Soap Format for Progress Notes


What is the soap format for progress notes
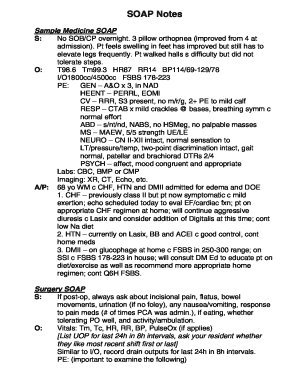
The soap format is a structured method used for documenting patient progress in a clear and organized manner. It stands for Subjective, Objective, Assessment, and Plan. This format allows healthcare professionals to capture essential information about a patient's condition and treatment in a way that is easily understood by other providers. Each section serves a specific purpose:
- Subjective: This section includes the patient's own words regarding their symptoms, feelings, and concerns.
- Objective: Here, healthcare providers document measurable data, such as vital signs, physical exam findings, and laboratory results.
- Assessment: This part involves the provider's clinical judgment based on the subjective and objective information gathered.
- Plan: The final section outlines the proposed treatment plan, including medications, referrals, and follow-up appointments.
How to use the soap format for progress notes
Using the soap format for progress notes involves following a systematic approach to ensure all relevant information is captured. Begin by gathering the patient's history and current complaints. In the subjective section, write down direct quotes from the patient to reflect their perspective. Next, collect objective data through examinations and tests, documenting findings accurately.
In the assessment section, synthesize the subjective and objective data to formulate a clinical impression. Finally, in the plan section, detail the next steps in the patient's care, including any tests to be ordered, treatments to be initiated, and educational points to discuss with the patient. This structured approach enhances communication and continuity of care.
Key elements of the soap format for progress notes
Each element of the soap format plays a critical role in creating comprehensive progress notes. The key elements include:
- Subjective: Patient-reported symptoms and concerns.
- Objective: Clinically observed data and measurable findings.
- Assessment: Clinical interpretation and diagnosis.
- Plan: Treatment strategy and follow-up care.
Incorporating these elements ensures that the notes are thorough and facilitate effective communication among healthcare providers.
Steps to complete the soap format for progress notes
Completing the soap format for progress notes involves several steps:
- Gather patient information, including history and current symptoms.
- Document the subjective section with the patient's own words.
- Record objective findings from examinations and tests.
- Analyze the information to form an assessment.
- Outline the plan for treatment and follow-up care.
By following these steps, healthcare professionals can create effective and informative progress notes that support patient care.
Legal use of the soap format for progress notes
The legal use of the soap format for progress notes is crucial in ensuring that documentation meets regulatory standards. Properly completed soap notes can serve as legal evidence in cases of disputes or audits. It is essential to maintain accuracy and clarity in each section, as any ambiguity may lead to misunderstandings or legal challenges.
Additionally, compliance with relevant laws and regulations, such as HIPAA, is vital to protect patient privacy and confidentiality. Ensuring that notes are securely stored and only accessible to authorized personnel is also an important aspect of legal documentation.
Examples of using the soap format for progress notes
Examples of using the soap format can help illustrate its application in real-world scenarios. For instance, consider a patient presenting with chest pain:
- Subjective: "I have been experiencing sharp chest pain for the last two hours."
- Objective: Vital signs: BP 130/80, HR 88, Respiratory rate 18. ECG shows normal sinus rhythm.
- Assessment: Possible angina; further evaluation needed.
- Plan: Order cardiac enzymes, schedule a stress test, and provide patient education on lifestyle modifications.
Such examples can guide healthcare professionals in effectively documenting patient encounters using the soap format.
Quick guide on how to complete soap format for progress notes
Streamline Soap Format For Progress Notes effortlessly on any device
Digital document management has become increasingly popular among businesses and individuals. It offers a seamless environmentally friendly alternative to conventional printed and signed documents, enabling you to locate the appropriate form and securely store it online. airSlate SignNow equips you with all the tools necessary to create, modify, and electronically sign your documents quickly and without delays. Manage Soap Format For Progress Notes on any device using airSlate SignNow’s Android or iOS applications and enhance any document-driven process today.
The simplest way to modify and electronically sign Soap Format For Progress Notes with ease
- Obtain Soap Format For Progress Notes and click on Get Form to initiate the process.
- Utilize the tools we offer to complete your form.
