Ohio Medicaid Pa Form


What is the Ohio Medicaid Prior Authorization Form?
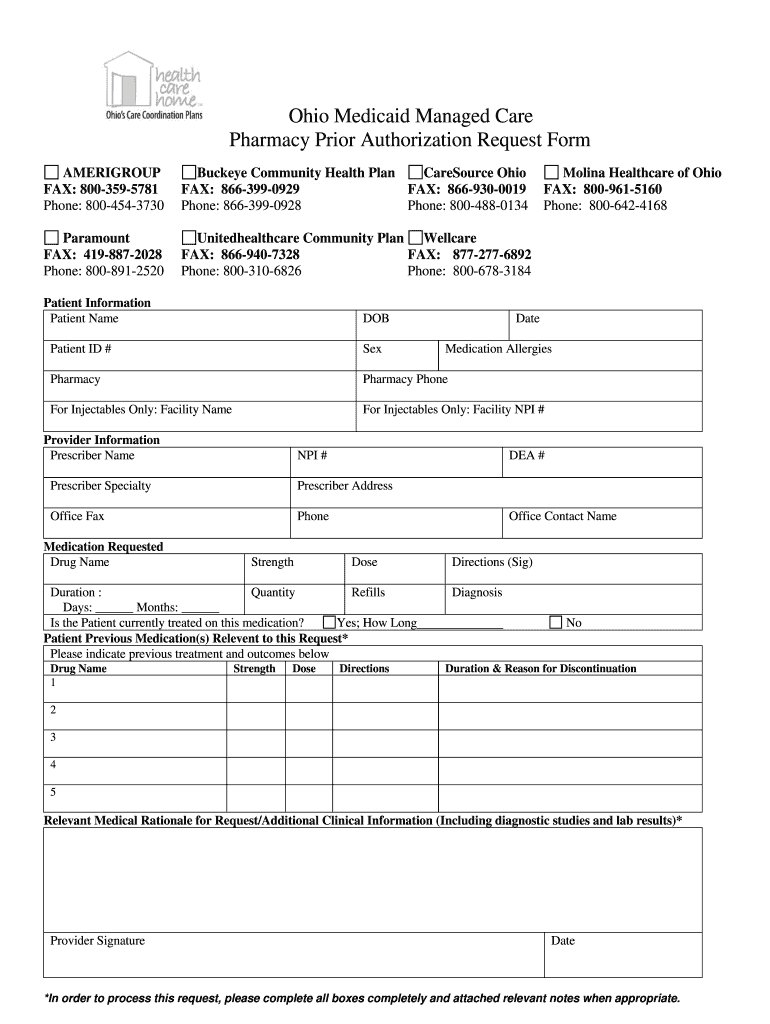
The Ohio Medicaid Prior Authorization Form, commonly referred to as the gainwell prior auth form, is a critical document used to obtain approval for specific medical services, treatments, or medications under the Ohio Medicaid program. This form ensures that the requested services are medically necessary and meet the criteria set by Medicaid. It is essential for healthcare providers to complete this form accurately to facilitate timely access to necessary care for their patients.
How to Use the Ohio Medicaid Prior Authorization Form
Using the Ohio Medicaid Prior Authorization Form involves several key steps. First, healthcare providers must gather all relevant patient information, including medical history and the specific services being requested. Next, the provider fills out the form, ensuring that all sections are completed accurately. Once completed, the form is submitted to the appropriate Medicaid office for review. Providers should keep a copy of the submitted form for their records and follow up on the status of the authorization.
Steps to Complete the Ohio Medicaid Prior Authorization Form
Completing the Ohio Medicaid Prior Authorization Form requires attention to detail. Here are the steps to follow:
- Gather patient information, including name, Medicaid number, and date of birth.
- Document the specific services, treatments, or medications being requested.
- Provide clinical justification for the request, including relevant medical history and documentation.
- Complete all required sections of the form, ensuring clarity and accuracy.
- Submit the form through the designated method, whether online, by mail, or in person.
Key Elements of the Ohio Medicaid Prior Authorization Form
The Ohio Medicaid Prior Authorization Form contains several key elements that must be included for successful processing. These elements include:
- Patient identification details, such as name and Medicaid ID.
- Provider information, including name, contact details, and NPI number.
