Pharmacy Prior Authorization Form 2012


What is the Pharmacy Prior Authorization Form
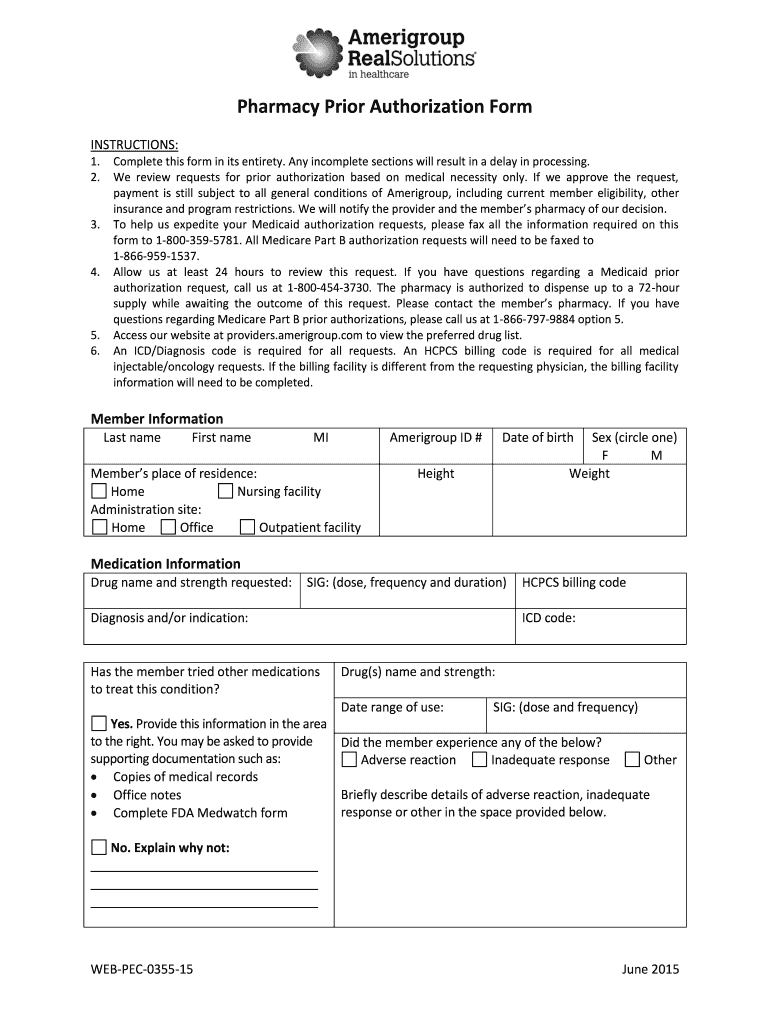
The Pharmacy Prior Authorization Form is a crucial document used in the healthcare system to obtain approval from a health insurance provider before a specific medication is dispensed. This form is essential for ensuring that prescribed medications are covered under a patient’s insurance plan, particularly for medications that may be considered high-cost or not typically covered. By submitting this form, healthcare providers can justify the medical necessity of the prescribed medication, allowing patients to access the treatment they need without incurring excessive out-of-pocket expenses.
How to use the Pharmacy Prior Authorization Form
Using the Pharmacy Prior Authorization Form involves several steps that ensure the process is smooth and effective. First, the healthcare provider must fill out the form with the patient's information, including their insurance details and the specific medication prescribed. Next, the provider should include relevant clinical information that supports the need for the medication, such as diagnosis and previous treatments. Once completed, the form can be submitted to the insurance company for review. It is important to follow up on the submission to ensure timely approval.
Steps to complete the Pharmacy Prior Authorization Form
Completing the Pharmacy Prior Authorization Form requires attention to detail to ensure all necessary information is provided. Here are the steps to follow:
- Gather patient information, including full name, date of birth, and insurance details.
- Provide the medication name, dosage, and prescribing physician's information.
- Include a detailed medical history that supports the need for the medication.
- Attach any relevant documentation, such as lab results or previous treatment records.
- Review the form for accuracy and completeness before submission.
