JUNE 2008
V o l ume 5 , I ssue 3
Aetna
OfficeLink Updates
™
Northeast Region
Inside This Issue
OfficeWise . . . . . . . . . . . . . . .
It’s here! Access to Personal Health Records on NaviNet®
2-3
Policy and Practice Updates . . . . 4
Aetna’s Education Site for
Health Care Professionals. . . . . . 5
Prescription Medications &
Pharmacy Management . . . . . . . 6
Physician Focus. . . . . . . . . . . . . . . 7
Plan Facts and Features. . . . . . . . 8
Striving for Quality
Excellence. . . . . . . . . . . . . . . . . . . 9
Northeast News. . . . . . . . . . 10-11
Options to reach us
Go to www.aetna.com
Select “for Health Care Professionals”
n Select “Medical”
n Select “Log In” or “Register Now!”
n
n
Or call our Provider Service Center:
n
F
� or indemnity and PPO-based
benefits plans call 1-888-MDAetna
(1-888-632-3862)
1-800-624-0756 for calls related to
HMO-based benefits plans and WA
Primary Choice plan
n
Providers who have registered for NaviNet
can access Personal Health Record (PHR)
information for their Aetna patients
starting in late June. Please note that
an Aetna member must first give their
permission for their physician to view the
PHR through NaviNet.
Initially, only physicians whom the
member designates will be able to access
the PHR.
Benefits of accessing a PHR
Aetna’s PHR provides a comprehensive
view of a patient’s health care treatment
and health history. It contains up to 24
How to view a PHR
months of health information derived
There are two ways you can access a PHR: from medical claims, pharmacy claims,
laboratory results and self-reported
n � nce logged in to NaviNet, click on
O
information that patients can share with
“Aetna Health Plan” from the “Health
their doctors.
Plans” list on the left. Then, to search
for your patients’ PHR information,
By accessing this information, physicians
select the “View Personal Health
can see which prescriptions were filled
Records” button on Aetna’s Plan
and when, whether diagnostic studies
Central page. Once there, you can enter were performed and which specialists a
search criteria to narrow your search by patient may have seen. We encourage you
patient. Or,
to ask your Aetna patients to authorize
you for online access to their PHR.
n �
While performing an eligibility
To learn more
transaction, if a PHR was made
If you have questions, contact NaviNet
available to the requesting provider for
Customer Care at 1-888-482-8057. Or,
viewing, an “alert” will appear in the
send an email by selecting “Contact Us”
eligibility response.
from the “Customer Service” section at
the top of the screen.
Take our Toolkit survey – we’ll enter you in gift card drawing
We need your help.
Let us know if the Health Care
Professional Toolkit, our online
provider manual, meets your needs.
Please take a minute to tell us if the
toolkit makes it easier for you to work
with us by completing our brief online
survey at https://navinet.navimedix.
com/Main.asp. Once logged in, select
23.22.807.1-NE (6/08)
“Aetna Support Center” then “Doing
Business with Aetna” and “Health Care
Professional Toolkit.”
The survey is available from June 4
through August 29. Your completed
survey automatically enters you in
our drawing to win one of three $50
American Express gift cards. We
will notify winners in September.
�OfficeWise
Go totally electronic: Send us your COB claims
Stop submitting coordination of
benefits (COB) claims on paper. Start
sending them to us electronically.
When you submit COB claims
electronically, you can edit them
and monitor their status online.
You can also:
n
n
n
necessary COB data. However, if your
billing system can’t send this data
electronically, we have other resources
to help you.
n
R
� eceive quicker payments than
through the mail.
S
� pend less time and money on
administrative tasks.
n
K
� now your claims transactions are
secure and protected.
n
Additional resources to help you
We can accept your COB (secondary)
claims electronically, provided your
practice management system can create
or forward claims that include
L
� og in to our secure provider
website and use our free “Claims
Submission” feature. Claims
submission materials are available in
the “Aetna User Guides” section of
NaviNet Customer Care.
C
� ontact your claims vendor or
clearinghouse for assistance.
S
� ubmit claims directly to us at no
cost via Aetna EDI ConnectSM
(www.aetnaedi.com). This option
is best for technically savvy
submitters.
Why not go totally electronic today?
eEOB tool offers many benefits
The electronic Explanation of Benefits
(eEOB) tool on our secure provider
website is now accessible to all
provider offices.
With this tool, you can turn off paper
EOBs and enroll in electronic funds
transfer (EFT), a fast, secure method of
receiving claims payments. You can also
take advantage of the many eEOB features
listed below.
