European Heart Journal Advance Access published September 9, 2010
CLINICAL RESEARCH
European Heart Journal
doi:10.1093/eurheartj/ehq324
Impaired microcirculation predicts poor
outcome of patients with acute myocardial
infarction complicated by cardiogenic shock
Corstiaan A. den Uil 1*, Wim K. Lagrand 2, Martin van der Ent 1,
Lucia S.D. Jewbali 1, Jin M. Cheng 1, Peter E. Spronk 3, and Maarten L. Simoons 1
1
Department of Cardiology, Thoraxcenter, Erasmus Medical Center, Room V-017, s-Gravendijkwal 230, Rotterdam NL-3015 CE, The Netherlands; 2Department of Intensive Care
Medicine, Academic Medical Center, Amsterdam, The Netherlands; and 3Department of Intensive Care Medicine, Gelre Hospitals, Apeldoorn, The Netherlands
Aims
We investigated the relationship between sublingual perfused capillary density (PCD) as a measure of tissue perfusion
and outcome (i.e. occurrence of organ failure and mortality) in patients with cardiogenic shock from acute myocardial
infarction.
.....................................................................................................................................................................................
Methods
We performed a prospective study in 68 patients. Using Sidestream Dark Field imaging, PCD was measured after
hospital admission (T0, baseline) and 24 h later (T1). We compared patients with baseline PCD ≤ median to patients
and results
with baseline PCD . median. Sequential organ failure assessment (SOFA) scores were calculated at both time points.
The Kaplan –Meier 30-day survival analyses were performed and predictors of 30-day mortality were identified. The
baseline PCD was a predictor of the change in the SOFA score between T0 and T1 (DSOFA; r ¼ 20.25, P ¼ 0.04).
Organ failure recovered more frequently in patients with PCD . median (.10.3 mm mm22; n ¼ 33) than in patients
with PCD ≤ median (n ¼ 35; 52 vs. 29%, P , 0.05). Twenty-two patients (32%) died: 17 patients (49%) with PCD ≤
median vs. 5 patients (15%) with PCD . median (P ¼ 0.004). After adjustment, the cardiac power index [odds ratio
(OR): 0.48, 95% CI: 0.24– 0.94) and PCD (OR: 0.65, 95% CI: 0.45 –0.92) remained significant predictors of 30-day
outcome. Patients with baseline sublingual PCD ≤ median that improved at T1 had a considerable better prognosis
relative to patients who had a persistently low PCD.
.....................................................................................................................................................................................
Conclusion
Diminished sublingual PCD, at baseline or following treatment, is associated with development of multi-organ failure
and is a predictor of poor outcome in patients with acute myocardial infarction complicated by cardiogenic shock.
----------------------------------------------------------------------------------------------------------------------------------------------------------Keywords
Cardiogenic shock † Microcirculation † Organ failure † Outcome † Perfusion
Introduction
Cardiogenic shock is the most important cause of death in patients
hospitalized with acute myocardial infarction.1 Although in-hospital
survival of cardiogenic shock is improving with more intensive
treatment, 30-day mortality rate remains high.2,3 Because cardiogenic shock is caused by extensive myocardial infarction and a
decrease in cardiac output, timely reperfusion and normalization
of haemodynamic parameters are the main objectives in the treatment of cardiogenic shock.4 However, it has been shown that 45%
of patients dying from cardiogenic shock have a preserved cardiac
index (CI), indicating that optimization of macro-haemodynamic
parameters alone may fail to save the patient.5,6 In line with
these data, post hoc analysis of data from the SHOCK trial demonstrated that the classic notion of systemic vasoconstriction as a
response to low arterial pressure did not apply to all patients
with cardiogenic shock. Indeed, a large variability in CI and systemic
vascular resistance (SVR) has been reported among patients with
cardiogenic shock, even despite application of vasopressor
therapy.7 These data indicate that cardiogenic shock is a primarily
cardiac problem leading to subsequent derangements in the entire
circulatory system.8 It is currently accepted that cardiogenic shock
* Corresponding author: Tel: +31 614673334, Fax: +31 10 70 32890, Email: c.denuil@erasmusmc.nl
Published on behalf of the European Society of Cardiology. All rights reserved. & The Author 2010. For permissions please email: journals.permissions@oxfordjournals.org.
Downloaded from http://eurheartj.oxfordjournals.org/ by guest on September 6, 2014
Received 8 April 2010; revised 2 July 2010; accepted 23 July 2010
�Page 2 of 8
blood pressure , 90 mmHg) induced by heart failure together with
the clinical signs of hypoperfusion (i.e. cold extremities, oliguria, or
altered mental state), not responsive to fluid resuscitation.4 The institutional ethical committee approved the protocol, and written
informed consent was obtained from each patient or, in the case of
patients who were sedated, from a relative authorized to consent on
behalf of such a patient.
Haemodynamic monitoring
All patients were monitored with a radial artery catheter (arterial
cannula with FloSwitch, Ohmeda, Swindon, UK). Forty-eight (71%)
patients were monitored with a pulmonary artery catheter (PAC:
Becton Dickinson Criticath SP5107H, Sandy, UT, USA, or CCOmbo,
Edwards Lifesciences, Saint-Prex, Switzerland). In the remaining
patients, central venous pressure (CVP) was measured via a threelumen central venous catheter (Multicath; Laboratoires Pharmaceutiques Vygon, Ecouen, France), inserted into the right internal jugular
vein. In these patients, CI was calculated according to the Cuschieri
formula, which shows close correlation with the CI measured with a
PAC.19
Data collection
Methods
Study design
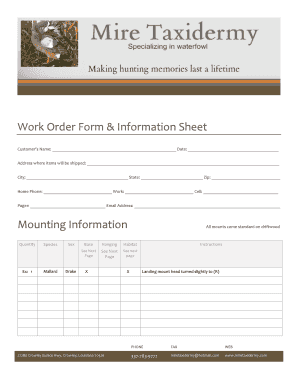
This prospective study was conducted at the Intensive Cardiac Care
Unit (ICCU) of the Thoraxcenter, Erasmus University Medical
Center, Rotterdam, the Netherlands. We included patients who
were admitted with acute myocardial infarction complicated by cardiogenic shock in the time period November 2007 –April 2009 (Figure 1).