Legal use of the Pharmacy Prior Authorization Form
The Pharmacy Prior Authorization Form must be used in compliance with relevant healthcare regulations and insurance policies. It is essential for healthcare providers to ensure that the information provided is accurate and truthful, as any misrepresentation can lead to legal repercussions. Additionally, the form must adhere to privacy laws, such as HIPAA, to protect patient information during the authorization process. Understanding these legal requirements helps to maintain the integrity of the healthcare system and protects both providers and patients.
Key elements of the Pharmacy Prior Authorization Form
Several key elements are critical to the Pharmacy Prior Authorization Form. These include:
- Patient Information: Essential details about the patient, including their insurance information.
- Medication Details: The name, dosage, and frequency of the prescribed medication.
- Clinical Justification: A section where the healthcare provider explains the necessity of the medication.
- Supporting Documentation: Any additional records or information that validate the request.
- Provider Information: The name and contact details of the healthcare provider submitting the form.
Form Submission Methods
The Pharmacy Prior Authorization Form can be submitted through various methods, depending on the insurance provider's requirements. Common submission methods include:
- Online Submission: Many insurance companies offer online portals where forms can be submitted electronically.
- Mail: The form can be printed and sent via postal mail to the insurance provider.
- Fax: Some providers may allow the form to be faxed directly to their office.
It is advisable to confirm the preferred submission method with the insurance provider to ensure compliance and expedite the approval process.
Quick guide on how to complete pharmacy authorization form
The simplest method to obtain and sign Pharmacy Prior Authorization Form
On the scale of your entire organization, ineffective procedures concerning paper authorization can take up a signNow amount of productive time. Signing documents such as Pharmacy Prior Authorization Form is an inherent component of operations across all sectors, which is why the effectiveness of each agreement’s lifecycle has a profound impact on the company’s overall performance. With airSlate SignNow, signing your Pharmacy Prior Authorization Form can be as straightforward and quick as possible. This platform provides you with the latest version of nearly any document. Even better, you can sign it instantly without needing to install external applications on your device or print out physical copies.
Steps to acquire and sign your Pharmacy Prior Authorization Form
- Explore our collection by category or utilize the search bar to locate the document you require.
- View the form preview by clicking Learn more to confirm it’s the correct one.
- Select Get form to begin editing immediately.
- Fill out your form and include any mandatory information using the toolbar.
- Once finished, click the Sign tool to sign your Pharmacy Prior Authorization Form.
- Choose the signature method that suits you best: Draw, Create initials, or upload a photo of your handwritten signature.
- Click Done to complete editing and proceed to document-sharing options as necessary.
With airSlate SignNow, you possess everything necessary to manage your documents efficiently. You can find, fill in, edit, and even send your Pharmacy Prior Authorization Form all in one tab without any complications. Enhance your workflows with a single, intelligent eSignature solution.
Create this form in 5 minutes or less
Find and fill out the correct pharmacy authorization form
FAQs
-
Why would a doctor send a prescription to a pharmacy, but not respond to repeated requests from the pharmacy to fill out a faxed prior authorization form?
Filling out a prior authorization is not a requirement of our practice. Most of us do this to help our patients, and it is sometimes taken for granted.Think about it. It is your insurance company that is requesting us to fill out this form, taking time away from actually treating patients, to help you save money on your medications. We understand that, and usually do our best to take care of them, but unless we have a large practice, with someone actually paid to spend all their time doing these PA’s, we have to carve out more time from our day to fill out paperwork.It’s also possible, although not likely, that the pharmacy does not have the correct fax number, the faxes have been misplaced, the doctor has some emergencies and is running behind, went on vacation, and so on.Paperwork and insurance requests have become more and more burdensome on our practices, not due to anything on the part of our patients, but a major hassle none the less.
-
How do I fill out the MHT-CET MBA exam application form in detail?