Advantages of eEOB
Start enjoying the benefits of using this
time- and money-saving tool. You can:
n
n
n
n
n
2
A
� ccess your EOBs 24/7
R
� eceive reimbursement up to one week
faster by using EFT instead of getting
your checks through the mail
O
� rganize records electronically
E
� liminate administrative costs associated
with retrieving paper EOB files
S
� earch by claim, patient, payment
or provider
Aetna OfficeLink Updates
n
A
� ccess claims detail pages and
statements for finalized claims
n
R
� eview real-time claims status
n
S
� ubmit claims reconsiderations online
Win a gift certificate
What’s more, by suppressing paper
EOBs or enrolling in EFT, you’ll have
an opportunity to win a $2,500 Dell™
gift certificate.
To access the tool on our secure
provider website, select “Claim EOB
Tool” from the “Aetna Plan Central”
home page. Then select “Paper Shut
Off” or “EFT Enrollment,” respectively,
and the online forms will appear. If you
don’t see “Claim EOB Tool” on the
home page, contact your office’s NaviNet
security officer to obtain access.
Facilities: Open the door to
electronic communications
Are you a participating facility or
hospital that wants to say “goodbye”
to paper correspondence and
clutter? If so, go to https://aetna.
providerpreference.com/facilities.
php and register to receive electronic
communications from us.
Receiving electronic communications
means you can quickly and efficiently
have critical information from us
at your fingertips – and at your
convenience. Don’t wait for paper
correspondence…sign up today.
�OfficeWise
What’s new on our secure provider website
We’re continually refreshing our secure
provider website to give you access to the
latest tools and resources for doing business
with us. Content updates include:
Clinical Resources
n
n
Doing Business with Aetna
n
n
n
n
A
� dded Aetna Benefits Products
Addendum – new products as of 2008
A
� dded Aetna at a Glance – New
Provider Welcome Kits under Mailings
R
� eplaced Medicare “Zero” Copayments
for Preventive Services and updated
Medicare Vaccine Information for all
Aetna Medicare Advantage Plans
A
� dded new patient safety flyer,
Making health care safer for everyone,
to Behavioral Health page
Claims
n
U
� pdated Preventive Services
Guidelines page
U
� pdated Clinical Practice Guideline for
Antidepressant Prescribing Guide for
Use in Primary Care
Forms Library
n
n
U
� pdated charting aids for Medical
History, Physical Examination, Patient
Progress Notes, Diabetic Foot Health
Screen and Adult Health Maintenance
U
� pdated ERA/EFT Enrollment Packet
Education
n
P
� lease see the feature article in this issue
for recent updates to our Education Site
for Health Care Professionals
U
� pdated Aetna Enhanced Grouper
Information for 2008
Get drug safety alerts online
Physicians can now receive important, time-urgent drug safety alerts online instead of
through the mail.
The Health Care Notification Network (HCNN) is free to physicians and includes no
advertisements or marketing materials. Once you sign up, HCNN will email you alerts
about significant drug-label changes, warnings and recalls. For more information or to
enroll, go to www.hcnn.net
Members may consult
you after using our
hospital comparison tool
The Aetna Navigator® Hospital
Comparison Tool will be available
to you through our secure provider
website in early June.
This interactive tool enables users
to compare hospitals on certain
procedures and diagnoses. It is
already available to Aetna members
through Aetna Navigator, our secure
member website.
We encourage members to review our
health-related information, tools and
resources, and share their findings
with their practitioners. After using
this tool, your Aetna patients may
want to discuss options for hospital
referrals for specific procedures.
View tool on secure website
Once you are on “Aetna Plan
Central,” select “Clinical Resources”
under “Aetna Support Center”
and link directly to the Hospital
Comparison Tool. You can search
more than 150 diagnoses and
procedures to compare over 6,000
hospitals nationwide. Users can print
a report that compares hospitals on
four inpatient measures:
n
T
� he number of patients treated
per year
For the most up-to-date information on the Aetna Medicare Preferred Drug
List, go to: http://www.aetna.com/members/individuals/medicare/member_
assistance/changes.html
M
� ortality rates
n
We update the Aetna Medicare Preferred Drug List, also known as our formulary,
from time to time during the year. As a result, it’s important for prescribing
physicians to reference the Medicare Preferred Drug List to confirm which
prescription drugs are covered under our Medicare plans.
C
� omplication rates
n
Keep track of Medicare formulary changes
n
A
� verage lengths of stay
The report also includes results
from The Leapfrog Group Hospital
Quality and Safety Survey and
data published by the Centers for
Medicare & Medicaid Services.
We contract with WebMD Health
Services to make the Hospital
Comparison Tool available.