Cardiogenic shock was defined as sustained hypotension (systolic
Data collection included central body temperature, heart rate, mean
arterial pressure (MAP), CVP, pulmonary capillary wedge pressure
(PCWP), mean pulmonary artery pressure, CI, SVR, lactate level, and
mixed-venous oxygen saturation (SvO2). When no PAC was available,
we estimated SvO2 by measuring venous oxygen saturation from
blood sampled from the central venous line. Systemic vascular resistance was calculated as (MAP 2 CVP) × 80/cardiac output. Cardiac
power index (CPI) was computed as MAP × CI/451. Glomerular filtration rate was estimated by the modification of diet in renal
disease equation.
Figure 1 Study flow chart. STEMI, ST-segment elevation myocardial infarction.
Downloaded from http://eurheartj.oxfordjournals.org/ by guest on September 6, 2014
causes a systemic inflammatory response (SIRS), which is characterized by the release of inflammatory mediators and neurohormones as well as by alterations in tissue microvasculature, which
may result in multi-organ failure.9,10 Indeed, several studies have
reported that markers of SIRS are predictive of short-term mortality in cardiogenic shock.11 – 14 Nevertheless, the mechanisms
involved in the pathogenesis of multiple organ failure in cardiogenic
shock patients remain largely unknown. Possibly impaired splanchnic perfusion at the microvascular level, modulated by the severity
of heart failure, by the degree of SIRS, and by the administration of
vasoactive agents, plays an important role in the pathogenesis of
multi-organ failure and the persistence of shock.15,16
Sublingual microcirculation is a surrogate marker of splanchnic
perfusion and can be measured at the bedside using the novel
imaging technology.16 – 18 Therefore, we investigated the relationship between sublingual microcirculation and outcome [i.e.
(change in) sequential organ failure assessment (SOFA) score,
occurrence of multi-organ failure, and mortality] in patients with
acute myocardial infarction complicated by cardiogenic shock.
C.A. den Uil et al.
�Page 3 of 8
Impaired microcirculation predicts poor
Statistical analysis
The Sidestream Dark Field (SDF) imaging device (MicroScan; Microvision Medical, Amsterdam, the Netherlands) was used to obtain
two-dimensional video images of sublingual microcirculatory blood
flow as described previously.20 In short, the camera emits green
light that is absorbed by red blood cells within microvessels. In this
way, red blood cells are used as the contrast agent to visualize sublingual blood flow in patent microvessels. Per time point, 3– 5 steady
video sequences of at least 20 s duration were obtained, stored, and
analysed in a randomized and blinded fashion. Quantification of the
images was done using dedicated software (Automated Vascular
Analysis 3.0, Microvision Medical) by a blinded investigator. Perfused
capillary density (PCD) was calculated by measuring total length of
perfused capillaries divided by the image area. Capillaries were
regarded as perfused if they had either of the following flow classifications obtained by visual inspection: sluggish, continuous, or hyperdynamic.21,22 Unperfused capillaries (i.e. capillaries with absent or
intermittent perfusion) were judged not to take part of the circulation and were not taken into account. Since SDF imaging enables
visualization of flowing intravascular erythrocytes rather than
microvessel walls, an increase in PCD was regarded as capillary
recruitment. This approach has been validated previously and withinpatient variability and inter- and intra-observer variability of the technique are low.23 – 25 Capillaries were defined as microvessels with a
diameter ,20 mm. Reference values for sublingual PCD in control
patients (i.e. patients awaiting cardiac surgery who were not in
shock) have been reported previously, i.e. ≥11.7 mm mm22 (2.5
percentile).26,27
Image acquisition is particularly comfortable in patients who are
sedated and intubated, whereas in patients who are awake, movement
of the tongue may more easily result in movement artefacts. However,
we and other investigators extensively reported the feasibility of using
this device in critically ill patients in several reports albeit in research
settings.25,28 – 30 In addition, Arnold et al. 30 recently compared a realtime point-of-care (POC) determination of the microcirculation to
conventional off-line analysis. The POC assessment of microcirculation
was 94% sensitive and 92% specific for detecting impaired microvascular flow.
Statistical analyses were performed using SPSS 15.0 for Windows. Categorical variables are presented as absolute numbers with percentages.
Continuous variables are presented as mean + standard deviation.
Non-normally distributed continuous variables are presented as
median (interquartile range). Because this study is the first study that
presents PCD measurements in patients with cardiogenic shock, we
decided a priori to compare the patients with baseline sublingual
PCD ≤ median with the patients in whom baseline sublingual PCD
was .median. Categorical variables were compared by the chi-square
test or Fisher’s exact test, when appropriate. Differences between
groups were tested with Student’s t-test or the Mann – Whitney test,
when appropriate. Changes between time points were tested with
the paired t-test or Cochran’s Q-test, when appropriate. Correlations
between variables were investigated with the Pearson or the Spearman
correlation test, when appropriate. The Kaplan –Meier cumulative
30-day survival was calculated, and the Kaplan – Meier survival curves
were compared by the log-rank test. Univariate and multivariate logistic regression analyses were performed to identify predictors of 30-day
all-cause mortality. Final results are presented as unadjusted and
adjusted odds ratios (OR) and 95% confidence intervals (95% CI).