- Description of the requested service or medication.
- Clinical rationale supporting the necessity of the request.
- Signature of the provider certifying the accuracy of the information provided.
Legal Use of the Ohio Medicaid Prior Authorization Form
The legal use of the Ohio Medicaid Prior Authorization Form is governed by state and federal regulations. It is crucial that healthcare providers adhere to these regulations to ensure compliance and avoid potential penalties. The form must be used solely for its intended purpose—seeking authorization for medically necessary services. Misuse of the form can result in legal consequences, including fines or loss of Medicaid privileges.
Form Submission Methods
The Ohio Medicaid Prior Authorization Form can be submitted through various methods to accommodate different provider preferences. These methods include:
- Online submission via the Ohio Medicaid portal.
- Mailing the completed form to the designated Medicaid office.
- In-person submission at local Medicaid offices.
Quick guide on how to complete ohio medicaid prior authorization form
Explore the simpler method for managing your Ohio Medicaid Pa Form
The traditional techniques for finalizing and endorsing documents consume an excessive amount of time compared to modern document management systems. You used to hunt for appropriate printed forms, produce hard copies, fill in all the information, and mail them. Nowadays, you can acquire, fill out, and sign your Ohio Medicaid Pa Form all in a single web browser tab with airSlate SignNow. Completing your Ohio Medicaid Pa Form has never been easier.
Steps to finalize your Ohio Medicaid Pa Form using airSlate SignNow
- Access the relevant category page and find your state-specific Ohio Medicaid Pa Form. Alternatively, utilize the search bar.
- Verify that the version of the form is accurate by previewing it.
- Click Get form to enter editing mode.
- Fill in your document with the required information using the editing features.
- Inspect the entered information and click the Sign tool to endorse your form.
- Select the most suitable method to create your signature: generate it, draw your signature, or upload an image of it.
- Click DONE to confirm changes.
- Download the document to your device or continue to Sharing settings for electronic distribution.
Efficient online platforms like airSlate SignNow ease the process of completing and submitting your forms. Give it a try to discover how quick document management and approval processes are meant to be. You will save a signNow amount of time.
Create this form in 5 minutes or less
FAQs
-
Why would a doctor send a prescription to a pharmacy, but not respond to repeated requests from the pharmacy to fill out a faxed prior authorization form?
Filling out a prior authorization is not a requirement of our practice. Most of us do this to help our patients, and it is sometimes taken for granted.Think about it. It is your insurance company that is requesting us to fill out this form, taking time away from actually treating patients, to help you save money on your medications. We understand that, and usually do our best to take care of them, but unless we have a large practice, with someone actually paid to spend all their time doing these PA’s, we have to carve out more time from our day to fill out paperwork.It’s also possible, although not likely, that the pharmacy does not have the correct fax number, the faxes have been misplaced, the doctor has some emergencies and is running behind, went on vacation, and so on.Paperwork and insurance requests have become more and more burdensome on our practices, not due to anything on the part of our patients, but a major hassle none the less.
-
How can I fill out the authorization form in Wipro's synergy?
By authorisation form I assume that you mean LOA. Just download the pdf and sign it with stylus or get a printout,sign it and scan the copy.Now upload it!If I my assumption is wrong please provide little clear picture!Thank you!Allah maalik!
-
Do we have to fill out an application form to US universities one year prior to admission?
The college application season for Fall 2019 opens in August 2018. Different colleges have different application timelines and deadlines. Find the requirements for the colleges on your list by googling “college name freshman application deadline”.
-
What does the authorization form in Wipro’s Synergy need to be filled out?
I don't exactly remember how the form was looking like in synergy portal. But I hope it is Authorizing Wipro to do background verification on all the details provided by candidate. It needs your name and signature with date.
-
Why do pharmacies need "prior authorization" to fill some prescriptions? Is the prescription itself not enough? What is prior authorization?