JUNE 2008
3
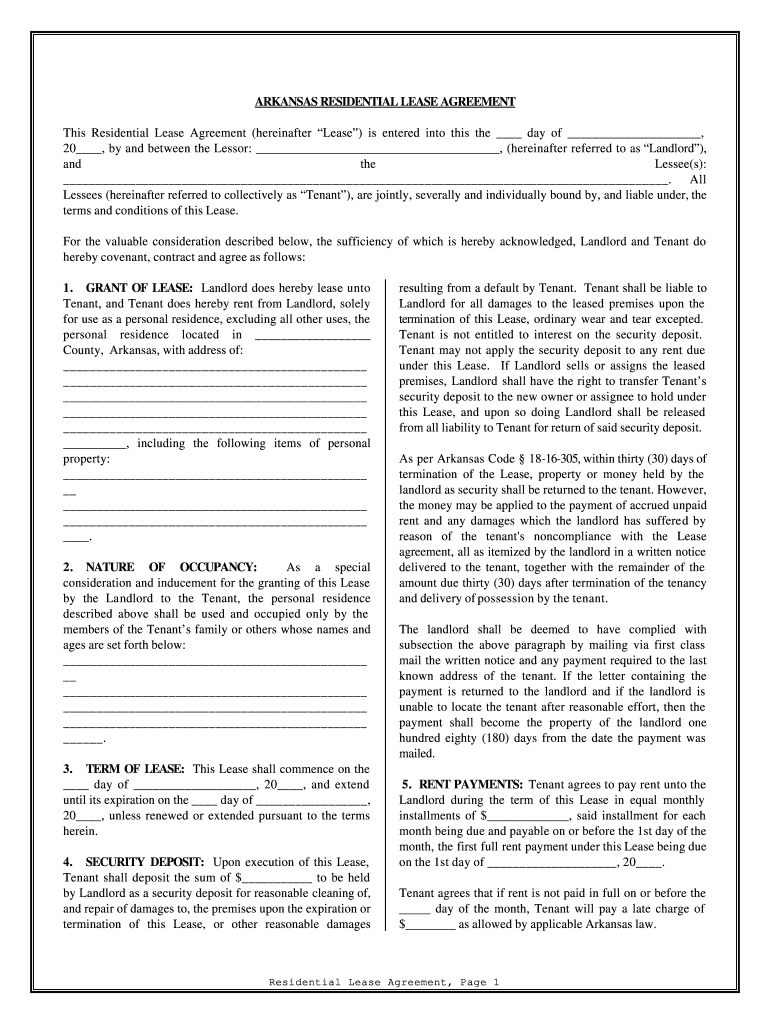
�Policy and Practice Updates
Clinical, payment and coding policy changes
As part of our ongoing policy review process, we regularly adjust our clinical, payment
and coding policy positions. In developing our policies, we may consult with external
professional organizations, medical societies and the independent Physician Advisory
Board, which provides advice to us on issues of importance to physicians.
The accompanying chart outlines coding and policy changes:
codes impacted
Procedure
What’s Changed
Implementation Date
706.0 and 706.1
Chemical
peels,
epidermal
We are changing diagnosis codes 706.0 and
706.1 from covered to not covered in CPB 251 for
chemical peels and epidermal.
September 1, 2008
Oncotype DX® test requires pre-claim review
Artificial disc surgeries
need precertification
For an Oncotype DX test to be covered, you must follow a pre-claim review
process. This will help determine if the patient meets the clinical criteria outlined in
our Clinical Policy Bulletin (CPB) #0352.
Aetna’s Precertification List now
includes a requirement for all artificial
disc surgeries. This provision is in
keeping with our policy that all
inpatient admissions be precertified.
As a reminder, please discuss with your patient the potential test results prior to
testing and agree that the results will be used to guide therapy.
To start the pre-claim review process, call Genomic Health at 1-866-662-6897.
Genomic Health will send you a form to complete and fax back to them.
The patient must meet all conditions listed on the form to be approved for the test,
as stated in our CPB.
Precertification approvals are valid
for six months from the date of
issue, unless stated otherwise.
Precertification requirements apply
to all Aetna plans, except Traditional
Choice® and the Aetna Medicare
OpenSM Plan, our Medicare Private
Fee-for-Service plan.
You can find the necessary criteria for coverage in Clinical Policy Bulletin #0352 at
www.aetna.com.
To view the precertification list, go to
www.aetna.com, select “for Health
Care Professionals” then “Medical.”
How we’re reducing your volume of mail
The next time you get mail from us, it
might look a little different. And, you
may have less mail to open. Maybe you’ve
already noticed the change.