The multivariate logistic regression model selection was done with a
backward stepwise method starting with the following variables: age
.75 years, CPI, baseline SOFA score, nitroglycerine, left main coronary artery occlusion, left ventricular ejection fraction ,30%, significant
mitral valve regurgitation, and sublingual PCD. Variables that remained
significantly associated with 30-day mortality were part of the
regression equation and are presented. The multivariate model was
confirmed by using the forward stepwise selection. We selected the
variables based on differences in baseline characteristics among both
subgroups and on previous reports on prognosticating factors in cardiogenic shock.25,26,33 – 35 Given our hypothesis, we further added sublingual PCD and baseline SOFA score, which consists of multiple
variables itself, including inotropic and vasopressor support. Sublingual
PCD was entered into the model as a continuous variable. The cardiac
power index was categorized into units of 0.10 W m22.33 All tests
were two-sided. A P-value of ,0.05 was regarded statistically
significant.
Study protocol
Results
The sublingual microcirculation was investigated as soon as possible
after the patient’s admission to the ICCU and after informed
consent had been obtained (T0, baseline). Measurements were
repeated 24 h after the first measurement or earlier, pending the individual clinical course of the patient (i.e. significant deterioration which
might lead to death within 24 h). In addition, at both time points, all
components of the SOFA score were calculated, with the exception
of the central nervous system parameters, because the majority of
the patients received central nervous system depressant drugs at the
time of evaluation.14,31 The total SOFA score was calculated by
summing the scores for each of the components (i.e. cardiac, renal,
respiratory, coagulation, and liver).32
Follow-up
Vital status at 30 days was registered for all patients. In patients who
were transported to other hospitals or were discharged during the
30 days following baseline measurements, vital status was acquired
from municipal civil registries. The response rate was 100% and no
patients were lost during 30 days of follow-up.
We investigated 68 patients with acute myocardial infarction complicated by cardiogenic shock; 47 patients had a STEMI and 21
patients had a non-STEMI (Figure 1, Table 1). Mean age was
60 + 14 years and 69% of the patients were male. Ninety-seven
per cent of the patients still met the inclusion criteria during baseline measurements. The remaining patients (n ¼ 2) received high
dosages of vasopressors, which resulted in systolic blood pressures
.90 mmHg. Median PCD was 10.3 mm mm22 (range: 4.3–
15.9 mm mm22; please note the Supplementary material online
for video samples of high- and low-sublingual PCD). Patients
with PCD ≤ median (n ¼ 35) were less frequently .75 years
when compared with patients with sublingual PCD . median
(n ¼ 33; 9 vs. 30%, P ¼ 0.03, Table 1). Patients with PCD ≤
median more frequently had an ejection fraction ,30% (74 vs.
42%, P ¼ 0.01). The median baseline SOFA score was not significantly different between both groups. Patients with a PCD ≤
median had a higher PCWP [23 (18 –25) vs. 18 (14 –22) mmHg,
P ¼ 0.04] than those with a PCD . median (Table 2).
Downloaded from http://eurheartj.oxfordjournals.org/ by guest on September 6, 2014
Microcirculatory assessment and analysis
�Page 4 of 8
Table 1
C.A. den Uil et al.
Baseline characteristics
All patients (n 5 68)
PCD ≤ mediana (n 5 35)
PCD > mediana (n 5 33)
P-value
...............................................................................................................................................................................
Age (years; mean + SD)
60 + 14
59 + 12
62 + 15
0.24
Age . 75 years [n (%)]
Gender [male; n (%)]
13 (19)
47 (69)
3 (9)
24 (69)
10 (30)
23 (70)
0.03
0.99
Proportion of patients still meeting inclusion
criteria during baseline measurementsb [n (%)]
66 (97)
34 (97)
32 (97)
0.99
...............................................................................................................................................................................
CV risk factors [n (%)]
Hypertension
27 (40)
11 (31)
16 (49)
0.22
Diabetes mellitus
Current smoking
21 (31)
16 (24)
12 (34)
10 (29)
9 (27)
6 (18)
0.61
0.4
Dyslipidaemia
18 (27)
9 (26)
9 (27)
0.99
21 (31)
11 (31)
10 (30)
0.99
47 (68)
24 (69)
23 (70)
...............................................................................................................................................................................
Electrocardiography [n (%)]
Non-STEMI
...............................................................................................................................................................................
Laboratory [median (IQR)]
Haemoglobin (mmol L21)
WBC count (×109 L21)
CRP (mg L21)
6.6 (5.9– 7.7)
11.9 (9.8– 17.3)
6.6 (5.8–7.7)
12.9 (9.8–18.0)
6.6 (6.0–7.7)
11.4 (8.8–17.1)
0.78
0.35
55 (15– 138)
55 (18–136)
49 (9– 149)
0.81
GFR (mL min21)
NT-proBNP (pg mL21)
58 (37– 83)
3775 (1316–9140)
55 (39–77)
4127 (1958– 10,873)
66 (33–90)
2839 (1186– 8653)
Peak creatine kinase (U L21)
3455 (403–6786)
3891 (355–7221)
3093 (413– 5948)
0.47
5.7 (1.2– 12.9)
7.8 (1.8–13.4)
4.0 (0.6–13.8)
0.54
Echocardiography [n (%)]
Ejection fraction , 30%
40 (59)
26 (74)
14 (42)
0.01
Moderate-severe MR
17 (25)
10 (29)
7 (21)
0.58
No angiography
One-vessel disease
6 (9)
17 (25)
4 (11)
7 (20)
2 (6)
10 (30)
0.67
Two-vessel disease
15 (22)
7 (20)
8 (24)
Three-vessel or LM disease
Occlusion of LM
30 (44)
15 (24)
17 (49)
8 (26)
13 (39)
7 (23)
Peak Troponin T (mg L21)
0.55
0.54
...............................................................................................................................................................................