This is a fun answer. FIRST, Pharmacies never require prior authorizations. Do you know why? Because pharmacies don’t pay for your medication, they sell you your medications. Who, besides you, pays for your medications? That’s right, your Insurance Company. It’s completely wrong to think any Pharmacy is holding up your prescription because of a Prior Auth. Pharmacies bill in real time. Unlike Doctors offices. Doctors collect payments on the expected charge. And, if that’s wrong, they ask for more money. And, if you don’t pay them, they send your bill to collections. Pharmacies don’t utilize collection agencies. They bill in real time. That’s why people have to wait for their prescriptions, because the pharmacy has to get the billing absolutely correct at the time of service or else the Pharmacy loses money. Somebody, I don’t know who, decided it was the Pharmacies responsibility to make sure the Patient’s Insurance pays for the Patient’s medications that the Doctor prescribed. In the prior authorization process, pharmacies have essentially nothing to do with any of it, except get yelled at by angry customers.Here’s the breakdown. Insurance companies are still businesses. They are in the business of making money. To keep deductibles affordable, they can not cover every medication. So, they make what is called a formulary. Which are the medications the Insurance Company prefers to cover. This gives the Insurance company wiggle room to make money. It allows them to work contracts with drug companies, and to cover less expensive medications so that they can use their business skills to make money. There are many categories Insurance Companies place medications in, primarily for business reasons. Formulary, Non-formulary, Not covered, partially covered. Formulary is the list of medications the Insurance prefers to cover. Non-formulary are those they prefer not to pay for. If a drug is a Prior Authorization drug, that means it’s not on their formulary. That does not mean that the Insurance Company will not pay for the medication at all. It means they will only pay for the medication under certain circumstances. And, “prior” to the Insurance Company paying for the medication, they want to make sure it meets their criteria. This information they often want only from the Doctor, because they might want the diagnosis, certain tests run, or chart notes. These things can only come from the Doctor.Here is the process… you get a prescription from a Doctor, and the Pharmacy tries to bill it. The pharmacy gets a rejection saying this medication requires a Prior Authorization. Occasionally, there are cases where the pharmacy can put in a code. If that is possible, the Pharmacy just does this for the patient. More often than not, the Insurance Company wants the Doctor to submit information as to why the patient needs the medication prescribed, versus a medication on their formulary, which saves the Insurance Company money. The Pharmacy faxes or calls the Doctor’s office, letting them know to contact the Insurance Company, to find out the requirements for the Insurance Company to pay for the medication. If the patient fits the criteria, the Doctor faxes the information to the Insurance Company, and eventually, the medication gets paid for. If the patient does not fit the criteria, the Doctor usually has to change the medication to something the Insurance Company will pay for.You may notice, in this process, the Pharmacy is just an “errand boy”. The Insurance Company says the medication requires a Prior Authorization, they tell the pharmacy by rejecting to pay for the medication. Then, the Pharmacy tells the Doctor’s office. Then, it’s worked out one way or another between the Insurance Company & the Doctor’s office. Depending on how fast the Doctor acts, how much information the Insurance Company requires, and how fast the Insurance Company makes their decision, is what determines how quickly/slowly the prior authorization takes.An interesting tidbit in this whole process… if the Insurance Company approves the Prior Authorization (Meaning they will now pay for your medication), they do not call the Pharmacy to let them know that the medication has been approved, and the Pharmacy can rebill the Medication. Apparently, they are too busy to do this. The Doctor’s office doesn’t usually call the Pharmacy either. Apparently, they are too busy to do this. So, the patient’s medication is now covered, but neither of the two parties that know this, contacts the Pharmacy, so that they can rebill the medication and fill it. If the patient calls the Insurance Company or the Doctor’s Office… they usually say, oh yes, that was approved, I have no idea why the Pharmacy did not fill that medication, and call you to let you know! Then, the customer calls the Pharmacy or comes in, and yells at someone in the Pharmacy.Of course, the Pharmacy never knew this, because nobody called them. But, nobody cares about that, because the patient gets to vent their irritation, even if it’s at the wrong people. Obviously, this is a simplified version of the whole process. It’s probably more than you needed to know. But, this is a situation that’s all too common for people in Pharmacy. Getting the fuzzy end of the lollipop.
Create this form in 5 minutes!
How to create an eSignature for the ohio medicaid prior authorization form
How to generate an electronic signature for the Ohio Medicaid Prior Authorization Form in the online mode
How to make an eSignature for the Ohio Medicaid Prior Authorization Form in Google Chrome
How to create an electronic signature for signing the Ohio Medicaid Prior Authorization Form in Gmail
How to create an electronic signature for the Ohio Medicaid Prior Authorization Form straight from your smart phone
How to generate an electronic signature for the Ohio Medicaid Prior Authorization Form on iOS
How to create an eSignature for the Ohio Medicaid Prior Authorization Form on Android devices
People also ask
-
What is the Ohio Medicaid Pa Form and how can airSlate SignNow help?
