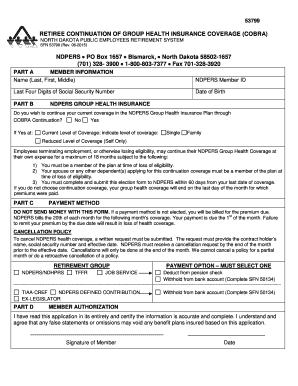
RETIREE CONTINUATION of GROUP HEALTH INSURANCE COVERAGE COBRA Form


What is the Retiree Continuation of Group Health Insurance Coverage COBRA
The Retiree Continuation of Group Health Insurance Coverage under COBRA allows eligible retirees to maintain their group health insurance coverage after leaving employment. This federal law ensures that individuals who have been part of a group health plan can continue their health benefits for a limited period, typically up to eighteen months, although this can extend under certain circumstances. The coverage includes the same benefits that were available while employed, providing a safety net for retirees as they transition to other health insurance options or Medicare.
Eligibility Criteria for COBRA Coverage
To qualify for the Retiree Continuation of Group Health Insurance Coverage through COBRA, individuals must meet specific eligibility requirements. Generally, retirees must have been enrolled in their employer's group health plan at the time of their employment termination. Additionally, the employer must have twenty or more employees for COBRA to apply. Retirees who are eligible for Medicare or who have access to another group health plan may not qualify for COBRA coverage. It's essential for retirees to review their eligibility carefully to ensure they can take advantage of this benefit.
Steps to Complete the COBRA Enrollment Process
Completing the enrollment process for the Retiree Continuation of Group Health Insurance Coverage involves several key steps:
- Notify the employer: Retirees should inform their employer of their intention to enroll in COBRA coverage.
- Receive the election notice: Employers are required to provide a COBRA election notice within fourteen days of the retirement date.
- Review the notice: The notice will outline the rights, responsibilities, and costs associated with COBRA coverage.
- Complete the enrollment form: Retirees must fill out the COBRA enrollment form accurately and completely.
- Submit the form: Send the completed form back to the employer or the designated plan administrator within the specified time frame.
- Pay premiums: Retirees must pay the required premiums to maintain their coverage, typically within a thirty-day grace period.
Required Documents for COBRA Enrollment
When enrolling in the Retiree Continuation of Group Health Insurance Coverage under COBRA, retirees need to prepare specific documents to facilitate the process. These may include:
- A copy of the COBRA election notice received from the employer.
- The completed COBRA enrollment form, which includes personal and health plan information.
- Proof of identity and employment, such as a driver's license or employee ID.
- Any additional documentation requested by the employer or health plan administrator.
Legal Use of COBRA Coverage
The legal framework surrounding the Retiree Continuation of Group Health Insurance Coverage under COBRA is designed to protect retirees' rights to health insurance. Employers must comply with federal regulations, ensuring that retirees are informed of their rights and options. Failure to adhere to these regulations can result in penalties for the employer. Retirees should be aware of their legal rights, including the right to appeal decisions regarding their coverage and the right to receive clear information about their benefits.
Filing Deadlines and Important Dates
Understanding the filing deadlines and important dates associated with COBRA coverage is crucial for retirees. Key dates include:
- Election period: Retirees typically have sixty days from the date of the election notice to enroll in COBRA coverage.
- Premium payment deadlines: Payments must be made within thirty days of the due date to avoid losing coverage.
- Notification timelines: Employers must provide the COBRA election notice within fourteen days of the qualifying event.
Quick guide on how to complete retiree continuation of group health insurance coverage cobra
Complete [SKS] effortlessly on any device
Managing documents online has gained traction among businesses and individuals. It offers an ideal eco-conscious alternative to traditional printed and signed paperwork, allowing you to access the necessary form and securely store it on the web. airSlate SignNow provides all the tools you need to create, modify, and eSign your documents rapidly without delays. Manage [SKS] on any platform using airSlate SignNow's Android or iOS applications and enhance any document-centric operation today.
How to modify and eSign [SKS] with ease
- Locate [SKS] and click Get Form to begin.
- Utilize the tools we provide to complete your form.
- Highlight necessary portions of the documents or obscure sensitive information with the tools that airSlate SignNow specifically offers for that purpose.
- Create your signature with the Sign tool, which takes mere seconds and carries the same legal validity as a conventional wet ink signature.
