Out of Network Claim Form for Members Penn Behavioral Health 2016-2026


What is the Out Of Network Claim Form For Members Penn Behavioral Health
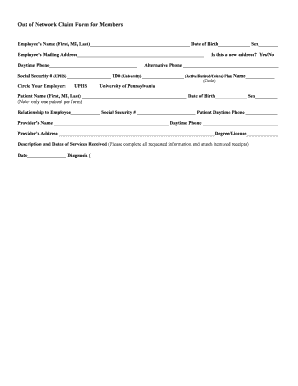
The Out Of Network Claim Form for Members Penn Behavioral Health is a document used by members seeking reimbursement for mental health services received from providers who are not part of the Penn Behavioral Health network. This form allows members to submit claims for services that may not be covered under their standard plan, enabling them to potentially recover some of their out-of-pocket expenses. It is essential for members to understand the details of their insurance coverage, as reimbursement amounts may vary based on the specifics of their policy.
How to obtain the Out Of Network Claim Form For Members Penn Behavioral Health
Members can obtain the Out Of Network Claim Form for Members Penn Behavioral Health through several methods. The form is typically available on the official Penn Behavioral Health website, where members can download it directly. Additionally, members may contact customer service for assistance in acquiring the form. It is advisable to ensure that the most current version of the form is being utilized to avoid any processing delays.
Steps to complete the Out Of Network Claim Form For Members Penn Behavioral Health
Completing the Out Of Network Claim Form requires careful attention to detail. Members should follow these steps:
- Begin by filling out personal information, including name, address, and member ID.
- Provide details about the out-of-network provider, including their name, address, and tax ID number.
- List the services received, including dates of service and the type of treatment.
- Attach any necessary documentation, such as receipts or invoices from the provider.
- Sign and date the form to certify that the information provided is accurate.
Once completed, the form should be submitted according to the instructions provided, either online or by mail.
Required Documents
When submitting the Out Of Network Claim Form, members must include specific documents to support their claim. These typically include:
- Receipts or invoices from the out-of-network provider detailing the services rendered.
- Any relevant medical records or treatment notes that may be necessary for processing the claim.
- Proof of payment, such as credit card statements or canceled checks, to confirm the member's out-of-pocket expenses.
Ensuring that all required documents are included can help expedite the claims process and improve the chances of reimbursement.
Form Submission Methods
Members have several options for submitting the Out Of Network Claim Form. These methods include:
- Online Submission: Members can often submit their claims electronically through the Penn Behavioral Health member portal.
- Mail Submission: The completed form and supporting documents can be mailed to the designated claims address provided on the form.
- In-Person Submission: Some members may choose to deliver the form in person at a local office, if available.
Choosing the appropriate submission method can depend on personal preference and the urgency of the claim.
Eligibility Criteria
To utilize the Out Of Network Claim Form, members must meet specific eligibility criteria. Generally, these criteria include:
- Being an active member of Penn Behavioral Health with a valid insurance policy.
- Receiving services from a provider who is not part of the Penn Behavioral Health network.
- Having a policy that allows for out-of-network reimbursements, as some plans may have restrictions.
Members should review their policy details to confirm eligibility before submitting a claim.
Quick guide on how to complete out of network claim form for members penn behavioral health
Complete Out Of Network Claim Form For Members Penn Behavioral Health seamlessly on any device
Digital document management has gained traction among businesses and individuals. It offers an ideal eco-friendly substitute to conventional printed and signed documents, allowing you to find the suitable form and securely store it online. airSlate SignNow equips you with all the tools necessary to create, edit, and eSign your documents swiftly without delays. Handle Out Of Network Claim Form For Members Penn Behavioral Health on any device using airSlate SignNow Android or iOS applications and streamline any document-related process today.
How to modify and eSign Out Of Network Claim Form For Members Penn Behavioral Health effortlessly
- Find Out Of Network Claim Form For Members Penn Behavioral Health and click Get Form to begin.
- Make use of the tools we provide to complete your form.
- Emphasize pertinent sections of your documents or obscure confidential information with tools specifically designed by airSlate SignNow for that purpose.
- Generate your signature using the Sign feature, which takes seconds and carries the same legal validity as a traditional ink signature.
- Review all the details and click the Done button to save your changes.
