Prior Authorization Benefit Form


What is the Prior Authorization Benefit Form
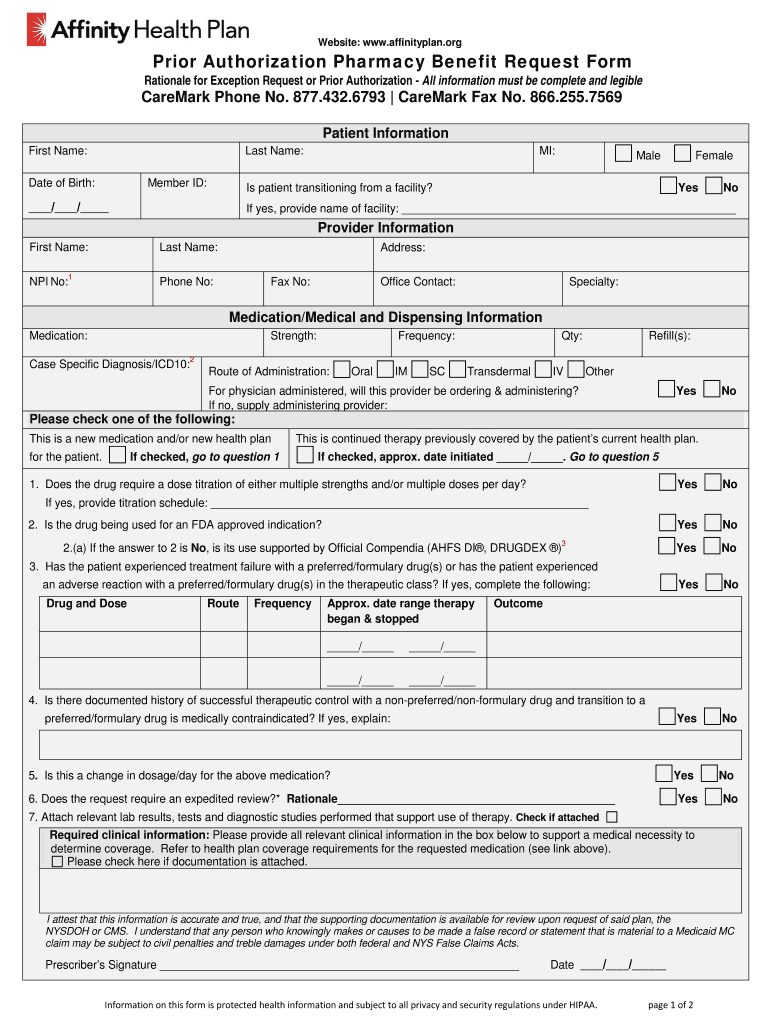
The Prior Authorization Benefit Form is a crucial document used by health plan pharmacies to determine whether a prescribed medication is covered under a patient's health insurance plan. This form is essential for ensuring that the patient receives the necessary medications while adhering to the coverage guidelines set by their health insurance provider. It outlines the specific medication requested, the patient's medical history, and the rationale for the prescription, allowing the pharmacy to assess eligibility for coverage.
How to use the Prior Authorization Benefit Form
Using the Prior Authorization Benefit Form involves several steps to ensure that the request is processed efficiently. First, the healthcare provider must complete the form with accurate details about the patient and the prescribed medication. Next, the completed form is submitted to the health plan pharmacy for review. The pharmacy will then evaluate the request based on the patient's insurance coverage and medical necessity. If approved, the patient can obtain their medication without incurring additional out-of-pocket costs.
Steps to complete the Prior Authorization Benefit Form
Completing the Prior Authorization Benefit Form requires careful attention to detail. Follow these steps:
- Gather necessary patient information, including full name, date of birth, and insurance details.
- Provide the prescribing physician's information, including their contact details and National Provider Identifier (NPI).
- Clearly state the medication name, dosage, and frequency of use.
- Include relevant medical history and any previous treatments related to the condition.
- Submit the form to the health plan pharmacy via the preferred submission method, such as online, by mail, or in person.
Legal use of the Prior Authorization Benefit Form
The legal use of the Prior Authorization Benefit Form is governed by regulations that ensure patient privacy and the integrity of the healthcare system. Compliance with the Health Insurance Portability and Accountability Act (HIPAA) is essential, as it protects sensitive patient information during the authorization process. Additionally, the form must be filled out accurately to avoid legal repercussions, such as denied claims or potential penalties for misrepresentation.
Required Documents
When submitting the Prior Authorization Benefit Form, certain documents may be required to support the request. These documents can include:
- Patient's insurance card to verify coverage.
- Medical records that provide evidence of the necessity for the prescribed medication.
- Previous treatment records or notes from the prescribing physician.
- Any other relevant documentation that may assist in the approval process.
Form Submission Methods
The Prior Authorization Benefit Form can be submitted through various methods, depending on the health plan pharmacy's requirements. Common submission methods include:
- Online submission through the health plan's secure portal.
- Mailing the completed form to the designated address provided by the health plan.
- In-person submission at the pharmacy or healthcare facility.
Eligibility Criteria
Eligibility for the Prior Authorization Benefit Form depends on several factors, including the patient's insurance plan, the specific medication requested, and the medical condition being treated. Typically, the following criteria must be met:
- The medication must be included in the patient's health plan formulary.
- The patient must have a documented medical need for the medication.
- Alternative treatments must have been considered or tried prior to the request.