...............................................................................................................................................................................
Angiography [n (%)]
0.99
...............................................................................................................................................................................
Treatment [n (%)]
ASA
67 (99)
35 (100)
32 (97)
0.49
Clopidogrel
UFH/LMWH
52 (77)
68 (100)
28 (80)
35 (100)
24 (73)
33 (100)
0.57
0.99
GP IIb/IIIa inhibitors
10 (15)
5 (14)
5 (15)
0.99
Enoximone and/or dobutamine and/or
dopamine ≤ 5c
27 (40)
16 (46)
11 (33)
0.31
Dopa . 5 or Norepi ≤ 0.1c
Dopa . 15 or Norepi . 0.1c
16 (24)
15 (22)
6 (17)
8 (23)
10 (30)
7 (21)
Nitroglycerine
Mechanical ventilation
IABP
ECMO
Revascularization [n (%)]
No revascularization
Thrombolysis
PCI
CABG
TIMI flow after PCI
9 (13)
7 (20)
2 (6)
0.15
49 (72)
30 (44)
22 (63)
18 (51)
27 (82)
12 (36)
0.11
0.23
3 (4)
1 (3)
2 (6)
0.61
14 (21)
6 (17)
8 (24)
0.74
0 (0)
0 (0)
0 (0)
49 (72)
5 (7)
26 (74)
3 (9)
23 (70)
2 (6)
3 (3–3)
3 (3– 3)
3 (3– 3)
0.22
Continued
Downloaded from http://eurheartj.oxfordjournals.org/ by guest on September 6, 2014
STEMI
�Page 5 of 8
Impaired microcirculation predicts poor
Table 1 Continued
All patients (n 5 68)
PCD ≤ mediana (n 5 35)
PCD > mediana (n 5 33)
P-value
...............................................................................................................................................................................
SOFA score [median (IQR)]
Total
Cardiac subscore
5 (4– 7)
2 (2– 3)
5 (3 –8)
2 (2 –3)
6 (4 –7)
3 (2 –3)
0.96
0.65
Renal subscore
1 (0– 1)
1 (0 –1)
0 (0 –2)
0.7
Respiratory subscore
Coagulation subscore
1 (1– 2)
0 (0– 1)
2 (1 –2)
0 (0 –1)
1 (1 –2)
0 (0 –1)
0.59
0.86
Liver subscore
0 (0– 0)
0 (0 –0)
0 (0 –0)
0.62
16 (6– 20)
5 (3– 10)
16 (9 –20)
5 (4 –8)
12 (4 –22)
4 (2 –11)
0.36
0.39
...............................................................................................................................................................................
Timing of baseline measurements [median (IQR)]
Time from AMI (h)
Time from shock onset (h)
Table 2
Baseline haemodynamic parameters
All patients (n 5 68)
PCD ≤ mediana (n 5 35)
PCD > mediana (n 5 33)
P-value
...............................................................................................................................................................................
HR (b.p.m.)
MAP (mmHg)
93 (72– 104)
69 (61– 70)
92 (71– 106)
66 (58– 70)
93 (72– 104)
70 (64– 70)
0.80
0.07
CVP (mmHg)
15 (12– 18)
16 (12– 19)
14 (13– 16)
0.23
PCWP (mmHg)b
MPAP (mmHg)b
21 (16– 24)
28 (24– 34)
23 (18– 25)
30 (24– 37)
18 (14– 22)
27 (24– 30)
0.04
0.18
CI (L min21m22)
CPI (W m22)
SVR (dynes s cm25)
2.5 (2.1– 2.9)
2.4 (1.8– 2.9)
2.7 (2.1– 2.9)
0.44
0.35 (0.26– 0.42)
1075 (825–1242)
0.33 (0.24–0.39)
1075 (798–1237)
0.38 (0.30– 0.42)
1052 (850–1256)
0.11
0.79
SvO2 (%)
66 (61– 73)
65 (60– 70)
68 (62– 75)
0.12
Lactate (mmol L21)
2.8 (2.0– 4.3)
2.9 (1.8– 4.5)
2.8 (2.2– 4.8)
0.58
HR, heart rate; NS, non-significant; MAP, mean arterial pressure; CVP, central venous pressure; PCWP, pulmonary capillary wedge pressure; MPAP, mean pulmonary artery
pressure; CI, cardiac index; CPI, cardiac power index; SVR, systemic vascular resistance; SvO2, central-venous oxygen saturation.
a
Median PCD ¼ 10.3 mm mm22.
b
Data available in 48 (71%) of the patients.
Baseline sublingual perfused capillary
density
Baseline PCD correlated with MAP (r ¼ 0.34, P ¼ 0.004), PCWP
(r ¼ 20.32, P ¼ 0.03), and CPI (r ¼ 0.25, P ¼ 0.04) but not significantly with the baseline SOFA score or with other parameters
listed in Table 2. Baseline PCD predicted the change in the
SOFA score between T0 and T1 (DSOFA; r ¼ 20.25, P ¼ 0.04).
