MODEL GENERAL NOTICE OF COBRA CONTINUATION COVERAGE RIGHTS
(For use by single-employer group health plans)
** CONTINUATION COVERAGE RIGHTS UNDER COBRA**
Introduction
You are receiving this notice because you have recently become covered under a group health
plan (the Plan). This notice contains important information about your right to COBRA
continuation coverage, which is a temporary extension of coverage under the Plan. This notice
generally explains COBRA continuation coverage, when it may become available to you
and your family, and what you need to do to protect the right to receive it.
The right to COBRA continuation coverage was created by a federal law, the Consolidated
Omnibus Budget Reconciliation Act of 1985 (COBRA). COBRA continuation coverage can
become available to you when you would otherwise lose your group health coverage. It can also
become available to other members of your family who are covered under the Plan when they
would otherwise lose their group health coverage. For additional information about your rights
and obligations under the Plan and under federal law, you should review the Plan’s Summary
Plan Description or contact the Plan Administrator.
What is COBRA Continuation Coverage?
COBRA continuation coverage is a continuation of Plan coverage when coverage would
otherwise end because of a life event known as a “qualifying event.” Specific qualifying events
are listed later in this notice. After a qualifying event, COBRA continuation coverage must be
offered to each person who is a “qualified beneficiary.” You, your spouse, and your dependent
children could become qualified beneficiaries if coverage under the Plan is lost because of the
qualifying event. Under the Plan, qualified beneficiaries who elect COBRA continuation
coverage [choose and enter appropriate information: must pay or are not required to pay] for
COBRA continuation coverage.
If you are an employee, you will become a qualified beneficiary if you lose your coverage under
the Plan because either one of the following qualifying events happens:
Your hours of employment are reduced, or
Your employment ends for any reason other than your gross misconduct.
If you are the spouse of an employee, you will become a qualified beneficiary if you lose your
coverage under the Plan because any of the following qualifying events happens:
Your spouse dies;
Your spouse’s hours of employment are reduced;
Your spouse’s employment ends for any reason other than his or her gross misconduct;
Your spouse becomes entitled to Medicare benefits (under Part A, Part B, or both); or
You become divorced or legally separated from your spouse.
Your dependent children will become qualified beneficiaries if they lose coverage under the
Plan because any of the following qualifying events happens:
The parent-employee dies;
The parent-employee’s hours of employment are reduced;
The parent-employee’s employment ends for any reason other than his or her gross
misconduct;
The parent-employee becomes entitled to Medicare benefits (Part A, Part B, or both);
The parents become divorced or legally separated; or
The child stops being eligible for coverage under the plan as a “dependent child.”
When is COBRA Coverage Available?
The Plan will offer COBRA continuation coverage to qualified beneficiaries only after the Plan
Administrator has been notified that a qualifying event has occurred. When the qualifying event
is the end of employment or reduction of hours of employment, death of the employee, [add if
Plan provides retiree health coverage: commencement of a proceeding in bankruptcy with
respect to the employer,] or the employee's becoming entitled to Medicare benefits (under Part
A, Part B, or both), the employer must notify the Plan Administrator of the qualifying event.
You Must Give Notice of Some Qualifying Events
For the other qualifying events ( divorce or legal separation of the employee and spouse or a
dependent child’s losing eligibility for coverage as a dependent child), you must notify the
Plan Administrator within 60 days [or enter longer period permitted under the terms of the
Plan] after the qualifying event occurs. You must provide this notice to: [Enter name of
appropriate party] . [Add description of any additional Plan procedures for this notice,
including a description of any required information or documentation.]
How is COBRA Coverage Provided?