Quick guide on how to complete prior authorization benefit form
Prepare Prior Authorization Benefit Form effortlessly on any gadget
Digital document management has gained traction among businesses and individuals. It serves as an ideal environmentally friendly alternative to conventional printed and signed documents, allowing you to locate the appropriate form and securely store it online. airSlate SignNow equips you with all the necessary tools to create, alter, and electronically sign your documents swiftly without any hold-ups. Handle Prior Authorization Benefit Form on any device with airSlate SignNow Android or iOS applications and enhance any document-related workflow today.
How to adjust and electronically sign Prior Authorization Benefit Form with ease
- Locate Prior Authorization Benefit Form and then click Get Form to begin.
- Utilize the tools we offer to fill out your form.
- Highlight pertinent sections of your documents or mask sensitive data with tools that airSlate SignNow specifically provides for that purpose.
- Create your signature using the Sign tool, which takes mere seconds and holds the same legal validity as a traditional wet ink signature.
- Review the details and then click on the Done button to save your modifications.
- Select your preferred method to send your form, via email, text message (SMS), or invitation link, or download it to your computer.
Forget about lost or misplaced files, tedious form searches, or errors that necessitate printing new copies of documents. airSlate SignNow meets all your document management needs in just a few clicks from any device you prefer. Adjust and electronically sign Prior Authorization Benefit Form and ensure effective communication at every step of your form preparation journey with airSlate SignNow.
Create this form in 5 minutes or less
Create this form in 5 minutes!
How to create an eSignature for the prior authorization benefit form
The way to generate an eSignature for your PDF online
The way to generate an eSignature for your PDF in Google Chrome
How to generate an electronic signature for signing PDFs in Gmail
How to generate an eSignature straight from your smartphone
The way to create an electronic signature for a PDF on iOS
How to generate an eSignature for a PDF document on Android
People also ask
-
What is a health plan pharmacy and how does it work?
A health plan pharmacy is a designated network of pharmacies that a health insurance provider collaborates with to offer prescription medications at reduced costs. By utilizing a health plan pharmacy, members can access essential medications while benefiting from negotiated pricing and better medication management.
-
How can airSlate SignNow streamline the process with health plan pharmacy documentation?
airSlate SignNow simplifies the eSigning and management of crucial health plan pharmacy documents, allowing healthcare professionals to process prescriptions and approvals faster. With its intuitive platform, users can easily send, sign, and track documents, ensuring compliance and efficiency in managing health plan pharmacy agreements.
-
What are the pricing options for using airSlate SignNow in relation to health plan pharmacy requirements?
AirSlate SignNow offers flexible pricing plans that cater to different business needs, including those in the healthcare sector dealing with health plan pharmacy documents. Plans are competitively priced to ensure that you get the best value while managing your document workflows effectively.
-
Can airSlate SignNow integrate with other health plan pharmacy management systems?
Yes, airSlate SignNow can integrate seamlessly with various health plan pharmacy management systems, enhancing your document workflow. This integration allows for better data sharing and improved operational efficiency when handling patient prescriptions and health plan pharmacy contracts.
-
What are the key benefits of using airSlate SignNow for health plan pharmacy documents?
Using airSlate SignNow for health plan pharmacy documents provides several benefits, such as faster turnaround times for document approvals and enhanced security for sensitive patient information. Additionally, it offers an easy-to-use interface that requires minimal training, making it ideal for healthcare providers.
-
Is airSlate SignNow compliant with health plan pharmacy regulations?
Yes, airSlate SignNow is designed with compliance in mind, adhering to necessary regulations such as HIPAA for health plan pharmacy documentation. This ensures that your sensitive healthcare information is secure while you manage and sign documents electronically.
-
How does airSlate SignNow enhance team collaboration on health plan pharmacy projects?
AirSlate SignNow fosters improved team collaboration on health plan pharmacy projects by allowing multiple team members to review and sign documents in real-time. This feature not only accelerates project timelines but also ensures that all relevant parties remain informed and involved throughout the process.
Get more for Prior Authorization Benefit Form
- Fencing contract for contractor new jersey form
- Hvac contract for contractor new jersey form
- Landscape contract for contractor new jersey form
- Commercial contract for contractor new jersey form
- Excavator contract for contractor new jersey form
- Renovation contract for contractor new jersey form
- Concrete mason contract for contractor new jersey form
- Sample demolition contract form
Find out other Prior Authorization Benefit Form
- eSignature New Jersey Healthcare / Medical Credit Memo Myself
- eSignature North Dakota Healthcare / Medical Medical History Simple
- Help Me With eSignature Arkansas High Tech Arbitration Agreement
- eSignature Ohio Healthcare / Medical Operating Agreement Simple
- eSignature Oregon Healthcare / Medical Limited Power Of Attorney Computer
- eSignature Pennsylvania Healthcare / Medical Warranty Deed Computer
- eSignature Texas Healthcare / Medical Bill Of Lading Simple
- eSignature Virginia Healthcare / Medical Living Will Computer
- eSignature West Virginia Healthcare / Medical Claim Free
- How To eSignature Kansas High Tech Business Plan Template
- eSignature Kansas High Tech Lease Agreement Template Online
- eSignature Alabama Insurance Forbearance Agreement Safe
- How Can I eSignature Arkansas Insurance LLC Operating Agreement
- Help Me With eSignature Michigan High Tech Emergency Contact Form
- eSignature Louisiana Insurance Rental Application Later
- eSignature Maryland Insurance Contract Safe
- eSignature Massachusetts Insurance Lease Termination Letter Free
- eSignature Nebraska High Tech Rental Application Now
- How Do I eSignature Mississippi Insurance Separation Agreement
- Help Me With eSignature Missouri Insurance Profit And Loss Statement