Patients with baseline sublingual PCD . median improved more
frequently in the total SOFA score (52 vs. 29%, P , 0.05) and in
the cardiac SOFA subscore (61 vs. 34%, P ¼ 0.03) at 24 h, when
compared with patients with sublingual impaired PCD ≤ median.
Twenty-two patients (32%) died during 30 days of follow-up. All
these patients died in the hospital. Of the patients who had a PCD ≤
median, 17 (49%) died vs. 5 (15%) of the patients with PCD .
median (P ¼ 0.004, Figure 2). Inverse sublingual PCD as a continuous
parameter had a greater predictive value on 30-day mortality than
the baseline SOFA score (area under the receiver operator characteristic curve of 0.75 vs. 0.56). The threshold best predicting 30-day
mortality was 10.0 mm mm22 [area under the curve of 0.72 vs. 0.69
when the median (10.3 mm mm22) was used]. Left ventricular ejection fraction ,30% (OR: 3.40, 95% CI: 1.07 –10.8) was significantly
associated with 30-day mortality, whereas CPI (OR: 0.42, 95% CI:
0.23 –0.78) and sublingual PCD (OR: 0.61, 95% CI: 0.44–0.84)
were significantly associated with improved 30-day survival. After
adjustment, CPI (OR: 0.48, 95% CI: 0.24–0.94) and sublingual
PCD (OR: 0.65, 95% CI: 0.45– 0.92) remained significant predictors
of 30-day outcome (Figure 3). Survival within 30 days according to
the quartile of baseline sublingual PCD is shown in Figure 4.
Downloaded from http://eurheartj.oxfordjournals.org/ by guest on September 6, 2014
SD, standard deviation; NS, non-significant; AMI, acute myocardial infarction; CV, cardiovascular; IABP, intra-aortic balloon pump; ECMO, extracorporeal membrane oxygenation;
NT-proBNP, N-terminal proB-type natriuretic peptide; IQR, interquartile range; WBC, white blood cell; CRP, C-reactive protein; GFR, glomerular filtration rate; MR, mitral valve
regurgitation; LM, left main coronary artery; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft surgery; SOFA, sequential organ failure assessment.
a
Median PCD ¼ 10.3 mm mm22.
b
Systolic blood pressure , 90 mmHg and clinical signs of hypoperfusion.
c
Dosages in mg kg21 min21.
�Page 6 of 8
Association between changes in PCD and
outcome
Figure 2 The Kaplan –Meier survival curve stratified according
to perfused capillary density at baseline. Median perfused capillary
density ¼ 10.3 mm mm22.
patients stratified to the level of PCD at both time points is shown
in Figure 5. Patients who had a PCD ≤ median at baseline, which
improved at T1 (‘low-high’), had a significant better prognosis when
compared with patients who had a persistently low PCD (‘low-low’).
When patients in whom no second measurement was performed
were regarded as the sicker patients (i.e. PCD T1 ≤ median), results
were identical. Finally, an increase in PCD was significantly associated
with a better outcome (OR: 0.73, 95% CI: 0.54–0.99).
Discussion
In this study, we demonstrated that patients with cardiogenic shock
from acute myocardial infarction who had a sublingual PCD ≤
median had a higher risk to die. Baseline PCD was a significant predictor for change in the SOFA score within the next 24 h. In addition,
the sublingual PCD at 24 h correlated with the SOFA score at T1.
Patients with a higher baseline sublingual PCD were more likely to
improve in the total SOFA score as well as in the cardiac SOFA subscore at 24 h. Furthermore, the baseline PCD was strongly and independently associated with 30-day outcome. Finally, in a large
subgroup of patients in whom measurements were repeated, we
demonstrated that patients who had a sublingual PCD ≤ median
at baseline as well as after 24 h were at high risk of poor outcome,
as opposed to those patients in whom microcirculation recovered
within 24 h. In the latter patients, survival rates were similar to
those of patients with PCD . median at both time points.
Using a semi-quantitative analysis technique, De Backer et al. 36
previously described sublingual microcirculatory alterations in 31
patients with cardiogenic shock. The authors reported a weak correlation of the proportion of perfused capillaries with MAP, which
is in line with our findings. We also found a weak correlation
between sublingual PCD and CPI. Such relative dissociation
between macrocirculation (haemodynamic measurements) and
microcirculation (perfusion) has been demonstrated previously.37
Since PCD was strongly associated with 30-day outcome, monitoring of microcirculation may therefore have an additional value for
risk stratification as well as for the treatment of patients with cardiogenic shock.38
Figure 3 Predictors of 30-day mortality (univariate and multivariate analyses). The multivariate logistic regression model selection was done
with the backward stepwise method starting with the following variables: age . 75 years, CPI, baseline sequential organ failure assessment
score, nitroglycerine, left main coronary artery occlusion, left ventricular ejection fraction , 30%, significant mitral valve regurgitation, and sublingual perfused capillary density. Variables that remained significantly associated with 30-day mortality were part of the regression equation and
are presented. The multivariate model was confirmed by using the forward stepwise selection.