We’re combining all your provider claims
checks, letters and Explanation of Benefits
(EOB) statements, where appropriate, so
your office receives fewer packages from us.
And, in response to your requests, we’ve
reformatted some of our provider EOBs
4
Aetna OfficeLink Updates
and claims letters to make them easier
to read.
In this order, you’ll find:
n
These changes began in mid-May, and are
being implemented for all providers by the
end of June.
Convenient information
For easier viewing of the contents, we’re
grouping similar items together and putting
the most important materials on top.
C
� hecks and remittances
n
E
� OBs
n
C
� laims letters
If you have questions, email us by clicking
the “Contact Aetna” icon on our secure
provider website.
�Aetna’s Education Site for Health Care Professionals
Learning Opportunities From Aetna....Developed With You In Mind
Free webinars are now available
More than 85 percent of health care
professionals responding to our last annual
survey said it would be valuable if we
offered virtual training seminars. Busy
health care professionals often can’t get
away to an in-person educational seminar,
which is why we’ve implemented a series of
ongoing virtual seminars – “webinars.”
We use your feedback to design our
learning opportunities for health care
professionals. Thanks to a dedicated
group of volunteer educators in several
practices and facilities around the country,
we successfully piloted and introduced a
series of new webinars. We also offer select
recorded webinars on our Education Site.
n
- � his 30-minute recorded webinar
T
offers information on handling
coding practices. You’ll learn tools
and tips for accurate and appropriate
coding practices with us.
A
� etna In-Service Updates (Office
A webinar is a virtual educational
seminar offered through the
Internet via your personal computer
and phone line. You can attend our
live or recorded webinars free of
charge at a time that’s convenient
for you from your own office.
administrative updates on key
information available via a live webinar.)
n
Live and recorded webinars your peers
helped design include:
How to enroll in a live or
recorded webinar
- � his 1-hour webinar helps you
T
understand our consumer-driven
benefits plans and how to administer
them using our secure provider
website, supported by NaviNet. The
webinar also focuses on specifics
about our coding policies
and procedures.
New online course offerings
Continuing Education
Recorded Events
Quality Interactions® for New Jersey
physicians (6 CME credits)
Coding Tool Training recorded webinar
Quality Interactions Refresher Course
(Adolescent Health Case)
Office Administration
Tour Aetna’s Secure Provider Website
via NaviNet
What is a webinar?
A
� etna Coding Tool Training
In addition to online courses, we offer
Aetna in-service, face-to-face sessions and
webinars. For upcoming events, see our
online calendar on the Education Site by
visiting our secure provider website and
clicking on the Education link.
n
n
This group gives us feedback on our
educational offerings and helps us create
new, relevant courses. If you would like
to help us continue to shape education
with you in mind, email us with the items
below to AetnaEducationSite@aetna.com:
n
n
n
Pri-Med is a national network of
continuing medical education programs
that offers practicing clinicians world-class
education where you live and work. If
you’ve attended these events, you pay have
noticed Aetna’s participation, supplying
attendees with free patient education
materials that support the doctor-patient
relationship.
T
� o view a recorded webinar
event – search for titles via the
Recorded Events course catalog
Interested in joining our
panel of educators?
n
Supporting the doctor-patient
relationship
To
�� enroll in a “live” webinar
event – click on the calendar to
see upcoming events.
n
n
n
Aetna at Pri-Med
Log in to our secure provider
��
website and select Education.
P
� ractice name
A
� ttention
Street address
C
� ity, state and zip
Phone number
E
� mail address
We’ve handed out materials on subjects
ranging from diabetes and asthma to
cardiovascular health – information that
often reinforces topics covered in the
Pri-Med curriculum.
conference, the highest steppers won prizes
in our “Step It Up” contest. Our physician
winner walked off with a fleece jacket after
totaling over 22,000 steps.
Getting active in Houston
For upcoming Pri-Med events in your area,
see the calendar on the home page of our
Education Site.
We also like to add an element of fun.
Recently, at the Houston Pri-Med, we got
attendees up and walking – literally – by
giving out pedometers. At the end of the
Visit our booth at upcoming Pri-Meds
JUNE 2008
5
�Prescription Medications & Pharmacy Management
Updates to the Aetna Commercial Preferred Drug List
We periodically review the Aetna Preferred Drug List (formulary) to make sure it meets established criteria for safety, effectiveness and
overall value. Recent changes and updates to our formulary are listed below. To view the complete Aetna Preferred Drug List, go to
www.aetna.com/formulary.