DTE Maharashtra has discharged MHT CET 2018 application form as on January 18 in online mode, can be filled by competitors by following the means said in how to fill MHT CET application frame 2018. Applicants who need to enlist themselves for the selection test should take after the means as given in how to fill MHT CET 2018 application form to maintain a strategic distance from oversights and entire method to go smooth and bother free. The means to fill the application type of MHT CET 2018 incorporates enlistment, filling of required subtle elements, transferring of filtered reports, instalment and affirmation page download. Hopefuls are required to fill the application type of MHT CET 2018 painstakingly to stay away from dismissal by the specialists. It is essential to take the application shape filling methodology of MHT CET genuinely on the grounds that exclusive those hopefuls who will present their structures effectively will get concede cards. Such applicants who will have legitimate MHT CET 2018 concede cards will be permitted to show up in the exam.Competitors must read the means offered underneath to fill and submit MHT CET 2018 application frame in a sorted-out way:Stage 1 – RegistrationApplicants should enrol themselves and give the required details. Candidate should concur whether he or she is an Indian resident or not.Proceeding onward, they will be required to fill the accompanying individual subtle elements:Full name (as showing up on the announcement of characteristics of SSC tenth or proportional exam), Father’s name, Mother’s first name, Last name, Gender, Contact Information, Address for correspondence, House No/Street, Area Name, Town/City , State, District, Pin code, Country, Mobile Number, Primary Email Id (Email will be sent to this email ID), Alternate Email Id (Parent’s Email ID, if accessible), Contact Telephone No. (with STD Code), Permanent Residence in Village/Town/City, Domicile of Maharashtra/Disputed Maharashtra Karnataka Border (MKB)/Outside Maharashtra, Reservation, Category of competitor (Caste perceived in Maharashtra state), Candidates having a place with SC, ST, VJ(A), NT(B), NT(C), NT(D), OBC and SBC classes must have their individual standing authentications, Candidates having a place with Non Creamy Layer (NCL) should create substantial testament upto March 31, 2019, Other DetailsRegardless of whether the candidate has a place with – PWD class or not (competitors qualified who are qualified under this classification ought to have under 40% incapacity), visually impaired, low vision. Orthopedically debilitated and competitors influenced with Cerebral Palsy and Dyslexia, who are not in a situation to compose, can benefit a copyist/author for the MHT-CET 2018 examRegardless of whether the applicant is a J&K vagrant or notReligionOther placement tests that applicant has enrolled for (JEE Main/NEET/None)Add up to Annual Family IncomeAadhaar NumberFinancial balance DetailsName of the record holder according to Bank recordName of the BankName of the Bank BranchKind of Account (Savings/Current)Financial balance NumberIFSC CodePoints of interest of HSC (twelfth/Equivalent Examination)Regardless of whether hopeful has passed/showed up for confirmation in Pharmacy (just for Biology applicants)Place from where hopeful has finished HSC (twelfth)/proportional exam showing up/Passed from school/Jr. School arranged (Maharashtra/Outside Maharashtra)Subtle elements required for MHT-CET 2018Subjects for CET examination (Physics, Chemistry, Mathematics, Biology)Dialect for the exam (English, Marathi, Urdu)Enter secret keyCompetitors should make a secret word (least 8 and most extreme 15 characters and should have one capitalized, one lower case and one numeric)In the wake of entering the secret key, competitors should affirm it. This secret word will be utilized for future logins.Statement by the hopefulApplicants should read the revelation composed and after that tap on “I Agree”Applicants need to enter the security key as gave and after that tap on “Next” catchStage 2 – Confirmation and SubmissionIn the wake of filling the previously mentioned subtle elements, hopefuls will have the capacity to check the data filled and alter certain things in the application frame.Applicants can backpedal and change or alter the accompanying particulars (as noticeable in green shading) before accommodation:Exam focusSubjects pickedDialect of the examIndividual with handicap choiceIn any case, there are particulars (as unmistakable in blue shading) that can’t be altered at this stage once submitted:Father’s nameLast nameDate of birthVersatile numberEmail IDSubsequent to rolling out the improvements, if required, hopefuls should present the shape.Stage 3 – Application number gotApplicants will get a message on the screen in regards to effective enlistment for MHT CET 2018 with their application number. A similar number will be sent to them gave email ID. Competitors can see and check their entered data in this progression.Stage 4 – Edit and Upload photo and markApplicants will have the capacity to alter the points of interest they have filled in the application frame. In any case, regardless they won’t have the capacity to alter their full name, father’s name, last name, date of birth, versatile number and email ID. In the event that candidates would prefer not to alter any points of interest, they can move to the subsequent stage of transferring their photo and mark in the arrangement recommended by the experts.Stage 5 – Uploading photo and markApplicants should transfer their current identification estimate shading photo and mark in the configuration given in the table underneath. On the off chance that, applicants are not ready to transfer the right photographs/marks, they should reload the right records and afterward transfer.Stage 6 – VerificationCompetitors will get a message on their screens with respect to fruitful transferring of photo and mark. They will likewise have the capacity to see a connection saying ” Click here to make payment “. Applicants should tap on the connection to enter the instalment entryway.Stage 7 – Payment gatewayHopefuls will have the capacity to see every one of the subtle elements filled by them alongside their transferred photo and mark on their screens. The application expense sum will likewise be noticeable in this progression, which they should pay in the wake of perusing the revelation. It is to noticed that competitors will have the capacity to change their subjects they are applying for.Applicants will have the capacity to influence application to charge payment through credit/check card, net saving money, plastic (ATM PIN), wallets and then some. They should influence instalment of the application to sum with comfort charge and expense.After instalment of utilisation charge, competitors will have the capacity to see a message on their screen with respect to accomplishment of exchange. Applicants must remove a print from this page.Stage 8 – Acknowledgment pageCompetitors must take a print from the affirmation page and keep it securely for some time later.Hope this Helps!!