Downloaded from http://eurheartj.oxfordjournals.org/ by guest on September 6, 2014
In 54 patients (79%), PCD measurements were repeated (T1). In the
remaining patients (n ¼ 14), PCD measurements at T1 were not possible. One patient died immediately after the first measurements, five
patients were sent back to the referring hospital before T1, and in
eight patients, there was no investigator available to perform the
measurements. Overall, sublingual PCD tended to increase at T1 relative to T0 (10.3 + 2.2 mm mm22 at T0 vs. 10.9 + 2.2 mm mm22 at
T1, P ¼ 0.09). At time point T0, 27% of patients had a PCD ≥
11.7 mm mm22 (reference value in control patients) and at T1, 43%
of patients reached reference values (T0 vs. T1, P , 0.05). Changes
in sublingual PCD were inversely correlated with changes in CVP
(r ¼ 20.38, P ¼ 0.009). There was a modest correlation between
PCD measured at 24 h and SOFA scores at T1 (r ¼ 20.40, P ¼
0.003). In the total study group, no significant correlation between
changes in PCD and changes in SOFA score was found. However,
patients who had a PCD ≤ median at both time points had higher
SOFA scores at T1 relative to patients who had a sublingual PCD .
median at T0 and T1 [7 (4–8) vs. 4 (3–5), P ¼ 0.03]. Survival of
C.A. den Uil et al.
�Page 7 of 8
Impaired microcirculation predicts poor
Clinical perspectives
Figure 4 The Kaplan–Meier survival curve stratified according
to the quartile of baseline sublingual perfused capillary density.
These findings raise the question whether sublingual PCD can be
used as a therapeutic target at the bedside and, if so, whether
interventions directed at improving PCD will be associated with
improved outcome. We demonstrated recently that PCD can be
improved by pharmacologic therapy (nitroglycerine)25,26 as well
as by mechanical circulatory support.29 The current study demonstrates that patients who had a low PCD at baseline which recovered at 24 h had a similar prognosis as those who had a higher
PCD at both time points. Taken together, these results suggest
that assessment of sublingual PCD by SDF imaging, followed by
prompt interventions directed at improving microvascular perfusion, might optimize therapy in order to improve the outcome
of patients with cardiogenic shock.
Limitations
Trzeciak et al.39 recently demonstrated that increased sublingual
microcirculatory flow during resuscitation of septic shock was associated with lower SOFA scores at 24 h. In contrast, we did not find a
relationship between changes in the sublingual PCD and changes in
the SOFA score between T0 and T1. Nevertheless, we demonstrated
that the sublingual PCD at baseline was predictive for recovery from
organ failure. In addition, patients who had a PCD ≤ median at T0 as
well as at T1 had the highest SOFA scores at T1.
Hasdai et al.40 demonstrated the predictive value of a cold,
clammy skin on 30-day mortality in patients with cardiogenic
shock complicating acute myocardial infarction. In addition, De
Backer et al. 36 reported that the proportion of sublingual perfused
capillaries, measured after hospital admission, was higher in patients
who survived than in patients who did not survive (64 vs. 43%, P ,
0.05). In our (larger) study, we confirmed these observations and
demonstrated that in patients all having clinical signs of hypoperfusion, sublingual PCD can be used to better define the severity of cardiogenic shock and to refine the prediction of outcome.
Conclusions
In conclusion, impaired microcirculation, as assessed by sublingual
PCD, is associated with the development of (multi-)organ failure.
In addition, this parameter is an independent, strong predictor of
outcome. Because of the independent and strong association
with prognosis in cardiogenic shock, assessment of sublingual
PCD using SDF imaging should be considered as a simple noninvasive tool to assess outcome in patients with cardiogenic
shock. Whether a strategy of improving sublingual PCD will
improve the survival of patients with cardiogenic shock, should
preferably be tested in a future, multicentre randomized trial.
Supplementary material
Supplementary material is available at European Heart Journal online.
Conflict of interest: none declared.
Downloaded from http://eurheartj.oxfordjournals.org/ by guest on September 6, 2014
Figure 5 The Kaplan –Meier survival curve of short-term
survival of cardiogenic shock patients stratified according to the
sublingual perfused capillary density at baseline and after 24 h.
Low–high, perfused capillary density ≤ median at T0 and perfused capillary density . median at T1; High –high, perfused capillary density . median at T0 and perfused capillary
density . median at T1; High–low, perfused capillary density .
median at T0 and perfused capillary density ≤ median at T1;
Low–low, perfused capillary density ≤ median at T0 and perfused capillary density ≤ median at T1.
Several limitations of our study need to be acknowledged. First,
measurements of the pulmonary circulation by a PAC were
missing in some patients when the attending clinicians were unwilling to use this monitoring device, even in a research setting.
Second, PCD measurements could not be repeated in some
patients. Third, we measured patients only after informed
consent had been obtained. This implies that, in most cases, it consumed hours before baseline measurements could be performed.
Nevertheless, our study clearly demonstrates that in these
patients, already being resuscitated, sublingual PCD can be used
to identify patients who are at a high risk of dying. Fourth, we
used PCD as the marker of microcirculatory perfusion, a softwarederived parameter in which microvascular flow and density are
combined. This parameter does not take into account the heterogeneity of perfusion, which may be increased in disease states.41
However, the problem of heterogeneous blood flow, visualized
sublingually as fields of absent or intermittent capillary blood
flow, seems to be more specific for septic shock than for cardiogenic shock.16,36,42,43 Finally, since our study was an observational
study, significant correlations, e.g. between baseline PCD and
changes in SOFA score, do not prove causality.
�Page 8 of 8
References
23. Hubble SM, Kyte HL, Gooding K, Shore AC. Variability in sublingual microvessel
density and flow measurements in healthy volunteers. Microcirculation 2009;16:
183 –191.
24. Dobbe JG, Streekstra GJ, Atasever B, van Zijderveld R, Ince C. Measurement of
functional microcirculatory geometry and velocity distributions using automated
image analysis. Med Biol Eng Comput 2008;46:659 –670.
25. den Uil CA, Caliskan K, Lagrand WK, van der Ent M, Jewbali LS, van Kuijk JP,
Spronk PE, Simoons ML. Dose-dependent benefit of nitroglycerin on microcirculation of patients with severe heart failure. Intensive Care Med 2009;35:
1893 –1899.