Drug
COverage update
precertification
step-therapy
quantity
limits
FORMULARY ADDITIONS
Renvela Tab® (sevelamer carbonate)
Preferred (P)
Tekturna HCT® (aliskerin hydrochlorothiazide)
P
X
Alendronate
P
X
Olux-Olux E® Complete Pack (clobetasol prop foam and
clobetasol emul foam pack)
P
Humira® Kit 20 mg/0.4 ml (adalimumab inj kite 20 mg/0.4 ml)
Preferred Pharmacy Managed
Self-Injectable (P-PMSI)
FORMULARY Removals
Fosamax® (alendronate)
Formulary Excluded (FE)
X
NEW DRUGS – Nonpreferred (NP) or FE
Ibudone™ (hydrocodone/ibuprofen)
FE
Pad®
NP
Lidamantle HC
acetate pad 2-2%)
(lidocaine/hydrocortisone
Intelence™(etravirine)
NP
Allegra® ODT (fexofenadine)
FE
X
Luvox®
CR (fluvoxamine maleate SR)
X
X
FE
Simcor® (niacin/simvastatin)
FE
Evamist™ (estradiol transdermal spray)
FE
Lamisil® granules (terbinafine oral granules)
FE
X
NP
Fenoglide™ (fenofibrate)
X
X
FE
Dazidox™ (oxycodone hcl)
X
X
X
Medications may be covered at a higher copayment or removed from our formulary after appropriate notification to providers and affected members.
As brand-name medications lose their patents and generic versions become available, the brand-name medication may be covered at a higher copayment and/or may be added to the
Formulary Exclusions List for commercial closed formulary plans.
The Aetna Preferred Drug List may change because the Food and Drug Administration approves many new medications throughout the year, or medications may be withdrawn from the
market or become available without a prescription. When an over-the-counter equivalent becomes available, the prescription medication may no longer be covered under many of Aetna’s
commercial pharmacy benefits plans.
California HMO members receiving coverage for medications added to the Formulary Exclusions, Precertification or Step-Therapy lists will continue to have those medications covered, as
long as the treating physician continues prescribing them, provided that the drug is considered safe and effective for treating the member’s medical condition.
Texas members: if currently covered, full-risk members will continue to have medications that are removed from the Preferred Drug List covered at the same benefit level until their plan’s
renewal date. The term “precertification” does not mean a reliable representation of payment of care or services to fully insured HMO and PPO members.
Some programs, such as step-therapy, precertification and quantity limits are not available in all service areas. Precertification programs do not apply in Indiana. Step-therapy does not
apply to fully insured members in Indiana and New Jersey. Members should refer to their plan documents or call the Member Services number on their ID card.
New billing requirement for Ceftriaxone
Beginning September 1, 2008, Aetna will
no longer routinely pay Ceftriaxone claims
that fall above these dosing levels:
n
6
A
� dults: Total daily dose should not
exceed 4 grams (16 units). Daily dose
is usually 1 to 2 grams given once a day
(or in equally divided doses twice a day),
depending on the type and severity
of infection.
Aetna OfficeLink Updates
n
C
� hildren (age 12 and under): Total
daily dose should not exceed 2 grams (8
units). Total daily dose is usually 50 to
75 mg/kg given once a day (or in equally
divided doses twice a day).
You should bill for Ceftriaxone using code
J0696 with a unit of 1 for each 250 mg of
Ceftriaxone administered.
This billing change results from a claims
review where we found some instances of
incorrect billing for single doses that are
substantially above levels recommended
by the FDA-approved product labeling.
These amounts are recommended by the
United States Pharmacopoeia Dispensing
Information (USPDI) and the American
Society of Health-System Pharmacists
(ASHP) (drug information).
�Physician Focus™
2008 and Beyond: Aetna’s Commitment to
Physician Relations
A message from
Troyen A. Brennan, M.D.,
Aetna Chief Medical Officer
The Physicians Settlement Agreement with Aetna ends this June. But the agreement’s
formal expiration has no impact on the way we will continue working with
physicians. All of the changes Aetna made as part of the settlement agreement are
embedded in our business model. They are in our DNA and serve as a foundation
for what we anticipate will be future collaborations with the medical community to
make health care safer and more effective.
We have worked hard to strengthen physician relations. Over the last few years, we
have established a level of trust with health care professionals and expect to build on
that in the years ahead. We want to continue to be a high-integrity business partner
with the medical community. We also understand that we must demonstrate that
commitment not only through words, but actions.