-
Why do pharmacists need so much time to count out pills and fill prescriptions?
Counting out pills is the least time consuming part of filling a prescription. Let me give you a brief walk through (different pharmacies may vary slightly):Prescription comes in the pharmacy (by whatever means).The pharmacist checks the prescription to make sure everything is correct and makes sense. You would be amazed at the number of times I’ve seen prescriptions for rash creams to be taken by mouth, inappropriate dosing schedules, or just sheer gibberish on a prescription form.If the pharmacist thinks there is a problem with the prescription, the pharmacy tech has to call the doctor’s office for clarification. Few doctors are happy to hear that someone is questioning their prescribing ability. There may be nothing wrong the prescription itself, but the new drug may interact with something you are already taking, so we have to get an alternative.Once that is straightened out (which may require quite a bit of phone tag), I, the pharmacy technician enter the prescription into the system.The pharmacist double checks my work.Then, and only then, do we run your insurance. It may go through the first time, it may not. It may require a prior authorization. The drug may be covered, but only for a certain number of doses per month. We pharmacy techs have to work all that out and navigate the maze of your insurance - assuming we have up-to-date information. Please let us know if you have changed insurance.Once your insurance has been processed, your prescription is added to the queue. Yours is not the only prescription. They are generally filled in the order they came in, with some priority given to people who are waiting.Your prescription has worked its way to the front of the queue. A pharmacy tech goes to the shelf, pulls the drug off the shelf, checking to make sure it is the correct drug in the correct strength. Bar codes are scanned, a label is generated, pills are counted out. Counting out pills may look easy, but some of those suckers are bound and determined to cause a problem. Let me pour a bunch of BB’s on a tray and see how fast you can count them out. Yes, there are pills that are shaped like BB’s. Then there are the fragile pills, the capsules that want to stick to the tray due to static, the tiny pills, the capsules that want to come open. That’s just pills. There are liquids, creams, drops, and pastes that have to be mixed at the time of dispensing.The label is put on the bottle. The pills are put in the bottle. The bottle and the associated paperwork are sent to the pharmacist for verification.Once the pharmacist okays it, the vial(s) and associated paperwork are put in a bag to await you. If for some reason, the pharmacist finds a problem with it, we have to go back a couple of steps and try again.Keep in mind all this is going on while other patients are coming to the counter to pick up or drop off prescriptions, the phone is ringing, people are coming through the drive-thru, people are asking us where the toothpaste or hair dye are, people wanting to know how long they will have to wait for a flu shot. I’m exhausted just thinking about it.All that so that you can get the correct drug, in the correct form, in the correct dose, in the correct quantity and grumble at the pharmacy staff over having to wait a whole 20 minutes for your prescription. This is not fast food. If we screw this up, we could kill you. Cut us some slack. Drop off your prescription, go run a couple of errands, and pick it up later - and don’t yell at me because your copay went up. Go yell at your insurance company. They are the ones who make that decision, not the pharmacy.
-
How can I fill out the authorization form in Wipro's synergy?