- Review all the details and click on the Done button to save your changes.
- Select your preferred method to send your form, whether by email, SMS, invite link, or download it to your computer.
Eliminate concerns about lost or misplaced documents, tedious form searches, or mistakes that require printing new copies. airSlate SignNow addresses your document management needs in just a few clicks from any device of your choice. Modify and eSign [SKS] and ensure outstanding communication at every stage of your form preparation process with airSlate SignNow.
Create this form in 5 minutes or less
Related searches to RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA
Create this form in 5 minutes!
How to create an eSignature for the retiree continuation of group health insurance coverage cobra
How to create an electronic signature for a PDF online
How to create an electronic signature for a PDF in Google Chrome
How to create an e-signature for signing PDFs in Gmail
How to create an e-signature right from your smartphone
How to create an e-signature for a PDF on iOS
How to create an e-signature for a PDF on Android
People also ask
-
What is RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA?
RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA allows retirees to maintain their group health insurance coverage after leaving employment. This federal law ensures that retirees can continue their health benefits for a limited time, providing essential support during their transition to retirement.
-
How does airSlate SignNow facilitate the RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA process?
airSlate SignNow streamlines the RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA process by enabling businesses to easily send and eSign necessary documents. This efficient solution reduces paperwork and ensures that retirees can quickly access their health insurance options without unnecessary delays.
-
What are the benefits of using airSlate SignNow for RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA?
Using airSlate SignNow for RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA offers several benefits, including faster document processing and enhanced security. The platform's user-friendly interface makes it easy for retirees to understand their options and complete necessary paperwork efficiently.
-
Is there a cost associated with RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA?
Yes, there are costs associated with RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA, typically involving premiums that retirees must pay to maintain their coverage. The specific costs can vary based on the employer's plan and the retiree's previous coverage, so it's essential to review the details provided during the COBRA notification process.
-
What features does airSlate SignNow offer for managing RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA?
airSlate SignNow offers features such as customizable templates, secure eSigning, and automated reminders to help manage RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA. These tools simplify the documentation process, ensuring that all necessary forms are completed accurately and on time.
-
How can businesses integrate airSlate SignNow with their existing systems for RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA?
Businesses can easily integrate airSlate SignNow with their existing HR and benefits management systems to streamline the RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA process. This integration allows for seamless data transfer and ensures that all relevant information is readily available for retirees.
-
What should retirees know about their rights under RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA?
Retirees should be aware that under RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA, they have the right to continue their health insurance for a specified period, typically up to 18 months. It's crucial for retirees to understand their rights and responsibilities, including payment deadlines and coverage options.
Get more for RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA
- Marine regatta permit application instructions dec ny form
- Ohio uniform incident report 2011 2019
- 529 investment forms and applications collegeadvantage
- Ohio withdrawal 2015 form
- Concealed carry license and renewal application form
- Deq va comprehensive site compliance evaluation sample 2011 2019 form
- South carolina department of motor vehicles request for scdmv form
- Sel 114 candidate filing individual electors oregon secretary of form
Find out other RETIREE CONTINUATION OF GROUP HEALTH INSURANCE COVERAGE COBRA
- Can I Electronic signature Texas Government PPT
- How To Electronic signature Utah Government Document
- How To Electronic signature Washington Government PDF
- How Can I Electronic signature New Mexico Finance & Tax Accounting Word
- How Do I Electronic signature New York Education Form
- How To Electronic signature North Carolina Education Form
- How Can I Electronic signature Arizona Healthcare / Medical Form
- How Can I Electronic signature Arizona Healthcare / Medical Presentation
- How To Electronic signature Oklahoma Finance & Tax Accounting PDF
- How Can I Electronic signature Oregon Finance & Tax Accounting PDF
- How To Electronic signature Indiana Healthcare / Medical PDF
- How Do I Electronic signature Maryland Healthcare / Medical Presentation
- How To Electronic signature Tennessee Healthcare / Medical Word
- Can I Electronic signature Hawaii Insurance PDF
- Help Me With Electronic signature Colorado High Tech Form
- How To Electronic signature Indiana Insurance Document
- Can I Electronic signature Virginia Education Word
- How To Electronic signature Louisiana Insurance Document
- Can I Electronic signature Florida High Tech Document
- Can I Electronic signature Minnesota Insurance PDF