With the settlement agreement about to end, Aetna proactively reached out to
state medical societies to share our commitment to continuing virtually all of the
provisions contained in the settlement. The only provisions we are not continuing
are a few administrative details that have outlived their usefulness. For example, the
annual compliance report has become obsolete, since we now address and resolve
issues face to face with the medical societies.
We also have established Guiding Principles for Physician Relations that formally
define Aetna’s genuine desire to building the best possible relationships with the
medical community. The document identifies specific behaviors and business actions
that govern Aetna in its interactions with health care professionals. It also outlines
business practices we will maintain including simplified business transactions,
increased transparency of policies and processes, and working with the medical
community to encourage adherence to evidence-based guidelines in medicine.
These Guiding Principles clearly demonstrate, in writing, that we are serious
about making it even easier to do business with us and moving forward
with the medical community with a shared focus – improving outcomes
for patients.
“� e want to continue to be
W
a high-integrity business
partner with the medical
community.”
For a copy of Aetna’s Guiding Principles for Physician Relations, go to our public
website at http://www.aetna.com/provider/medical/join_med/advantages_med/
advantage.html.
Aetna also will continue the Physician Advisory Board, and will consult with the
Physicians Advocacy Institute, the organization funded by the medical societies to
ensure that payers are behaving reasonably.
Sincerely,
Troyen A. Brennan, M.D.
Senior Vice President and
Chief Medical Officer
JUNE 2008
7
�Plan Facts and Features
Benefits of
immunization registries
Plain language materials help members with asthma
Immunization registries are confidential,
computerized databases used to maintain
immunization records on a statewide basis.
Aetna last year began a study to see if
clearer, simpler health information could
help members with asthma understand
and better manage their disease.
Preliminary results indicate that
easier-to-read health information can
improve patients’ knowledge about
asthma and how to control it.
How we conducted the study
Members were placed in either a control
or outreach group. We then measured
each group’s baseline knowledge of
asthma. The outreach group received
information about asthma written in
updated “plain language” while the
control group received standard materials.
The materials written in “plain language”
have shorter sentences and words
that are familiar to people without
medical training.
Preliminary results and next steps
At one-month follow-up, members who
received the “plain language” asthma
materials scored higher on the knowledge
survey than those in the control group.
Follow-up studies will determine
if members retain long term the
information they learned about asthma
care and control. We’ll also look at
whether improved knowledge results in
better medication compliance and
health outcomes.
Participating in an immunization registry
can help your office by:
n
n
n
An award-winning study
The Institute for Healthcare
Advancement (IHA) recognized our
efforts to promote health literacy and
better health outcomes. The asthma
health literacy study was selected as
the winner in the Research Category
in the IHA’s Health Literacy Awards
competition.
n
n
n
We’ve simplified our
Aexcel®
We continue to improve and strengthen
our Aexcel designation process to make
it more understandable for members
and physicians. Beginning this year,
physicians in Aexcel specialties will
be evaluated for efficiency using one
methodology – the Symmetry Episode
Treatment Groups®. We previously used
two methodologies when evaluating a
physician’s efficiency of care.
n
n
8
F
� or 2008, we will exclusively use the
Symmetry methodology in markets
that will introduce Aexcel in 2009 and
in existing markets whose two-year
Aexcel re-designation review occurs
in 2008.
F
� or 2009, this change will apply to
markets introducing Aexcel in 2010
and to the remaining existing markets
whose Aexcel re-designation review
occurs in 2009.
Aetna OfficeLink Updates
efficiency methodology
Why we use one methodology
Our experience shows that Symmetry
produces more year-to-year consistency
in determining which physicians
are efficient, compared to using two
methodologies. In addition, using
one methodology simplifies review
of performance measurement results
for physicians and streamlines our
evaluation process.
Symmetry is also integrated with our
other provider performance initiatives,
such as Provider Quality Performance
ProgramSM (formally known as
Pay-for-Performance). This helps
ensure we are using a standard,
consistent methodology when evaluating
and measuring provider performance
across all programs.
n
P
� roviding a reliable immunization history
about your patients, helping to eliminate
duplicate immunizations if patients
previously saw other providers.
I
� mproving office efficiency by
consolidating immunization information
in one source.
S
� implifying completing the proof-ofimmunization paperwork for your
patients’ school, camp and daycare
admission requirements.
E
� nhancing quality of care by
generating appointment reminders for
immunizations that are due or overdue.
A
� utomatically recording vaccine
manufacturer and lot number for each
patient, which can help identify patients
for revaccination in cases of recalled
vaccine lots.
R
� educing the need for your office to
obtain documentation during HEDIS
data collection.
P
� roviding safe storage of data in case of
an office disaster or lost records.
