior Authorization drug, that means it’s not on their formulary. That does not mean that the Insurance Company will not pay for the medication at all. It means they will only pay for the medication under certain circumstances. And, “prior” to the Insurance Company paying for the medication, they want to make sure it meets their criteria. This information they often want only from the Doctor, because they might want the diagnosis, certain tests run, or chart notes. These things can only come from the Doctor.Here is the process… you get a prescription from a Doctor, and the Pharmacy tries to bill it. The pharmacy gets a rejection saying this medication requires a Prior Authorization. Occasionally, there are cases where the pharmacy can put in a code. If that is possible, the Pharmacy just does this for the patient. More often than not, the Insurance Company wants the Doctor to submit information as to why the patient needs the medication prescribed, versus a medication on their formulary, which saves the Insurance Company money. The Pharmacy faxes or calls the Doctor’s office, letting them know to contact the Insurance Company, to find out the requirements for the Insurance Company to pay for the medication. If the patient fits the criteria, the Doctor faxes the information to the Insurance Company, and eventually, the medication gets paid for. If the patient does not fit the criteria, the Doctor usually has to change the medication to something the Insurance Company will pay for.You may notice, in this process, the Pharmacy is just an “errand boy”. The Insurance Company says the medication requires a Prior Authorization, they tell the pharmacy by rejecting to pay for the medication. Then, the Pharmacy tells the Doctor’s office. Then, it’s worked out one way or another between the Insurance Company & the Doctor’s office. Depending on how fast the Doctor acts, how much information the Insurance Company requires, and how fast the Insurance Company makes their decision, is what determines how quickly/slowly the prior authorization takes.An interesting tidbit in this whole process… if the Insurance Company approves the Prior Authorization (Meaning they will now pay for your medication), they do not call the Pharmacy to let them know that the medication has been approved, and the Pharmacy can rebill the Medication. Apparently, they are too busy to do this. The Doctor’s office doesn’t usually call the Pharmacy either. Apparently, they are too busy to do this. So, the patient’s medication is now covered, but neither of the two parties that know this, contacts the Pharmacy, so that they can rebill the medication and fill it. If the patient calls the Insurance Company or the Doctor’s Office… they usually say, oh yes, that was approved, I have no idea why the Pharmacy did not fill that medication, and call you to let you know! Then, the customer calls the Pharmacy or comes in, and yells at someone in the Pharmacy.Of course, the Pharmacy never knew this, because nobody called them. But, nobody cares about that, because the patient gets to vent their irritation, even if it’s at the wrong people. Obviously, this is a simplified version of the whole process. It’s probably more than you needed to know. But, this is a situation that’s all too common for people in Pharmacy. Getting the fuzzy end of the lollipop.
Create this form in 5 minutes!
How to create an eSignature for the ohio medicaid prior authorization form
How to generate an electronic signature for the Ohio Medicaid Prior Authorization Form in the online mode
How to make an eSignature for the Ohio Medicaid Prior Authorization Form in Google Chrome
How to create an electronic signature for signing the Ohio Medicaid Prior Authorization Form in Gmail
How to create an electronic signature for the Ohio Medicaid Prior Authorization Form straight from your smart phone
How to generate an electronic signature for the Ohio Medicaid Prior Authorization Form on iOS
How to create an eSignature for the Ohio Medicaid Prior Authorization Form on Android devices
People also ask
-
What is the Gainwell prior auth form?
The Gainwell prior auth form is a document utilized to obtain prior authorization for certain medical services. This form ensures that necessary approvals are secured before patient care begins, streamlining the healthcare process and enhancing patient outcomes.
-
How can airSlate SignNow assist with the Gainwell prior auth form?
airSlate SignNow allows users to easily create, send, and eSign the Gainwell prior auth form. With its user-friendly platform, you can quickly streamline the approval process, reduce paperwork, and improve efficiency in getting the necessary authorizations.
-
Is there a cost associated with using airSlate SignNow for the Gainwell prior auth form?
airSlate SignNow offers various pricing plans that cater to different business needs, including options for efficiently managing the Gainwell prior auth form. You can start with a free trial to explore its features before committing to a plan that suits your requirements.
-
What features does airSlate SignNow provide for handling the Gainwell prior auth form?
airSlate SignNow provides features such as document templates, secure eSigning, and real-time tracking for the Gainwell prior auth form. These features enhance the signing process and make it easy to manage all necessary documentation efficiently.
-
Are there integrations available for the Gainwell prior auth form with airSlate SignNow?
Yes, airSlate SignNow supports various integrations with popular business applications. This allows for seamless workflows when filling out and processing the Gainwell prior auth form, simplifying the healthcare authorization process.
-
How secure is the airSlate SignNow platform when using the Gainwell prior auth form?
The airSlate SignNow platform is designed with top-notch security features to protect sensitive data associated with the Gainwell prior auth form. With encryption and compliance with regulatory standards, your documents and patient information remain secure.
-
Can multiple users collaborate on the Gainwell prior auth form using airSlate SignNow?
Absolutely! airSlate SignNow enables collaboration among multiple users when working on the Gainwell prior auth form. This feature ensures that healthcare providers can efficiently communicate and finalize the documentation needed for prior authorization.
Get more for Ohio Medicaid Pa Form
- C 21 front rev form
- State of alabama eforms fill online printable fillable
- Cases dockets and filings in alabamajustia dockets form
- Consumer credit act alabama state banking department form
- Form c 24d rev
- Alabama circuit courts wikipedia form
- In the court of alabama form
- For unlawful detainer alabama administrative office of courts form
Find out other Ohio Medicaid Pa Form
- eSign Iowa Legal Separation Agreement Easy
- How To eSign New Jersey Life Sciences LLC Operating Agreement
- eSign Tennessee Insurance Rental Lease Agreement Later
- eSign Texas Insurance Affidavit Of Heirship Myself
- Help Me With eSign Kentucky Legal Quitclaim Deed
- eSign Louisiana Legal Limited Power Of Attorney Online
- How Can I eSign Maine Legal NDA
- eSign Maryland Legal LLC Operating Agreement Safe
- Can I eSign Virginia Life Sciences Job Description Template
- eSign Massachusetts Legal Promissory Note Template Safe
- eSign West Virginia Life Sciences Agreement Later
- How To eSign Michigan Legal Living Will
- eSign Alabama Non-Profit Business Plan Template Easy
- eSign Mississippi Legal Last Will And Testament Secure
- eSign California Non-Profit Month To Month Lease Myself
- eSign Colorado Non-Profit POA Mobile
- How Can I eSign Missouri Legal RFP
- eSign Missouri Legal Living Will Computer
- eSign Connecticut Non-Profit Job Description Template Now
- eSign Montana Legal Bill Of Lading Free