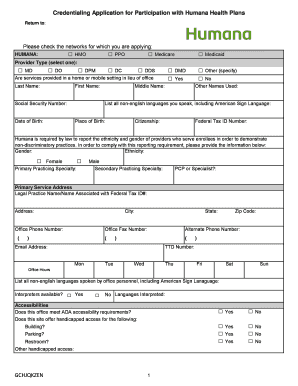
Credentialing Application for Participation with Humana Health Plans Form


What is the credentialing application for participation with Humana health plans
The credentialing application for participation with Humana health plans is a formal process that healthcare providers must complete to become part of Humana's network. This application is essential for providers seeking to offer services to Humana members. It involves providing detailed information about the provider’s qualifications, practice history, and any relevant certifications. Completing this application accurately is crucial for ensuring compliance with Humana’s standards and regulations.
Steps to complete the credentialing application for participation with Humana health plans
Completing the credentialing application involves several important steps:
- Gather necessary documentation, including licenses, certifications, and proof of malpractice insurance.
- Fill out the credentialing application form thoroughly, ensuring all information is accurate and up-to-date.
- Submit the application via the designated method, which may include online submission or mailing.
- Follow up with Humana to confirm receipt of the application and to inquire about the status of the review process.
Legal use of the credentialing application for participation with Humana health plans
The legal use of the credentialing application is governed by various regulations that ensure the integrity of the healthcare system. Providers must adhere to federal and state laws regarding patient privacy and data protection. Additionally, the application must be completed honestly, as any misrepresentation can lead to legal repercussions and denial of participation in Humana's network.
Required documents for the credentialing application
When applying for credentialing with Humana, several documents are typically required:
- Current state medical license or relevant professional license.
- Board certification documentation, if applicable.
- Proof of malpractice insurance coverage.
- Curriculum vitae detailing professional experience and education.
- Any additional credentials or certifications relevant to the provider's specialty.
How to obtain the credentialing application for participation with Humana health plans
Providers can obtain the credentialing application for participation with Humana health plans through several methods. The application is often available on Humana’s official website. Providers may also contact Humana's credentialing department directly for assistance. Additionally, some healthcare facilities may provide the application as part of their onboarding process for new providers.
Application process and approval time for Humana credentialing
The application process for Humana credentialing typically involves a review period during which Humana verifies the information provided. This process can take several weeks, depending on the completeness of the application and the volume of applications being processed. Providers are encouraged to ensure all documentation is accurate and submitted promptly to avoid delays in approval.
Quick guide on how to complete credentialing application for participation with humana health plans
Prepare Credentialing Application For Participation With Humana Health Plans effortlessly on any device
Digital document management has become favored by businesses and individuals alike. It offers a superb eco-friendly substitute to traditional printed and signed documents, as you can access the necessary form and securely store it online. airSlate SignNow equips you with all the tools required to create, edit, and eSign your documents swiftly without delays. Manage Credentialing Application For Participation With Humana Health Plans on any platform using airSlate SignNow's Android or iOS applications and enhance any document-centric procedure today.
The easiest method to edit and eSign Credentialing Application For Participation With Humana Health Plans without hassle
- Find Credentialing Application For Participation With Humana Health Plans and then click Get Form to begin.
- Utilize the tools we provide to fill out your form.
- Highlight important sections of the documents or obscure sensitive information with tools that airSlate SignNow offers specifically for that purpose.
- Generate your signature using the Sign tool, which takes mere seconds and carries the same legal validity as a conventional wet ink signature.
- Verify the details and then click the Done button to save your modifications.
- Select how you wish to share your form, through email, SMS, invitation link, or download it to your computer.
Eliminate concerns about missing or lost documents, tedious form searches, or errors that require printing new document copies. airSlate SignNow caters to all your document management needs in just a few clicks from any device of your choosing. Edit and eSign Credentialing Application For Participation With Humana Health Plans and ensure excellent communication at any stage of your document preparation process with airSlate SignNow.
Create this form in 5 minutes or less
Create this form in 5 minutes!
How to create an eSignature for the credentialing application for participation with humana health plans
How to create an electronic signature for a PDF online
How to create an electronic signature for a PDF in Google Chrome
How to create an e-signature for signing PDFs in Gmail
How to create an e-signature right from your smartphone
How to create an e-signature for a PDF on iOS
How to create an e-signature for a PDF on Android
People also ask
-
What is the Humana provider credentialing phone number?
The Humana provider credentialing phone number is a specific line to contact for inquiries related to provider enrollment and credentialing. It's essential for healthcare providers to know this number to facilitate communication and resolve credentialing issues efficiently.
-
How can I access the Humana provider credentialing phone number?
You can access the Humana provider credentialing phone number by visiting their official website. Typically, this contact information is located under the provider services or contact us sections, ensuring you have direct access for any inquiries.
-
What services are provided through Humana provider credentialing?
Humana provider credentialing services include evaluating and verifying healthcare practitioners' qualifications, ensuring compliance with safety and quality standards. By working with the Humana provider credentialing phone number, you can streamline your onboarding process and get necessary updates.
-
Is there a fee associated with Humana provider credentialing?
Generally, there is no fee for using the Humana provider credentialing services. However, various practices may have costs linked to the necessary documentation or additional services, which can be clarified by calling the Humana provider credentialing phone number.
-
What are the benefits of using Humana for credentialing?
Using Humana for credentialing can speed up the enrollment process, ensuring that your practice gets paid for services rendered without delays. It also provides a trusted framework for compliance, which can be further discussed if you signNow out through the Humana provider credentialing phone number.
-
Can the Humana provider credentialing process be completed online?
Yes, much of the Humana provider credentialing process can be completed online. Providers can submit their documentation and track the status of their credentials through the Humana portal, though you can also inquire about specific steps by calling the Humana provider credentialing phone number.
-
What documentation is required for Humana provider credentialing?
The required documentation for Humana provider credentialing generally includes professional license verification, proof of malpractice insurance, and educational credentials. For a complete checklist or further assistance, you can contact the Humana provider credentialing phone number.
Get more for Credentialing Application For Participation With Humana Health Plans
- Contractor warranty template form
- Construction project closeout checklist template form
- Maverest dental network form
- Optus billing services form
- Six flags permission slip form
- Articles of incorporation and bylaws of dairy farmers of america inc form
- Equi vest annuity formsequitable
- Refusal of medical treatment media services form
Find out other Credentialing Application For Participation With Humana Health Plans
- Help Me With eSign Iowa Insurance Living Will
- eSign North Dakota Lawers Quitclaim Deed Easy
- eSign Ohio Lawers Agreement Computer
- eSign North Dakota Lawers Separation Agreement Online
- How To eSign North Dakota Lawers Separation Agreement
- eSign Kansas Insurance Moving Checklist Free
- eSign Louisiana Insurance Promissory Note Template Simple
- eSign Texas Lawers Contract Fast
- eSign Texas Lawers Lease Agreement Free
- eSign Maine Insurance Rental Application Free
- How Can I eSign Maryland Insurance IOU
- eSign Washington Lawers Limited Power Of Attorney Computer
- eSign Wisconsin Lawers LLC Operating Agreement Free
- eSign Alabama Legal Quitclaim Deed Online
- eSign Alaska Legal Contract Safe
- How To eSign Alaska Legal Warranty Deed
- eSign Alaska Legal Cease And Desist Letter Simple
- eSign Arkansas Legal LLC Operating Agreement Simple
- eSign Alabama Life Sciences Residential Lease Agreement Fast
- How To eSign Arkansas Legal Residential Lease Agreement