Standard Prior Authorization Criteria Form


Understanding the Standard Prior Authorization Criteria
The Standard Prior Authorization Criteria serves as a guideline for healthcare providers and patients to ensure that specific medical services or medications are covered by insurance before they are provided. This process is essential in managing healthcare costs and ensuring that patients receive necessary treatments. The criteria typically include medical necessity, the appropriateness of the service, and alternative treatment options. Understanding these criteria can help streamline the authorization process and improve patient care.
Steps to Complete the Standard Prior Authorization Criteria
Completing the Standard Prior Authorization Criteria involves several key steps:
- Gather necessary patient information, including medical history and current treatments.
- Identify the specific service or medication requiring authorization.
- Review the insurance provider's criteria for the requested service.
- Complete the authorization form, ensuring all required fields are filled accurately.
- Submit the form through the appropriate channels, such as online portals or by mail.
- Follow up with the insurance provider to confirm receipt and status of the authorization request.
Legal Use of the Standard Prior Authorization Criteria
The legal use of the Standard Prior Authorization Criteria is crucial for compliance with healthcare regulations. It ensures that both providers and patients adhere to the established guidelines set forth by insurance companies and governmental regulations. Utilizing these criteria legally protects healthcare providers from potential liabilities and ensures that patients receive appropriate care based on their medical needs.
Eligibility Criteria for Standard Prior Authorization
Eligibility for Standard Prior Authorization typically depends on several factors, including:
- The specific insurance plan and its coverage policies.
- The type of service or medication being requested.
- Patient medical history and current health status.
- Compliance with any pre-existing conditions or treatment protocols.
Understanding these eligibility criteria can help patients and providers navigate the authorization process more effectively.
Required Documents for Standard Prior Authorization
When applying for Standard Prior Authorization, certain documents are generally required to support the request. These may include:
- Completed authorization request form.
- Patient's medical records relevant to the treatment.
- Documentation of previous treatments and outcomes.
- Any additional information requested by the insurance provider.
Having these documents ready can expedite the approval process and reduce delays in patient care.
Form Submission Methods for Standard Prior Authorization
There are various methods to submit the Standard Prior Authorization form, including:
- Online submission through the insurance provider’s portal.
- Mailing the completed form to the designated address.
- In-person submission at the insurance company’s local office.
Choosing the appropriate submission method can depend on urgency and the specific requirements of the insurance provider.
Quick guide on how to complete 2021 standard prior authorization criteria
Easily Prepare Standard Prior Authorization Criteria on Any Device
Digital document management has become prevalent among businesses and individuals. It serves as an excellent eco-friendly alternative to conventional printed and signed documents, allowing you to obtain the necessary form and securely store it online. airSlate SignNow provides you with all the tools required to create, edit, and eSign your documents swiftly without delays. Manage Standard Prior Authorization Criteria on any device with the airSlate SignNow apps for Android or iOS and streamline your document-related tasks today.
How to Edit and eSign Standard Prior Authorization Criteria Effortlessly
- Obtain Standard Prior Authorization Criteria and click on Get Form to begin.
- Utilize the tools we offer to complete your form.
- Emphasize important sections of your documents or obscure sensitive details with tools specifically designed for this purpose by airSlate SignNow.
- Create your eSignature using the Sign feature, which takes just moments and carries the same legal validity as a traditional wet ink signature.
- Review all the details and click on the Done button to save your changes.
- Choose how you wish to send your form—via email, SMS, invitation link, or download it to your computer.
Eliminate concerns over lost or misplaced documents, tedious form searching, or mistakes that necessitate printing new copies. airSlate SignNow meets all your document management needs with just a few clicks from any device you prefer. Modify and eSign Standard Prior Authorization Criteria to ensure excellent communication throughout every stage of the form preparation process with airSlate SignNow.
Create this form in 5 minutes or less
Create this form in 5 minutes!