Once the Plan Administrator receives notice that a qualifying event has occurred, COBRA
continuation coverage will be offered to each of the qualified beneficiaries. Each qualified
beneficiary will have an independent right to elect COBRA continuation coverage. Covered
2[ If the Plan provides retiree health coverage, add the following paragraph: ]
Sometimes, filing a proceeding in bankruptcy under title 11 of the United States Code can be
a qualifying event. If a proceeding in bankruptcy is filed with respect to [ enter name of
employer sponsoring the plan ], and that bankruptcy results in the loss of coverage of any
retired employee covered under the Plan, the retired employee will become a qualified
beneficiary with respect to the bankruptcy. The retired employee’s spouse, surviving spouse,
and dependent children will also become qualified beneficiaries if bankruptcy results in the
loss of their coverage under the Plan.
employees may elect COBRA continuation coverage on behalf of their spouses, and parents may
elect COBRA continuation coverage on behalf of their children.
COBRA continuation coverage is a temporary continuation of coverage. When the qualifying
event is the death of the employee, the employee's becoming entitled to Medicare benefits (under
Part A, Part B, or both), your divorce or legal separation, or a dependent child's losing eligibility
as a dependent child, COBRA continuation coverage lasts for up to a total of 36 months. When
the qualifying event is the end of employment or reduction of the employee's hours of
employment, and the employee became entitled to Medicare benefits less than 18 months before
the qualifying event, COBRA continuation coverage for qualified beneficiaries other than the
employee lasts until 36 months after the date of Medicare entitlement. For example, if a covered
employee becomes entitled to Medicare 8 months before the date on which his employment
terminates, COBRA continuation coverage for his spouse and children can last up to 36 months
after the date of Medicare entitlement, which is equal to 28 months after the date of the
qualifying event (36 months minus 8 months). Otherwise, when the qualifying event is the end
of employment or reduction of the employee’s hours of employment, COBRA continuation
coverage generally lasts for only up to a total of 18 months. There are two ways in which this
18-month period of COBRA continuation coverage can be extended.
Disability extension of 18-month period of continuation coverage
If you or anyone in your family covered under the Plan is determined by the Social Security
Administration to be disabled and you notify the Plan Administrator in a timely fashion, you and
your entire family may be entitled to receive up to an additional 11 months of COBRA
continuation coverage, for a total maximum of 29 months. The disability would have to have
started at some time before the 60th day of COBRA continuation coverage and must last at least
until the end of the 18-month period of continuation coverage. [Add description of any
additional Plan procedures for this notice, including a description of any required information or
documentation, the name of the appropriate party to whom notice must be sent, and the time
period for giving notice.]
Second qualifying event extension of 18-month period of continuation coverage
If your family experiences another qualifying event while receiving 18 months of COBRA
continuation coverage, the spouse and dependent children in your family can get up to 18
additional months of COBRA continuation coverage, for a maximum of 36 months, if notice of
the second qualifying event is properly given to the Plan. This extension may be available to the
spouse and any dependent children receiving continuation coverage if the employee or former
employee dies, becomes entitled to Medicare benefits (under Part A, Part B, or both), or gets
divorced or legally separated, or if the dependent child stops being eligible under the Plan as a
dependent child, but only if the event would have caused the spouse or dependent child to lose
coverage under the Plan had the first qualifying event not occurred.
3
If You Have Questions
Questions concerning your Plan or your COBRA continuation coverage rights should be
addressed to the contact or contacts identified below. For more information about your rights
under ERISA, including COBRA, the Health Insurance Portability and Accountability Act
(HIPAA), and other laws affecting group health plans, contact the nearest Regional or District
Office of the U.S. Department of Labor’s Employee Benefits Security Administration (EBSA) in
your area or visit the EBSA website at www.dol.gov/ebsa. (Addresses and phone numbers of
Regional and District EBSA Offices are available through EBSA’s website.)
Keep Your Plan Informed of Address Changes
In order to protect your family’s rights, you should keep the Plan Administrator informed of any
changes in the addresses of family members. You should also keep a copy, for your records, of
any notices you send to the Plan Administrator.