The Ohio Medicaid Pa Form is a crucial document used for prior authorization requests in Ohio's Medicaid program. With airSlate SignNow, you can easily fill out and eSign the Ohio Medicaid Pa Form online, ensuring a seamless and efficient submission process. Our platform simplifies the management of these forms, saving you time and reducing paperwork.
-
How does airSlate SignNow ensure the security of my Ohio Medicaid Pa Form?
AirSlate SignNow takes data security seriously, especially when handling sensitive documents like the Ohio Medicaid Pa Form. We utilize advanced encryption protocols and compliance with industry standards to ensure that your information remains secure during transmission and storage. You can trust that your Ohio Medicaid Pa Form is protected at all times.
-
Is there a cost associated with using airSlate SignNow for the Ohio Medicaid Pa Form?
Yes, airSlate SignNow offers flexible pricing plans that cater to different business needs. You can choose a plan that best fits your requirements for managing the Ohio Medicaid Pa Form and other documents. Our cost-effective solutions ensure you get the best value for your eSigning and document management needs.
-
Can I integrate airSlate SignNow with other software for handling the Ohio Medicaid Pa Form?
Absolutely! AirSlate SignNow provides seamless integrations with various applications, making it easier to manage the Ohio Medicaid Pa Form alongside your existing workflows. Whether you're using CRM systems, document storage solutions, or other software, our platform can enhance your productivity and streamline your processes.
-
What features does airSlate SignNow offer for managing the Ohio Medicaid Pa Form?
AirSlate SignNow includes features like customizable templates, real-time tracking, and automatic reminders to help you manage the Ohio Medicaid Pa Form efficiently. You can create templates for repetitive use, track the status of your submissions, and receive notifications to ensure nothing slips through the cracks.
-
How can airSlate SignNow improve the submission process for the Ohio Medicaid Pa Form?
Using airSlate SignNow simplifies the submission process for the Ohio Medicaid Pa Form by allowing you to complete and eSign documents digitally. This eliminates the need for printing and mailing, reducing delays and mistakes. With our platform, you can submit your forms quickly and receive confirmation of receipt, ensuring prompt processing.
-
Is airSlate SignNow user-friendly for completing the Ohio Medicaid Pa Form?
Yes, airSlate SignNow is designed with user experience in mind. Our intuitive interface makes it easy for anyone to navigate and complete the Ohio Medicaid Pa Form without prior technical knowledge. We provide guides and customer support to assist you in getting started quickly and efficiently.
Get more for Ohio Medicaid Pa Form
- C 21 front rev form
- State of alabama eforms fill online printable fillable
- Cases dockets and filings in alabamajustia dockets form
- Consumer credit act alabama state banking department form
- Form c 24d rev
- Alabama circuit courts wikipedia form
- In the court of alabama form
- For unlawful detainer alabama administrative office of courts form
Find out other Ohio Medicaid Pa Form
- eSign Arizona Notice of Intent to Vacate Easy
- eSign Louisiana Notice of Rent Increase Mobile
- eSign Washington Notice of Rent Increase Computer
- How To eSign Florida Notice to Quit
- How To eSign Hawaii Notice to Quit
- eSign Montana Pet Addendum to Lease Agreement Online
- How To eSign Florida Tenant Removal
- How To eSign Hawaii Tenant Removal
- eSign Hawaii Tenant Removal Simple
- eSign Arkansas Vacation Rental Short Term Lease Agreement Easy
- Can I eSign North Carolina Vacation Rental Short Term Lease Agreement
- eSign Michigan Escrow Agreement Now
- eSign Hawaii Sales Receipt Template Online
- eSign Utah Sales Receipt Template Free
- eSign Alabama Sales Invoice Template Online
- eSign Vermont Escrow Agreement Easy
- How Can I eSign Wisconsin Escrow Agreement
- How To eSign Nebraska Sales Invoice Template
- eSign Nebraska Sales Invoice Template Simple
- eSign New York Sales Invoice Template Now