Streamline Your Medical Bill Book Format for Product Quality with airSlate SignNow
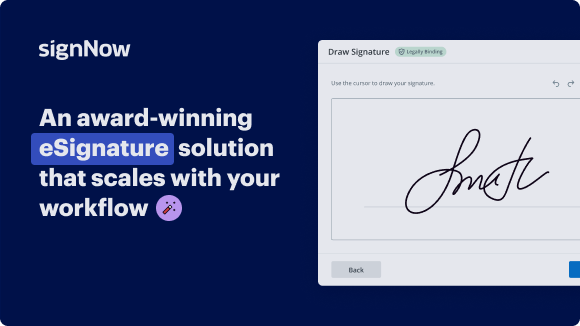
See airSlate SignNow eSignatures in action
Choose a better solution
Move your business forward with the airSlate SignNow eSignature solution
Add your legally binding signature
Integrate via API
Send conditional documents
Share documents via an invite link
Save time with reusable templates
Improve team collaboration
Our user reviews speak for themselves






airSlate SignNow solutions for better efficiency
Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.

How to use medical bill book format for product quality
Ensuring high product quality is crucial for businesses, and using a structured approach can greatly improve the process. One such approach is leveraging digital tools like airSlate SignNow, which offers an efficient method for handling documents. This guide will walk you through the steps needed to get started with airSlate SignNow to enhance your document signing process while maintaining product quality.
Using medical bill book format for product quality with airSlate SignNow
- Visit the airSlate SignNow website on your preferred browser.
- Create a free trial account or log into your existing account.
- Select and upload a document that requires signing or that you wish to send for signatures.
- If you plan to use this document again, convert it into a reusable template.
- Access your uploaded file and make necessary edits, such as adding fillable fields and relevant information.
- Apply your signature to the document and designate areas for recipients to sign.
- Proceed by clicking 'Continue' to configure and dispatch the eSignature invitation.
airSlate SignNow is designed to enable businesses to send and eSign documents efficiently while providing signNow savings. Its rich feature set ensures a substantial return on investment, making it perfect for small to mid-sized businesses.
With straightforward pricing that eliminates hidden fees and superior support around the clock for paid plans, airSlate SignNow stands out as a reliable solution. Start streamlining your document workflow today!
How it works
Get legally-binding signatures now!
FAQs
-
What is the medical bill book format for product quality?
The medical bill book format for product quality is a structured template used to ensure accurate billing and documentation in healthcare. This format helps standardize entries for medical services, facilitating better tracking and accountability of product quality in medical billing processes. -
How does airSlate SignNow support the medical bill book format for product quality?
airSlate SignNow supports the medical bill book format for product quality by offering customizable templates that enhance accuracy and compliance. With our eSigning capabilities, businesses can easily manage and electronically sign medical bills, ensuring they align with the necessary quality standards. -
Are there any pricing options for using airSlate SignNow with the medical bill book format for product quality?
Yes, airSlate SignNow offers competitive pricing plans tailored to various business needs. These plans enable access to features that enhance the medical bill book format for product quality, allowing you to manage document workflows efficiently. -
What features does airSlate SignNow provide for the medical bill book format for product quality?
airSlate SignNow includes features such as customizable templates, secure electronic signatures, and real-time collaboration tools. These features streamline the management of your medical bill book format for product quality, making documentation processes simpler and more effective. -
Can I integrate airSlate SignNow with other systems while using the medical bill book format for product quality?
Absolutely! airSlate SignNow offers seamless integrations with various business applications. This capability allows you to enhance your workflow while utilizing the medical bill book format for product quality across different platforms for maximum efficiency. -
What are the benefits of using airSlate SignNow for the medical bill book format for product quality?
Using airSlate SignNow for the medical bill book format for product quality provides numerous benefits, including improved accuracy, reduced processing time, and enhanced compliance. These advantages help businesses maintain a high standard of quality in their medical billing practices. -
How can airSlate SignNow improve my team’s efficiency with the medical bill book format for product quality?
airSlate SignNow enhances your team's efficiency by automating repetitive tasks and providing easy access to the medical bill book format for product quality. The platform's user-friendly interface allows team members to create, edit, and sign documents swiftly, signNowly reducing turnaround times.
What active users are saying — medical bill book format for product quality
Get more for medical bill book format for product quality
- Car Service Receipt for Travel Industry
- Car service receipt for HighTech
- Car Service Receipt for Manufacturing
- Car service receipt for Building services
- Car Service Receipt for Sport Organisations
- Car service receipt for Pharmaceutical
- Get Your Car Service Receipt for Human Resources
- Car service receipt for HR
Find out other medical bill book format for product quality
- Empowering your workflows with AI for bank loan ...
- Empowering your workflows with AI for car lease ...
- Empowering your workflows with AI for child custody ...
- Empowering your workflows with AI for engineering ...
- Empowering your workflows with AI for equipment sales ...
- Empowering your workflows with AI for grant proposal ...
- Empowering your workflows with AI for lease termination ...
- Empowering your workflows with AI for postnuptial ...
- Empowering your workflows with AI for retainer ...
- Empowering your workflows with AI for sales invoice ...
- Empowering your workflows with AI tools for signing a ...
- Start Your eSignature Journey: sign pdf documents
- Start Your eSignature Journey: online pdf signer
- Start Your eSignature Journey: sign doc online
- Start Your eSignature Journey: sign documents online
- Start Your eSignature Journey: sign the pdf online
- Start Your eSignature Journey: signing on pdf online
- Start Your eSignature Journey: sign any document online
- Start Your eSignature Journey: signed documents
- Start Your eSignature Journey: sign pdf document free