Plan Contact Information
[Enter name of group health plan and name (or position), address and phone number of party or
parties from whom information about the plan and COBRA continuation coverage can be
obtained on request.]
4
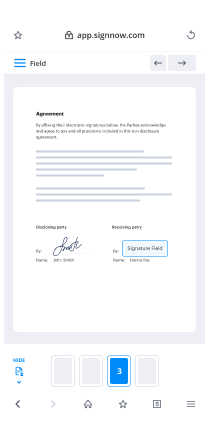
Useful advice for finalizing your ‘Cobra Notice Of Rights’ online
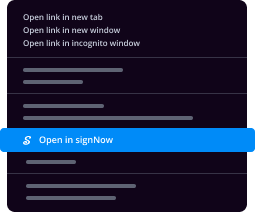
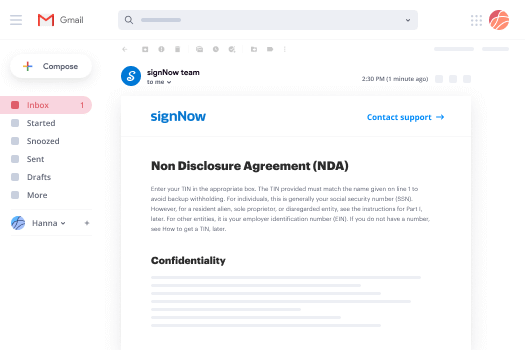
Are you fed up with the inconvenience of managing paperwork? Look no further than airSlate SignNow, the premier electronic signature solution for individuals and organizations. Bid farewell to the tedious process of printing and scanning documents. With airSlate SignNow, you can easily complete and sign documents online. Take advantage of the extensive features offered by this user-friendly and cost-effective platform and transform your approach to document handling. Whether you need to sign forms or gather electronic signatures, airSlate SignNow manages it all effortlessly, with just a few clicks.
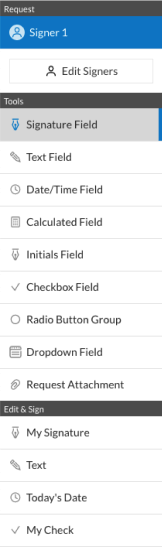
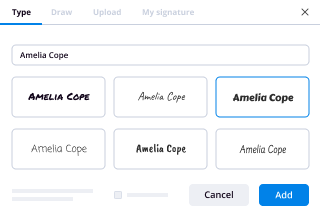
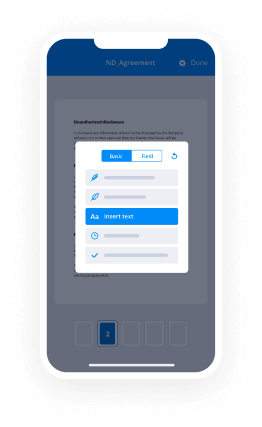
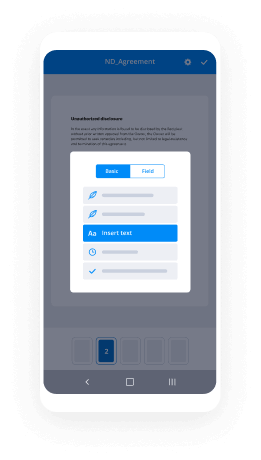
Follow this comprehensive guide:
- Sign in to your account or sign up for a free trial with our service.
- Click +Create to upload a document from your device, cloud, or our template library.
- Open your ‘Cobra Notice Of Rights’ in the editor.
- Click Me (Fill Out Now) to prepare the document on your end.
- Add and designate fillable fields for others (if needed).
- Proceed with the Send Invite settings to request eSignatures from others.
- Download, print your copy, or convert it into a reusable template.
Don't worry if you need to collaborate with your colleagues on your Cobra Notice Of Rights or send it for notarization—our solution provides you with everything you need to accomplish such tasks. Register with airSlate SignNow today and elevate your document management to a new standard!