Go to www.cdc.gov/vaccines/programs/
iis/default.htm to locate your state’s
immunization registry and for information
on how you can participate.
Aetna’s depression
screening program
The Aetna Depression Management
Program provides resources for primary
care physicians (PCPs) to help diagnose
and treat patients with depression.
We also offer PCP offices participating in
this program additional compensation for
screening Aetna members for depression.
To learn more or to participate,
call 1-888-812-3862 or email us at
depression@aetna.com. You can go to
www.aetnadepressionmanagement.com
to register for the program, tour program
highlights and find printable office tools.
�Striving for Quality Excellence
Keeping you informed: NCQA-required notification
The National Committee for Quality
Assurance (NCQA) requires health plans
to inform physicians of certain policies,
standards and programs annually,
including:
n
n
n
Members’ rights and responsibilities
C
� ase management and disease
management programs and how
members and providers can
access them
Information on advance directives
You’ll find information on these
and other topics in our Health Care
Professional Toolkit, available online
through our secure provider website.
Medical practices without Internet access
can request a paper copy by calling our
Provider Service Center.
Advance directives
QI program information
The Centers for Medicare & Medicaid
Services requires that information on
whether a member has prepared an
advance directive be documented in
your Medicare patients’ charts. Aetna
Participating Practitioner Medical Record
Criteria require that documentation
about advance directives (whether
executed or not) is in a prominent place
in the patient’s record (except for patients
under age 18).
If you want information on our Quality
Improvement (QI) program goals, call
our Provider Service Center. These
goals include:
Advance directive forms for
specific states are posted on
www.aetnacompassionatecare.com.
If the state you practice in is not listed,
you or your patients can visit
www.uslivingwillregistry.com/forms.
shtm for an advance directive form or for
additional information.
n
n
n
M
� easuring, monitoring and achieving
optimum performance of clinical and
service quality.
I
� mplementing a program that is
responsive to members’ health
care needs.
�Complying with requirements of
benefits plans, plan sponsors, federal
and state regulators, and appropriate
accrediting bodies.
New HEDIS® documentation requirements for DTaP
Coverage determinations
and utilization management
HEDIS 2009 requires that for immunizations given in 2006, 2007 and 2008,
health plans must now confirm in the medical record that members received
the acellular pertussis (aP) vaccination, in addition to the diphtheria and tetanus
(DT) vaccinations.
Aetna uses evidence-based clinical
guidelines from nationally recognized
authorities to guide utilization
management (UM) decisions.
To help us with HEDIS reporting, we ask that the member’s medical record
clearly indicate that the DTaP vaccine was given and the date. Charting aids that
display multiple vaccines together, such as DTaP/DTP/DT, are not acceptable.
A Pediatric Vaccine Record form that meets HEDIS documentation standards is
posted on our secure provider website.
If your patients got a DTaP vaccine in 2006 or 2007 and your office used a
charting aid that grouped DTaP, DTP and DT together, please circle DTaP so
we know that vaccine was administered.
Accessing the vaccine record form
To access the Pediatric Vaccine Record form from our secure provider website,
select “Aetna Support Center,” “Forms Library” and “Pediatric Vaccine Record”
under “Member Health Information Forms/Charting Aids.”
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA).
Specifically, we review any request for
coverage to determine if the member
is eligible for benefits, if the service
requested is a covered benefit under
the member’s plan and if the service is
delivered consistent with established
guidelines. If a coverage request is
denied, the member (or a physician
acting on the member’s behalf) may
appeal this decision through our
complaint and appeal process.
Staff conducting UM activities assist
members in accessing services covered
under their plans. We do not reward
physicians or individuals who conduct
utilization review for creating barriers to
care or for issuing denials of coverage.
You can find more about our utilization
review policies on our website.
Aetna OfficeLink Updates
JUNE 2008
9
�Northeast News
Online pricing information available for additional
health care specialties
Along with pricing information for
participating physicians, beginning in
June our price transparency tool will
include pricing information for
these specialists:
n
Physical therapists
n
Occupational therapists
n
Speech therapists
n
Speech pathologists
n
Audiologists
n
Chiropractors
n
Podiatrists
n
Members in areas where this tool is
available can view rates for office visits
with these professionals. Depending
on the specialty, rate information may
also be available for diagnostic tests,
as well as for major, minor and other
procedures.
Optometrists
The unit price transparency tool is
available to members through our
secure member website and helps them
make more informed, cost-effective
decisions about their health care.
Consultative services available through Vital Decisions1
We are pleased to support physicians with
access to a new service to help patients with
chronic and complex illnesses, or end-oflife decisions. Vital Decisions is a health
care counseling service that helps patients
who are facing difficult medical situations
make well-informed health care choices.