By authorisation form I assume that you mean LOA. Just download the pdf and sign it with stylus or get a printout,sign it and scan the copy.Now upload it!If I my assumption is wrong please provide little clear picture!Thank you!Allah maalik!
-
What does the authorization form in Wipro’s Synergy need to be filled out?
I don't exactly remember how the form was looking like in synergy portal. But I hope it is Authorizing Wipro to do background verification on all the details provided by candidate. It needs your name and signature with date.
-
Can pharmacy be studied through the NEET?
What u want to ask exactly ? NEET is an entrance exam for medical colleges for MBBS/BDS courses. If you want to seek eligibility to b.pharm. course through neet then I would say you can but some states prefer there own entrance exam for pharmacy such as Maharashtra , Karnataka, west bengal , Orissa , andhra Pradesh, etc. And if seats remains vacant in pharmacy colleges thru state entrance exam then lastly they will fill through neet qualified candidates. But NEET is compulsory for B.Pharma. if you wish to study pharmacy from national level institutes such as BIT mesra, BITS pillani BHU-IP etc. But in these central/national level colleges first preference will be given to JEE advanced qualified candidates and if seats remaining vacant then those may be offered to neet qualified candidates. Just remember to study pharmacy through neet, qualify in neet is compulsory.
-
Do military members have to pay any fee for leave or fiancee forms?
NOOOOOOO. You are talking to a military romance scammer. I received an email from the US Army that directly answers your question that is pasted below please keep reading.I believe you are the victim of a military Romance Scam whereas the person you are talking to is a foreign national posing as an American Soldier claiming to be stationed overseas on a peacekeeping mission. That's the key to the scam they always claim to be on a peacekeeping mission.Part of their scam is saying that they have no access to their money that their mission is highly dangerous.If your boyfriend girlfriend/future husband/wife is asking you to do the following or has exhibited this behavior, it is a most likely a scam:Moves to private messaging site immediately after meeting you on Facebook or SnapChat or Instagram or some dating or social media site. Often times they delete the site you met them on right after they asked you to move to a more private messaging siteProfesses love to you very quickly & seems to quote poems and song lyrics along with using their own sort of broken language, as they profess their love and devotion quickly. They also showed concern for your health and love for your family.Promises marriage as soon as he/she gets to state for leave that they asked you to pay for.They Requests money (wire transfers) and Amazon, iTune ,Verizon, etc gift cards, for medicine, religious practices, and leaves to come home, internet access, complete job assignments, help sick friend, get him out of trouble, or anything that sounds fishy.The military does provide all the soldier needs including food medical Care and transportation for leave. Trust me, I lived it, you are probably being scammed. I am just trying to show you examples that you are most likely being connned.Below is an email response I received after I sent an inquiry to the US government when I discovered I was scammed. I received this wonderful response back with lots of useful links on how to find and report your scammer. And how to learn more about Romance Scams.Right now you can also copy the picture he gave you and do a google image search and you will hopefully see the pictures of the real person he is impersonating. this doesn't always work and take some digging. if you find the real person you can direct message them and alert them that their image is being used for scamming.Good Luck to you and I'm sorry this may be happening to you. please continue reading the government response I received below it's very informative. You have contacted an email that is monitored by the U.S. Army Criminal Investigation Command. Unfortunately, this is a common concern. We assure you there is never any reason to send money to anyone claiming to be a Soldier online. If you have only spoken with this person online, it is likely they are not a U.S. Soldier at all. If this is a suspected imposter social media profile, we urge you to report it to that platform as soon as possible. Please continue reading for more resources and answers to other frequently asked questions: How to report an imposter Facebook profile: Caution-https://www.facebook.com/help/16... < Caution-https://www.facebook.com/help/16... > Answers to frequently asked questions: - Soldiers and their loved ones are not charged money so that the Soldier can go on leave. - Soldiers are not charged money for secure communications or leave. - Soldiers do not need permission to get married. - Soldiers emails are in this format: john.doe.mil@mail.mil < Caution-mailto: john.doe.mil@mail.mil > anything ending in .us or .com is not an official email account. - Soldiers have medical insurance, which pays for their medical costs when treated at civilian health care facilities worldwide – family and friends do not need to pay their