People also ask
-
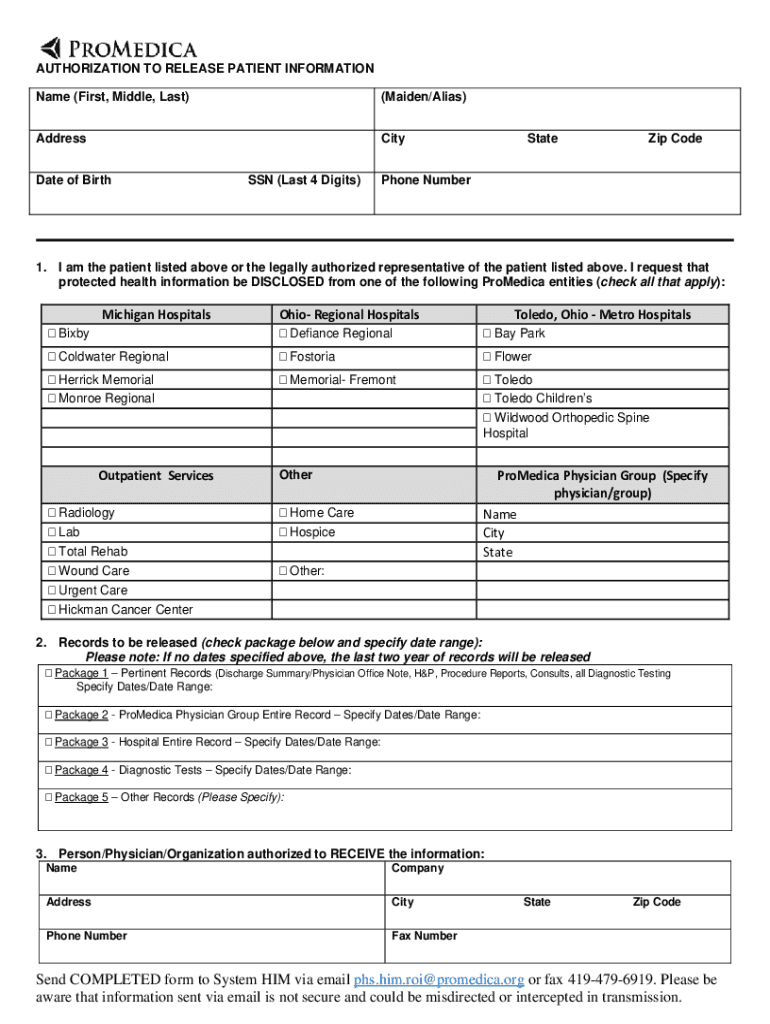
What is the promedica release patient form?
The promedica release patient form is a document used to authorize the release of a patient's medical information. It simplifies the process of obtaining necessary consents, ensuring compliance with privacy laws while delivering critical information quickly. Using airSlate SignNow, you can create, share, and eSign this form easily.
-
How does airSlate SignNow facilitate the promedica release patient form?
airSlate SignNow streamlines the process of managing the promedica release patient form by allowing users to create templates and automate workflows. You can customize the form to fit your specific needs and ensure it adheres to legal requirements. This efficiency helps healthcare providers save time and reduce administrative burdens.
-
Is there a cost associated with using airSlate SignNow for the promedica release patient form?
Yes, there is a cost associated with using airSlate SignNow, but it is designed to be a cost-effective solution for businesses. Pricing plans vary based on features and usage, ensuring you only pay for what you need. You can get started with a free trial to assess whether airSlate SignNow meets your needs for the promedica release patient form.
-
What features does airSlate SignNow offer for the promedica release patient form?
airSlate SignNow provides several key features for the promedica release patient form, including electronic signatures, document templates, and tracking capabilities. You can easily customize your form and automate notifications for recipients, ensuring a seamless process. Additionally, the platform supports integration with other tools, making it a versatile option for healthcare professionals.
-
How can the promedica release patient form benefit healthcare providers?
The promedica release patient form benefits healthcare providers by streamlining the process of obtaining patient consent for information sharing. This not only improves efficiency but also enhances patient trust and satisfaction. By using airSlate SignNow, providers can ensure that their documentation is both compliant and easily accessible.
-
Can I integrate airSlate SignNow with other software for managing the promedica release patient form?
Yes, airSlate SignNow offers integrations with various software solutions, including CRM and practice management systems. This means you can easily manage the promedica release patient form alongside your other critical business processes. Such integrations enhance workflow efficiency and data accuracy.
-
How secure is the promedica release patient form when using airSlate SignNow?
Security is a top priority with airSlate SignNow, especially when handling sensitive documents like the promedica release patient form. The platform employs advanced encryption and adheres to compliance standards to protect patient information. This ensures that your documents remain confidential and secure.
Get more for Standard Prior Authorization Criteria
- Deed real estate contract form
- Landlord notice rent 497429612 form
- Deed real estate 497429613 form
- Letter from tenant to landlord about sexual harassment washington form
- Real estate contract form
- Letter from tenant to landlord about fair housing reduction or denial of services to family with children washington form
- Deed and purchasers assignment of real estate contract with individual acknowledgment washington form
- Bargain deed form
Find out other Standard Prior Authorization Criteria
- How To Electronic signature Utah Courts Operating Agreement
- Electronic signature West Virginia Courts Quitclaim Deed Computer
- Electronic signature West Virginia Courts Quitclaim Deed Free
- Electronic signature Virginia Courts Limited Power Of Attorney Computer
- Can I Sign Alabama Banking PPT
- Electronic signature Washington Sports POA Simple
- How To Electronic signature West Virginia Sports Arbitration Agreement
- Electronic signature Wisconsin Sports Residential Lease Agreement Myself
- Help Me With Sign Arizona Banking Document
- How Do I Sign Arizona Banking Form
- How Can I Sign Arizona Banking Form
- How Can I Sign Arizona Banking Form
- Can I Sign Colorado Banking PPT
- How Do I Sign Idaho Banking Presentation
- Can I Sign Indiana Banking Document
- How Can I Sign Indiana Banking PPT
- How To Sign Maine Banking PPT
- Help Me With Sign Massachusetts Banking Presentation
- Can I Sign Michigan Banking PDF
- Can I Sign Michigan Banking PDF