- Identify signNow parts of the documents or obscure confidential information with tools provided by airSlate SignNow specifically for this purpose.
- Craft your signature with the Sign tool, which takes a matter of seconds and holds the same legal validity as a traditional ink signature.
- Review the information and click on the Done button to save your modifications.
- Choose your preferred method of sending your form, via email, text message (SMS), or invitation link, or download it to your computer.
Eliminate concerns about lost or misfiled documents, tedious form searching, or mistakes that necessitate printing new document copies. airSlate SignNow addresses all your document management needs in just a few clicks from any device you select. Edit and electronically sign Soap Format For Progress Notes to guarantee excellent communication at every step of your form preparation process with airSlate SignNow.
Create this form in 5 minutes or less
Create this form in 5 minutes!
How to create an eSignature for the soap format for progress notes
How to create an electronic signature for a PDF online
How to create an electronic signature for a PDF in Google Chrome
How to create an e-signature for signing PDFs in Gmail
How to create an e-signature right from your smartphone
How to create an e-signature for a PDF on iOS
How to create an e-signature for a PDF on Android
People also ask
-
What is soap narrative ems in the context of airSlate SignNow?
Soap narrative ems refers to the structured documentation method used to capture and convey important information in the eSigning process. By utilizing this approach within airSlate SignNow, users can enhance their documentation practices, ensuring clarity and compliance.
-
How does airSlate SignNow integrate soap narrative ems?
AirSlate SignNow seamlessly integrates soap narrative ems into its workflow, allowing users to document interactions and signatures effectively. This integration simplifies the eSigning process while ensuring all necessary details are captured and organized for future reference.
-
What are the pricing options for airSlate SignNow's soap narrative ems features?
AirSlate SignNow offers competitive pricing for its suite of features, including those related to soap narrative ems. Users can choose from various plans based on their needs, ensuring they get the best value while leveraging powerful eSigning capabilities.
-
What benefits does soap narrative ems provide for businesses?
Implementing soap narrative ems in airSlate SignNow benefits businesses by improving documentation accuracy and enhancing communication. This approach allows teams to maintain clear records and accountability, ultimately streamlining operations and reducing errors.
-
Are there any integrations available with soap narrative ems in airSlate SignNow?
Yes, airSlate SignNow supports various integrations that complement soap narrative ems functionalities. This enables users to connect their eSigning processes with other business tools, facilitating a more cohesive and efficient experience across platforms.
-
How can soap narrative ems improve compliance in document signing?
Soap narrative ems enhances compliance during the document signing process by providing a clear and detailed account of each interaction. This structured approach helps organizations meet regulatory standards and maintain proper documentation for audits and reviews.
-
Is training required to implement soap narrative ems with airSlate SignNow?
While airSlate SignNow is designed for ease of use, some training may enhance knowledge of soap narrative ems and its best practices. However, many users find the platform intuitive and can quickly adapt to utilizing soap narrative ems in their workflow without extensive training.
Get more for Soap Format For Progress Notes
Find out other Soap Format For Progress Notes
- eSignature Minnesota Sports Forbearance Agreement Online
- eSignature Oklahoma Real Estate Business Plan Template Free
- eSignature South Dakota Police Limited Power Of Attorney Online
- How To eSignature West Virginia Police POA
- eSignature Rhode Island Real Estate Letter Of Intent Free
- eSignature Rhode Island Real Estate Business Letter Template Later
- eSignature South Dakota Real Estate Lease Termination Letter Simple
- eSignature Tennessee Real Estate Cease And Desist Letter Myself
- How To eSignature New Mexico Sports Executive Summary Template
- Can I eSignature Utah Real Estate Operating Agreement
- eSignature Vermont Real Estate Warranty Deed Online
- eSignature Vermont Real Estate Operating Agreement Online
- eSignature Utah Real Estate Emergency Contact Form Safe
- eSignature Washington Real Estate Lease Agreement Form Mobile
- How Can I eSignature New York Sports Executive Summary Template
- eSignature Arkansas Courts LLC Operating Agreement Now
- How Do I eSignature Arizona Courts Moving Checklist
- eSignature Wyoming Real Estate Quitclaim Deed Myself
- eSignature Wyoming Real Estate Lease Agreement Template Online
- How Can I eSignature Delaware Courts Stock Certificate