Streamline Your Billing Process with a Medical Invoice Format for Operations
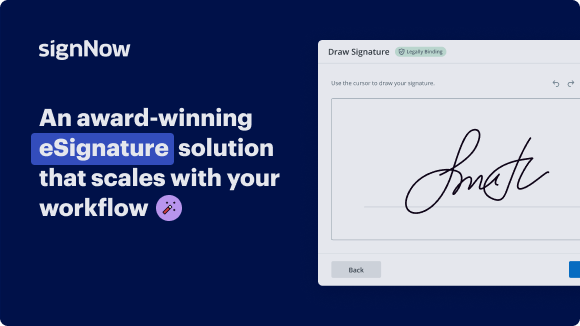
See airSlate SignNow eSignatures in action
Choose a better solution
Move your business forward with the airSlate SignNow eSignature solution
Add your legally binding signature
Integrate via API
Send conditional documents
Share documents via an invite link
Save time with reusable templates
Improve team collaboration
Our user reviews speak for themselves






airSlate SignNow solutions for better efficiency
Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.

How to create a medical invoice format for operations using airSlate SignNow
Creating a medical invoice format for operations can be streamlined with airSlate SignNow. This platform allows healthcare providers to efficiently send and sign documents, ensuring that the billing process is smooth and error-free. With its user-friendly interface and robust features, you can focus on what matters most—providing quality care.
Steps to create a medical invoice format for operations
- Open your web browser and navigate to the airSlate SignNow homepage.
- Register for a free trial or log in to your existing account.
- Select the document you wish to sign or send out for signatures and upload it.
- If relevant, convert your uploaded document into a reusable template.
- Access your uploaded document and modify it by inserting editable fields or required details.
- Affix your signature and designate fields for the other signers.
- Proceed by clicking the Continue button to configure and dispatch your eSignature invitation.
Utilizing airSlate SignNow can signNowly enhance your document signing experience. Its effective features promise excellent returns on investment with each dollar spent, while being easy to adapt for small to mid-sized businesses.
With clear and straightforward pricing, users won't face hidden costs or unexpected fees. Plus, airSlate SignNow provides reliable 24/7 customer support for all subscription plans. Start transforming your document processes today!
How it works
Get legally-binding signatures now!
FAQs
-
What is a medical invoice format for operations?
A medical invoice format for operations is a structured document used to itemize the services rendered during a medical procedure. It typically includes patient information, details of services provided, and payment terms. Understanding this format is crucial for both healthcare providers and patients to ensure accurate billing. -
How does airSlate SignNow support the medical invoice format for operations?
airSlate SignNow provides a user-friendly platform that allows medical professionals to create and manage invoices effortlessly. With customizable templates, users can easily design a medical invoice format for operations that meets their specific needs. This enhances accuracy and efficiency in the billing process. -
Can I integrate airSlate SignNow with existing billing software for medical invoices?
Yes, airSlate SignNow offers integrations with various billing software solutions. This capability allows users to seamlessly incorporate their medical invoice format for operations into existing systems. As a result, you can streamline your billing processes while ensuring compliance and accuracy. -
What are the benefits of using airSlate SignNow for medical invoicing?
Using airSlate SignNow for medical invoicing streamlines the billing process, saves time, and reduces errors. The platform’s ease of use allows healthcare providers to focus more on patient care rather than paperwork. Additionally, the medical invoice format for operations can be easily shared and eSigned, enhancing the overall efficiency. -
Is there a cost associated with using airSlate SignNow for medical invoices?
Yes, airSlate SignNow is a cost-effective solution with various pricing plans tailored for different business needs. Prospective users can choose a plan that aligns with their requirements for creating and managing a medical invoice format for operations. The investment often leads to signNow savings in time and resources. -
How can I customize my medical invoice format for operations with airSlate SignNow?
airSlate SignNow offers various customization options to create a medical invoice format for operations that fits your practice’s branding. Users can modify templates, add logos, and adjust layout elements to ensure clarity and professionalism in their invoices. This personalization helps in maintaining consistency in patient communication. -
What security features does airSlate SignNow provide for medical invoices?
airSlate SignNow prioritizes security, offering features such as end-to-end encryption and secure cloud storage for medical invoices. This ensures that your medical invoice format for operations remains protected from unauthorized access. Compliance with healthcare regulations also adds an extra layer of safety for sensitive information.
What active users are saying — medical invoice format for operations
Get more for medical invoice format for operations
- Sales Proposal Automation Software for Enterprises
- Sales Proposal Automation Software for Small Businesses
- Sales Proposal Automation Software for Teams
- Sales Proposal Automation Software for Organizations
- Sales Proposal Automation Software for NPOs
- Sales Proposal Automation Software for Non-Profit Organizations
- Software Development Project Proposal for Businesses
- Software Development Project Proposal for Corporations
Find out other medical invoice format for operations
- ESignature Legality for Insurance Industry in United ...
- ESignature Lawfulness for Accounting and Tax in ...
- Ensuring eSignature Lawfulness for Healthcare in the ...
- Enhance eSignature Legitimacy for Government in United ...
- Boost your Manufacturing Business with eSignature ...
- Unlocking eSignature Legitimateness for Higher ...
- Digital Signature Legality for Retail Trade in United ...
- Ensuring Digital Signature Legality for Hospitality in ...
- Digital Signature Lawfulness for Insurance Industry in ...
- Understanding the Lawfulness of Digital Signatures for ...
- Ensuring Digital Signature Lawfulness for Hospitality ...
- Digital Signature Legitimacy for Government in United ...
- Unlock the Power of Digital Signature Legitimateness ...
- Boosting Digital Signature Legitimateness for Insurance ...
- Unlocking Digital Signature Legitimateness for Real ...
- Digital signature licitness for Financial Services in ...
- Unlock the Power of Digital Signature Licitness for ...
- Electronic Signature Legality for Mortgage in United ...
- Electronic Signature Lawfulness for Accounting and Tax ...
- Ensuring Electronic Signature Lawfulness for Insurance ...