- Select how you wish to submit your form, via email, SMS, or invitation link, or download it to your computer.
Eliminate concerns about lost or misplaced files, tedious form searches, or errors that necessitate printing new document copies. airSlate SignNow meets your document administration needs in just a few clicks from any device you choose. Edit and eSign Out Of Network Claim Form For Members Penn Behavioral Health and ensure excellent communication at any stage of your form preparation process with airSlate SignNow.
Create this form in 5 minutes or less
Find and fill out the correct out of network claim form for members penn behavioral health
Create this form in 5 minutes!
How to create an eSignature for the out of network claim form for members penn behavioral health
How to create an electronic signature for a PDF online
How to create an electronic signature for a PDF in Google Chrome
How to create an e-signature for signing PDFs in Gmail
How to create an e-signature right from your smartphone
How to create an e-signature for a PDF on iOS
How to create an e-signature for a PDF on Android
People also ask
-
What is the Out Of Network Claim Form For Members Penn Behavioral Health?
The Out Of Network Claim Form For Members Penn Behavioral Health is a document that allows members to request reimbursement for services received from out-of-network providers. This form is essential for ensuring that you can claim benefits for treatments not covered by your primary network.
-
How do I fill out the Out Of Network Claim Form For Members Penn Behavioral Health?
To fill out the Out Of Network Claim Form For Members Penn Behavioral Health, you need to provide your personal information, details about the services received, and any relevant receipts. Ensure that all sections are completed accurately to avoid delays in processing your claim.
-
What are the benefits of using the Out Of Network Claim Form For Members Penn Behavioral Health?
Using the Out Of Network Claim Form For Members Penn Behavioral Health allows you to access reimbursement for services that may not be covered by your in-network providers. This can signNowly reduce your out-of-pocket expenses and ensure you receive the care you need.
-
Is there a fee associated with submitting the Out Of Network Claim Form For Members Penn Behavioral Health?
There is typically no fee for submitting the Out Of Network Claim Form For Members Penn Behavioral Health. However, it’s important to check with your specific plan for any potential costs associated with processing claims.
-
How long does it take to process the Out Of Network Claim Form For Members Penn Behavioral Health?
Processing times for the Out Of Network Claim Form For Members Penn Behavioral Health can vary, but it generally takes between 2 to 4 weeks. To expedite the process, ensure that all required information is complete and accurate when submitting your claim.
-
Can I track the status of my Out Of Network Claim Form For Members Penn Behavioral Health?
Yes, you can track the status of your Out Of Network Claim Form For Members Penn Behavioral Health through your member portal. This feature allows you to stay updated on the progress of your claim and any additional information that may be required.
-
What should I do if my Out Of Network Claim Form For Members Penn Behavioral Health is denied?
If your Out Of Network Claim Form For Members Penn Behavioral Health is denied, you should review the denial notice for specific reasons. You can appeal the decision by providing additional documentation or clarification to support your claim.
Get more for Out Of Network Claim Form For Members Penn Behavioral Health
Find out other Out Of Network Claim Form For Members Penn Behavioral Health
- Can I Electronic signature Ohio Consumer Credit Application
- eSignature Georgia Junior Employment Offer Letter Later
- Electronic signature Utah Outsourcing Services Contract Online
- How To Electronic signature Wisconsin Debit Memo
- Electronic signature Delaware Junior Employment Offer Letter Later
- Electronic signature Texas Time Off Policy Later
- Electronic signature Texas Time Off Policy Free
- eSignature Delaware Time Off Policy Online
- Help Me With Electronic signature Indiana Direct Deposit Enrollment Form
- Electronic signature Iowa Overtime Authorization Form Online
- Electronic signature Illinois Employee Appraisal Form Simple
- Electronic signature West Virginia Business Ethics and Conduct Disclosure Statement Free
- Electronic signature Alabama Disclosure Notice Simple
- Electronic signature Massachusetts Disclosure Notice Free
- Electronic signature Delaware Drug Testing Consent Agreement Easy
- Electronic signature North Dakota Disclosure Notice Simple
- Electronic signature California Car Lease Agreement Template Free
- How Can I Electronic signature Florida Car Lease Agreement Template
- Electronic signature Kentucky Car Lease Agreement Template Myself
- Electronic signature Texas Car Lease Agreement Template Easy