medical expenses. - Military aircraft are not used to transport Privately Owned Vehicles. - Army financial offices are not used to help Soldiers buy or sell items of any kind. - Soldiers deployed to Combat Zones do not need to solicit money from the public to feed or house themselves or their troops. - Deployed Soldiers do not find large unclaimed sums of money and need your help to get that money out of the country. Anyone who tells you one of the above-listed conditions/circumstances is true is likely posing as a Soldier and trying to steal money from you. We would urge you to immediately cease all contact with this individual. For more information on avoiding online scams and to report this crime, please see the following sites and articles: This article may help clarify some of the tricks social media scammers try to use to take advantage of people: Caution-https://www.army.mil/article/61432/< Caution-https://www.army.mil/article/61432/> CID advises vigilance against 'romance scams,' scammers impersonating Soldiers Caution-https://www.army.mil/article/180749 < Caution-https://www.army.mil/article/180749 > FBI Internet Crime Complaint Center: Caution-http://www.ic3.gov/default.aspx< Caution-http://www.ic3.gov/default.aspx> U.S. Army investigators warn public against romance scams: Caution-https://www.army.mil/article/130...< Caution-https://www.army.mil/article/130...> DOD warns troops, families to be cybercrime smart -Caution-http://www.army.mil/article/1450...< Caution-http://www.army.mil/article/1450...> Use caution with social networking Caution-https://www.army.mil/article/146...< Caution-https://www.army.mil/article/146...> Please see our frequently asked questions section under scams and legal issues. Caution-http://www.army.mil/faq/ < Caution-http://www.army.mil/faq/ > or visit Caution-http://www.cid.army.mil/ < Caution-http://www.cid.army.mil/ >. The challenge with most scams is determining if an individual is a legitimate member of the US Army. Based on the Privacy Act of 1974, we cannot provide this information. If concerned about a scam you may contact the Better Business Bureau (if it involves a solicitation for money), or local law enforcement. If you're involved in a Facebook or dating site scam, you are free to contact us direct; (571) 305-4056. If you have a social security number, you can find information about Soldiers online at Caution-https://www.dmdc.osd.mil/appj/sc... < Caution-https://www.dmdc.osd.mil/appj/sc... > . While this is a free search, it does not help you locate a retiree, but it can tell you if the Soldier is active duty or not. If more information is needed such as current duty station or location, you can contact the Commander Soldier's Records Data Center (SRDC) by phone or mail and they will help you locate individuals on active duty only, not retirees. There is a fee of $3.50 for businesses to use this service. The check or money order must be made out to the U.S. Treasury. It is not refundable. The address is: Commander Soldier's Records Data Center (SRDC) 8899 East 56th Street Indianapolis, IN 46249-5301 Phone: 1-866-771-6357 In addition, it is not possible to remove social networking site profiles without legitimate proof of identity theft or a scam. If you suspect fraud on this site, take a screenshot of any advances for money or impersonations and report the account on the social networking platform immediately. Please submit all information you have on this incident to Caution-www.ic3.gov < Caution-http://www.ic3.gov > (FBI website, Internet Criminal Complaint Center), immediately stop contact with the scammer (you are potentially providing them more information which can be used to scam you), and learn how to protect yourself against these scams at Caution-http://www.ftc.gov < Caution-http://www.ftc.gov > (Federal Trade Commission's website)
-
How can I fill out Google's intern host matching form to optimize my chances of receiving a match?
I was selected for a summer internship 2016.I tried to be very open while filling the preference form: I choose many products as my favorite products and I said I'm open about the team I want to join.I even was very open in the location and start date to get host matching interviews (I negotiated the start date in the interview until both me and my host were happy.) You could ask your recruiter to review your form (there are very cool and could help you a lot since they have a bigger experience).Do a search on the potential team.Before the interviews, try to find smart question that you are going to ask for the potential host (do a search on the team to find nice and deep questions to impress your host). Prepare well your resume.You are very likely not going to get algorithm/data structure questions like in the first round. It's going to be just some friendly chat if you are lucky. If your potential team is working on something like machine learning, expect that they are going to ask you questions about machine learning, courses related to machine learning you have and relevant experience (projects, internship). Of course you have to study that before the interview. Take as long time as you need if you feel rusty. It takes some time to get ready for the host matching (it's less than the technical interview) but it's worth it of course.
