Prior Authorization Request Form Member OptumRx


What is the Prior Authorization Request Form Member OptumRx
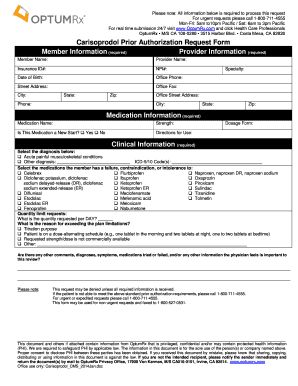
The Prior Authorization Request Form Member OptumRx is a crucial document used in the healthcare process. It is designed for members seeking approval from their insurance provider before certain medications or treatments can be covered. This form ensures that the prescribed services align with the insurance policy guidelines, helping to manage costs and ensure appropriate care. By submitting this form, members can facilitate the review process for their medications, ensuring that they receive the necessary treatment without unnecessary delays.
How to use the Prior Authorization Request Form Member OptumRx
Using the Prior Authorization Request Form Member OptumRx involves several straightforward steps. First, members need to obtain the form, which can typically be found on the OptumRx website or through their healthcare provider. Once the form is in hand, it should be filled out with accurate information regarding the member's personal details, the prescribed medication, and the healthcare provider's information. After completing the form, members can submit it electronically or by mail, depending on the options provided by their insurance plan. It is essential to ensure that all required fields are filled out to avoid delays in processing.
Steps to complete the Prior Authorization Request Form Member OptumRx
Completing the Prior Authorization Request Form Member OptumRx requires careful attention to detail. Here are the steps to follow:
- Gather necessary information, including personal details, medication name, and prescribing physician's information.
- Access the form from the OptumRx website or through your healthcare provider.
- Fill in all required fields accurately, ensuring that no information is omitted.
- Review the completed form for accuracy and completeness.
- Submit the form as directed, either electronically or via mail.
Legal use of the Prior Authorization Request Form Member OptumRx
The legal use of the Prior Authorization Request Form Member OptumRx is governed by various regulations surrounding healthcare documentation. When completed correctly, this form serves as a legally binding request for approval from the insurance provider. It is essential that the form is filled out truthfully and accurately, as any discrepancies could lead to denial of coverage or legal issues. Additionally, electronic submissions must comply with eSignature laws, ensuring that they are recognized as valid and enforceable under U.S. law.
Key elements of the Prior Authorization Request Form Member OptumRx
Several key elements must be included in the Prior Authorization Request Form Member OptumRx for it to be valid. These include:
- Member's full name and contact information.
- Insurance policy number and group number.
- Details of the prescribed medication, including dosage and frequency.
- Prescribing physician's name, contact information, and signature.
- Any relevant medical history or justification for the requested medication.
Form Submission Methods (Online / Mail / In-Person)
Members have several options for submitting the Prior Authorization Request Form Member OptumRx. The most common methods include:
- Online Submission: Many insurance providers offer a secure portal for electronic submissions, allowing for quicker processing times.
- Mail: Members can print the completed form and send it via postal service to the designated address provided by their insurance plan.
- In-Person: In some cases, members may choose to deliver the form directly to their healthcare provider's office for submission.
Quick guide on how to complete prior authorization request form member optumrx 50745103
Complete Prior Authorization Request Form Member OptumRx effortlessly on any device
Digital document management has gained traction among businesses and individuals alike. It serves as an ideal eco-friendly substitute for conventional printed and signed documents, allowing you to easily find the appropriate form and securely archive it online. airSlate SignNow equips you with all the tools necessary to create, modify, and eSign your documents quickly without delays. Handle Prior Authorization Request Form Member OptumRx on any platform using airSlate SignNow's Android or iOS applications and simplify any document-related process today.
The simplest way to alter and eSign Prior Authorization Request Form Member OptumRx without hassle
- Find Prior Authorization Request Form Member OptumRx and click Get Form to begin.
- Utilize the tools we provide to complete your form.
- Emphasize pertinent sections of the documents or obscure sensitive information with tools that airSlate SignNow specifically offers for that purpose.
- Create your signature using the Sign feature, which takes seconds and holds the same legal validity as a traditional handwritten signature.
- Review all the details and click on the Done button to save your modifications.
- Choose how you want to send your form, whether by email, text message (SMS), an invite link, or downloading it to your computer.