26. den Uil CA, Lagrand WK, Spronk PE, van der Ent M, Jewbali LS, Brugts JJ, Ince C,
Simoons ML. Low-dose nitroglycerin improves microcirculation in hospitalized
patients with acute heart failure. Eur J Heart Fail 2009;11:386 –390.
27. den Uil CA, Lagrand WK, Spronk PE, van Domburg RT, Hofland J, Lüthen C,
Brugts JJ, van der Ent M, Simoons ML. Impaired sublingual microvascular perfusion
during surgery with cardiopulmonary bypass: a pilot study. J Thorac Cardiovasc Surg
2008;136:129 –134.
28. Boerma EC, Koopmans M, Konijn A, Kaiferova K, Bakker AJ, van Roon EN,
Buter H, Bruins N, Egbers PH, Gerritsen RT, Koetsier PM, Kingma WP,
Kuiper MA, Ince C. Effects of nitroglycerin on sublingual microcirculatory blood
flow in patients with severe sepsis/septic shock after a strict resuscitation protocol: a double-blind randomized placebo controlled trial. Crit Care Med 2009;38:
93 –100.
29. den Uil CA, Maat AP, Lagrand WK, van der Ent M, Jewbali LS, van Thiel RJ,
Spronk PE, Simoons ML. Mechanical circulatory support devices improve tissue
perfusion in patients with end-stage heart failure or cardiogenic shock. J Heart
Lung Transpl 2009;28:906 –911.
30. Arnold RC, Parrillo JE, Phillip Dellinger R, Chansky ME, Shapiro NI, Lundy DJ,
Trzeciak S, Hollenberg SM. Point-of-care assessment of microvascular blood
flow in critically ill patients. Intensive Care Med 2009;35:1761 –1766.
31. Vincent JL, Angus DC, Artigas A, Kalil A, Basson BR, Jamal HH, Johnson G,
Bernard GR. Effects of drotrecogin alfa (activated) on organ dysfunction in the
PROWESS trial. Crit Care Med 2003;31:834 –840.
32. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H,
Reinhart CK, Suter PM, Thijs LG. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working
Group on Sepsis-Related Problems of the European Society of Intensive Care
Medicine. Intensive Care Med 1996;22:707 –710.
33. Fincke R, Hochman JS, Lowe AM, Menon V, Slater JN, Webb JG, LeJemtel TH,
Cotter G. Cardiac power is the strongest hemodynamic correlate of mortality
in cardiogenic shock: a report from the SHOCK trial registry. J Am Coll Cardiol
2004;44:340 –348.
34. Garcia-Alvarez A, Arzamendi D, Loma-Osorio P, Kiamco R, Masotti M, Sionis A,
Betriu A, Brugada J, Bosch X. Early risk stratification of patients with cardiogenic
shock complicating acute myocardial infarction who undergo percutaneous coronary intervention. Am J Cardiol 2009;103:1073 – 1077.
35. Picard MH, Davidoff R, Sleeper LA, Mendes LA, Thompson CR, Dzavik V,
Steingart R, Gin K, White HD, Hochman JS. Echocardiographic predictors of survival and response to early revascularization in cardiogenic shock. Circulation 2003;
107:279 – 284.
36. De Backer D, Creteur J, Dubois MJ, Sakr Y, Vincent JL. Microvascular alterations
in patients with acute severe heart failure and cardiogenic shock. Am Heart J 2004;
147:91 –99.
37. De Backer D, Ortiz JA, Salgado D. Coupling microcirculation to systemic hemodynamics. Curr Opin Crit Care 2010;16:250–254.
38. Kaluski E, Milo-Cotter O, Cotter G. Death and life are in the power of the tongue.
Cardiology 2009;114:39–41.
39. Trzeciak S, McCoy JV, Delllinger RP, Arnold RC, Rizzuto M, Abate NL,
Shapiro NL, Parillo JE, Hollenberg SM. Early increases in microcirculatory perfusion during protocol-directed resuscitation are associated with reduced multiorgan failure at 24 h in patients with sepsis. Intensive Care Med 2008;34:
2210 –2217.
40. Hasdai D, Holmes DR, Califf RM, Thompson TD, Hochman JS, Pfisterer M, Topol EJ.
Cardiogenic shock complicating acute myocardial infarction: predictors of death.
GUSTO Investigators. Global Utilization of Streptokinase and Tissue-Plasminogen
Activator for Occluded Coronary Arteries. Am Heart J 1999;138:21–31.
41. Spanos A, Jhanji S, Vivian-Smith A, Harris T, Pearse RM. Early microvascular
changes in sepsis and severe sepsis. Shock 2010;33:387–391.
42. Klijn E, Den Uil CA, Bakker J, Ince C. The heterogeneity of the microcirculation in
critical illness. Clin Chest Med 2008;29:643–654.
43. Wan Z, Ristagno G, Sun S, Li Y, Weil MH, Tang W. Preserved cerebral microcirculation during cardiogenic shock. Crit Care Med 2009;37:2333 –2337.
Downloaded from http://eurheartj.oxfordjournals.org/ by guest on September 6, 2014
1. Wu AH, Parsons L, Every NR, Bates ER. Hospital outcomes in patients presenting
with congestive heart failure complicating acute myocardial infarction: a report
from the Second National Registry of Myocardial Infarction (NRMI-2). J Am Coll
Cardiol 2002;40:1389 –1394.