Helping you help your patients
For physicians striving to help their
patients create an effective advance care
plan, it can be helpful to have a health
care/bioethics counselor who can assist in
setting realistic care goals.
The Vital Decisions service includes
ethicists, nurses, physicians, social workers
and other professionals with extensive
experience in bioethics/health care
consultation. The telephone-based service
provides information and tools to help the
patient and his/her family:
n
U
� nderstand the patient’s medical
situation and prognosis.
10
Aetna OfficeLink Updates
n
n
n
C
� larify medical, ethical and legal issues
relating to treatment and the setting of
realistic care goals.
Here’s how to learn more
E
� xplore options to help the responsible
parties arrive at the best plan of care for
the patient.
Visit the Vital Decisions website at
www.vitaldecisions.net or contact them at
973-379-0079. To refer a member for this
service, complete a Counseling Request
Form on the website.
C
� ustomize care by matching the medical
choices to the individual’s personal goals,
preferences and values.
You may also contact Aetna Medical
Director Ira Klein, M.D., M.B.A.,
F.A.C.P, at 908-369-0818 with questions.
The service is a fully covered member
benefit, with the Vital Decisions counselor
remaining a 24/7 resource for the patient
throughout the entirety of their illness.
While referrals can be requested by either
a physician, member or a member’s
representative, the Vital Decisions
counselor will always contact the attending
physician about any impending consult.
Recommendations or guidance offered
during the consultation are advisory, with
the patient’s physician directing the course
of care.
Vital Decisions is a contracted entity, and is
not otherwise affiliated with Aetna. Aetna is not
responsible for any advice or actions taken by
Vital Decisions.
1
�Don’t just think outside the box.
Think outside the mailbox.
Close the mailbox and open your inbox.
Get information electronically from
Aetna through email instead of in a
paper format in your mailbox.
Visit https://aetna.providerpreference.com
Sign up today
for our
electronic
correspondence
option.
JUNE 2008
11
�PRSRT STD
U.S. POSTAGE
PAID
PERMIT NO. 12
ENFIELD, CT
CPE RS51
151 Farmington Ave.
Hartford, CT 06156
Contact us at: OfficeLinkUpdates@aetna.com
Please route this publication to:
q Office Manager
q Business Staff
q Front Desk Staff
q Medical Records/Medical Assistants
q Primary Care Physicians
q Specialists
q Physician Assistants/Clinical
Nurse Specialists
q Nurses
q Referral and Precertification Stafftaff
Aetna is the brand name used for products and services provided by one or more of the Aetna group of subsidiary companies. The
Aetna companies that offer, underwrite or administer benefits coverage include Aetna Health Inc., Aetna Health of California Inc.,
Aetna Life Insurance Company and Corporate Health Insurance Company and Strategic Resource Company.
Register for NaviNet website to get clinical alerts
Our improved secure provider website
via NaviNet has many new features and
enhancements, including important
“Care Considerations” for your Aetna
patients. However, you can’t review
online Care Considerations if you aren’t
registered with NaviNet.
Supporting patient care
Care Considerations are clinical alerts
based on a member’s claims history.
MedQuery®, administered by our
subsidiary ActiveHealth Management,
compares a member’s pharmacy,
laboratory and medical claims against
clinical algorithms derived from
published medical evidence and
guidelines recommended by professional
organizations. Care Considerations
identify potential gaps in care and
bring these to the attention of the
treating physician.
Most Care Considerations pertain
to disease and drug interactions; tests,
medications or monitoring patient needs
based on an existing health condition;
and preventive care or screenings that
are overdue. Physicians can use this
information to adjust a treatment
plan or suggest the patient schedule a
recommended test or screening.
Receiving Care Considerations
Once you are registered, Care
Considerations will display in your
NaviNet Action Items and as an “alert”
within an electronic eligibility response.
Your office may want to establish a
workflow to review and respond to
online Care Considerations.
To register for NaviNet, go to
www.aetna.com. Select “for Health
Care Professionals,” “Medical,” then
“Register Now!” from the “Provider
Secure Website” box on the right.
The information and/or programs described in this newsletter may not necessarily apply to all services in this region. Please contact your Aetna
network representative to find out what is available in your local network. Application of copayments and/or coinsurance may vary by plan design.
This newsletter is provided solely for your information and is not intended as legal advice. If you have any questions concerning the application or
interpretation of any law mentioned in this newsletter, please contact your attorney.
23.22.807.1-NE (6/08)
©2008 Aetna Inc.