Eliminate the concern of lost or misplaced files, tedious form navigation, or errors that necessitate printing new document versions. airSlate SignNow meets your document management requirements in just a few clicks from your preferred device. Modify and eSign Prior Authorization Request Form Member OptumRx to ensure excellent communication at every stage of the form preparation process with airSlate SignNow.
Create this form in 5 minutes or less
Create this form in 5 minutes!
How to create an eSignature for the prior authorization request form member optumrx 50745103
How to create an electronic signature for a PDF online
How to create an electronic signature for a PDF in Google Chrome
How to create an e-signature for signing PDFs in Gmail
How to create an e-signature right from your smartphone
How to create an e-signature for a PDF on iOS
How to create an e-signature for a PDF on Android
People also ask
-
What is the Prior Authorization Request Form Member OptumRx?
The Prior Authorization Request Form Member OptumRx is a necessary document for obtaining approval from your insurance provider before certain medications or treatments are administered. This form helps healthcare providers communicate essential information to ensure that patients receive the coverage they need.
-
How can I access the Prior Authorization Request Form Member OptumRx?
You can easily access the Prior Authorization Request Form Member OptumRx through the OptumRx website or by asking your healthcare provider. Many providers have digital solutions or can provide you with the necessary forms or templates to fill out.
-
Is there a fee associated with submitting the Prior Authorization Request Form Member OptumRx?
Most insurance companies and healthcare providers do not charge a fee for submitting the Prior Authorization Request Form Member OptumRx. However, it's essential to check with your insurance provider for any potential costs that may be associated with the review process.
-
What information do I need to complete the Prior Authorization Request Form Member OptumRx?
To complete the Prior Authorization Request Form Member OptumRx, you typically need patient details, medical history, prescribed medications, and diagnosis information. Ensure that all fields are accurately filled to avoid any delays in processing.
-
How long does it take to process the Prior Authorization Request Form Member OptumRx?
The processing time for the Prior Authorization Request Form Member OptumRx can vary depending on the insurance provider. Generally, you can expect a response within a few business days, but it may take longer if additional documentation is required.
-
Can I track the status of my Prior Authorization Request Form Member OptumRx?
Yes, many insurance companies offer online portals where you can track the status of your Prior Authorization Request Form Member OptumRx. You may also contact your healthcare provider or insurance representative for updates directly.
-
What should I do if my Prior Authorization Request Form Member OptumRx is denied?
If your Prior Authorization Request Form Member OptumRx is denied, review the denial notice for specific reasons. You can appeal the decision by providing additional medical documentation or consulting with your healthcare provider for clarification and assistance.
Get more for Prior Authorization Request Form Member OptumRx
- Health care proxy etc form
- Form sd 988lt
- Sd notarial certificates notary stamp form
- Ohio southern district bankruptcy guide and forms package
- Alabama abandoned motor vehicle bill of salefrkwita form
- County of state of south dakota hereinafter seller whether one or form
- City of county of and state of south dakota towit form
- Plan dated form
Find out other Prior Authorization Request Form Member OptumRx
- Electronic signature Oregon Non-Profit POA Free
- Electronic signature South Dakota Non-Profit Business Plan Template Now
- Electronic signature South Dakota Non-Profit Lease Agreement Template Online
- Electronic signature Legal Document Missouri Online
- Electronic signature Missouri Legal Claim Online
- Can I Electronic signature Texas Non-Profit Permission Slip
- Electronic signature Missouri Legal Rental Lease Agreement Simple
- Electronic signature Utah Non-Profit Cease And Desist Letter Fast
- Electronic signature Missouri Legal Lease Agreement Template Free
- Electronic signature Non-Profit PDF Vermont Online
- Electronic signature Non-Profit PDF Vermont Computer
- Electronic signature Missouri Legal Medical History Mobile
- Help Me With Electronic signature West Virginia Non-Profit Business Plan Template
- Electronic signature Nebraska Legal Living Will Simple
- Electronic signature Nevada Legal Contract Safe
- How Can I Electronic signature Nevada Legal Operating Agreement
- How Do I Electronic signature New Hampshire Legal LLC Operating Agreement
- How Can I Electronic signature New Mexico Legal Forbearance Agreement
- Electronic signature New Jersey Legal Residential Lease Agreement Fast
- How To Electronic signature New York Legal Lease Agreement