2. Goldberg RJ, Spencer FA, Gore JM, Lessard D, Yarzebski J. Thirty-year trends
(1975 to 2005) in the magnitude of, management of, and hospital death rates
associated with cardiogenic shock in patients with acute myocardial infarction:
a population-based perspective. Circulation 2009;119:1211 –1219.
3. Cheng JM, Valk SDA, den Uil CA, van der Ent M, Lagrand WK, van de Sande M,
van Domburg RT, Simoons ML. Usefulness of intra-aortic balloon pump counterpulsation in patients with cardiogenic shock from acute myocardial infarction. Am
J Cardiol 2009;104:327 – 332.
4. Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P,
Poole-Wilson PA, Strömberg A, van Veldhuisen DJ, Atar D, Hoes AW,
Keren A, Mebazaa A, Nieminen M, Priori SG, Swedberg K. ESC guidelines for
the diagnosis and treatment of acute and chronic heart failure 2008: the Task
Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure
2008 of the European Society of Cardiology. Developed in collaboration with
the Heart Failure Association of the ESC (HFA) and endorsed by the European
Society of Intensive Care Medicine (ESICM). Eur Heart J 2008;29:2388 –2442.
5. Lim N, Dubois MJ, De Backer D, Vincent JL. Do all nonsurvivors of cardiogenic
shock die with a low cardiac index? Chest 2003;124:1885 –1891.
6. Cheng JM, Den Uil CA, Hoeks SE, Van der Ent M, Jewbali LS, Van Domburg RT,
Serruys PW. Percutaneous left ventricular assist devices vs. intra-aortic balloon
pump counterpulsation for treatment of cardiogenic shock: a meta-analysis of
controlled trials. Eur Heart J 2009;30:2102 –2108.
7. Kohsaka S, Menon V, Lowe AM, Lange M, Dzavik V, Sleeper LA, Hochman JS. Systemic inflammatory response syndrome after acute myocardial infarction complicated by cardiogenic shock. Arch Intern Med 2005;165:1643 –1650.
8. Reynolds HR, Hochman JS. Cardiogenic shock: current concepts and improving
outcomes. Circulation 2008;117:686 –697.
9. Hasper D, Hummel M, Kleber FX, Reindl I, Volk HD. Systemic inflammation in
patients with heart failure. Eur Heart J 1998;19:761 –765.
10. Reilly PM, Wilkins KB, Fuh KC, Haglund U, Bulkley GB. The mesenteric hemodynamic response to circulatory shock: an overview. Shock 2001;15:329 –343.
11. Smith I, Kumar P, Molloy S, Rhodes A, Newman PJ, Grounds RM, Bennett ED.
Base excess and lactate as prognostic indicators for patients admitted to intensive
care. Intensive Care Med 2001;27:74–83.
12. Geppert A, Dorninger A, Delle-Karth G, Zorn G, Heinz G, Huber K. Plasma concentrations of interleukin-6, organ failure, vasopressor support, and successful coronary revascularization in predicting 30-day mortality of patients with cardiogenic
shock complicating acute myocardial infarction. Crit Care Med 2006;34:2035 –2042.
13. Nicholls SJ, Wang Z, Koeth R, Levison B, DelFraino B, Dzavik V, Griffith OW,
Hathaway D, Panza JA, Nissen SE, Hochman JS, Hazen SL. Metabolic profiling
of arginine and nitric oxide pathways predicts hemodynamic abnormalities and
mortality in patients with cardiogenic shock after acute myocardial infarction. Circulation 2007;116:2315 –2324.
14. Jarai R, Fellner B, Haoula D, Jordanova N, Heinz G, Delle-Karth G, Huber K,
Geppert A. Early assessment of outcome in cardiogenic shock: Relevance of
plasma N-terminal pro-B-type natriuretic peptide and interleuking-6 levels. Crit
Care Med 2009;37:1837 –1844.
15. Hochman JS. Cardiogenic shock complicating acute myocardial infarction:
expanding the paradigm. Circulation 2003;107:2998 –3002.
16. den Uil CA, Klijn E, Lagrand WK, Brugts JJ, Ince C, Spronk PE, Simoons ML. The
microcirculation in health and critical disease. Prog Cardiovasc Dis 2008;51:
161 –170.
17. Ware LB, Matthay MA. Measuring microvascular blood flow in sepsis-a continuing
challenge. Lancet 2002;360:1187 –1188.
18. Struijker-Boudier HA, Rosei AE, Bruneval P, Camici PG, Christ F, Henrion D,
Lévy BI, Pries A, Vanoverschelde JL. Evaluation of the microcirculation in hypertension and cardiovascular disease. Eur Heart J 2007;28:2834 –2840.
19. Cuschieri J, Rivers EP, Donnino MW, Katilius M, Jacobsen G, Nguyen HB,
Pamukov N, Horst HM. Central venous-arterial carbon dioxide difference as an
indicator of cardiac index. Intensive Care Med 2005;31:818 – 822.
20. Goedhart PT, Khalilzada M, Bezemer R, Merza J, Ince C. Sidestream Dark Field
(SDF) imaging: a novel stroboscopic LED ring-based imaging modality for clinical
assessment of the microcirculation. Opt Express 2007;15:15101– 15114.
21. Spronk PE, Ince C, Gardien MJ, Mathura KR, Oudemans-van Straaten HM,
Zandstra DF. Nitroglycerin in septic shock after intravascular volume resuscitation. Lancet 2002;360:1395 –1396.
22. De Backer D, Hollenberg S, Boerma C, Goedhart P, Büchele G,
Ospina-Tascon G, Dobbe I, Ince C. How to evaluate the microcirculation:
report of a round table conference. Crit Care 2007;11:R101.
C.A. den Uil et al.