Create this form in 5 minutes!
How to create an eSignature for the pharmacy authorization form
How to generate an electronic signature for the Pharmacy Authorization Form online
How to generate an eSignature for the Pharmacy Authorization Form in Google Chrome
How to create an eSignature for signing the Pharmacy Authorization Form in Gmail
How to create an eSignature for the Pharmacy Authorization Form from your smartphone
How to make an eSignature for the Pharmacy Authorization Form on iOS devices
How to make an eSignature for the Pharmacy Authorization Form on Android devices
People also ask
-
What are Amerigroup forms and how can airSlate SignNow help with them?
Amerigroup forms are essential documents used in healthcare that require signatures for various purposes. airSlate SignNow offers a seamless solution to create, send, and eSign Amerigroup forms, streamlining the workflow and ensuring compliance. With the platform's user-friendly interface, you can quickly manage forms without any hassle.
-
Is airSlate SignNow a cost-effective solution for managing Amerigroup forms?
Absolutely! airSlate SignNow provides a cost-effective solution for businesses looking to manage Amerigroup forms efficiently. With various pricing plans, users can choose the option that best fits their budget while enjoying all the necessary features for secure document management.
-
What features does airSlate SignNow offer for Amerigroup forms?
airSlate SignNow is equipped with a variety of features designed specifically for Amerigroup forms. These include customizable templates, automated workflows, and real-time tracking of document status. This ensures that every step of your document signing process is streamlined and efficient.
-
Can I integrate airSlate SignNow with other tools for managing Amerigroup forms?
Yes, airSlate SignNow offers integration capabilities with various popular business tools such as Google Drive, Salesforce, and Microsoft Office. This makes it easy to manage Amerigroup forms within your existing workflows, enhancing productivity and collaboration.
-
How secure is airSlate SignNow for handling Amerigroup forms?
Security is a top priority at airSlate SignNow. The platform utilizes advanced encryption and compliance measures to ensure the safety of your Amerigroup forms. You can trust that your sensitive information is protected at all times.
-
What are the benefits of eSigning Amerigroup forms with airSlate SignNow?
eSigning Amerigroup forms with airSlate SignNow offers numerous benefits, including faster turnaround times and enhanced convenience for all parties involved. By eliminating the need for physical signatures, you can streamline processes and improve efficiency signNowly.
-
Can I access airSlate SignNow on mobile devices for Amerigroup forms?
Yes, airSlate SignNow has a mobile-friendly platform that allows you to manage Amerigroup forms on the go. Whether you're using a smartphone or tablet, you can easily send, sign, and store documents anytime, anywhere.
Get more for Pharmacy Prior Authorization Form
- Tr 500 s instruction to defendant for remote california courts courts ca form
- Fillable court forms california
- California time form
- Adopt 200 fillable form 2010
- Dv 500 form
- Dv 520 info s get ready for the court hearing spanish judicial council forms courts ca
- Fl 160 form 2007
- S lo para informaci n no entregue a la corte california courts courts ca 6967774
Find out other Pharmacy Prior Authorization Form
- Electronic signature South Carolina Sports Separation Agreement Easy
- Electronic signature Virginia Courts Business Plan Template Fast
- How To Electronic signature Utah Courts Operating Agreement
- Electronic signature West Virginia Courts Quitclaim Deed Computer
- Electronic signature West Virginia Courts Quitclaim Deed Free
- Electronic signature Virginia Courts Limited Power Of Attorney Computer
- Can I Sign Alabama Banking PPT
- Electronic signature Washington Sports POA Simple
- How To Electronic signature West Virginia Sports Arbitration Agreement
- Electronic signature Wisconsin Sports Residential Lease Agreement Myself
- Help Me With Sign Arizona Banking Document
- How Do I Sign Arizona Banking Form
- How Can I Sign Arizona Banking Form
- How Can I Sign Arizona Banking Form
- Can I Sign Colorado Banking PPT
- How Do I Sign Idaho Banking Presentation
- Can I Sign Indiana Banking Document
- How Can I Sign Indiana Banking PPT
- How To Sign Maine Banking PPT
- Help Me With Sign Massachusetts Banking Presentation