Collaborate on Pharmacy Bill Format for R&D with Ease Using airSlate SignNow
See how it works!Click here to sign a sample doc
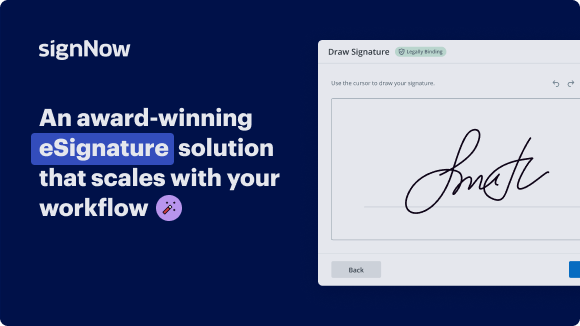
See airSlate SignNow eSignatures in action
be ready to get more
Choose a better solution
Move your business forward with the airSlate SignNow eSignature solution
Add your legally binding signature
Create your signature in seconds on any desktop computer or mobile device, even while offline. Type, draw, or upload an image of your signature.
Integrate via API
Deliver a seamless eSignature experience from any website, CRM, or custom app — anywhere and anytime.
Send conditional documents
Organize multiple documents in groups and automatically route them for recipients in a role-based order.
Share documents via an invite link
Collect signatures faster by sharing your documents with multiple recipients via a link — no need to add recipient email addresses.
Save time with reusable templates
Create unlimited templates of your most-used documents. Make your templates easy to complete by adding customizable fillable fields.
Improve team collaboration
Create teams within airSlate SignNow to securely collaborate on documents and templates. Send the approved version to every signer.
Our user reviews speak for themselves






Collect signatures
24x
faster
Reduce costs by
$30
per document
Save up to
40h
per employee / month
airSlate SignNow solutions for better efficiency
Keep contracts protected
Enhance your document security and keep contracts safe from unauthorized access with dual-factor authentication options. Ask your recipients to prove their identity before opening a contract to pharmacy bill format for rd.
Stay mobile while eSigning
Install the airSlate SignNow app on your iOS or Android device and close deals from anywhere, 24/7. Work with forms and contracts even offline and pharmacy bill format for rd later when your internet connection is restored.
Integrate eSignatures into your business apps
Incorporate airSlate SignNow into your business applications to quickly pharmacy bill format for rd without switching between windows and tabs. Benefit from airSlate SignNow integrations to save time and effort while eSigning forms in just a few clicks.
Generate fillable forms with smart fields
Update any document with fillable fields, make them required or optional, or add conditions for them to appear. Make sure signers complete your form correctly by assigning roles to fields.
Close deals and get paid promptly
Collect documents from clients and partners in minutes instead of weeks. Ask your signers to pharmacy bill format for rd and include a charge request field to your sample to automatically collect payments during the contract signing.
be ready to get more
Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.

Discover how to simplify your workflow on the pharmacy bill format for R&D with airSlate SignNow.
Searching for a way to simplify your invoicing process? Look no further, and adhere to these quick guidelines to conveniently collaborate on the pharmacy bill format for R&D or ask for signatures on it with our user-friendly platform:
- Set up an account starting a free trial and log in with your email sign-in information.
- Upload a file up to 10MB you need to eSign from your laptop or the online storage.
- Proceed by opening your uploaded invoice in the editor.
- Perform all the required actions with the file using the tools from the toolbar.
- Click on Save and Close to keep all the changes made.
- Send or share your file for signing with all the necessary recipients.
Looks like the pharmacy bill format for R&D workflow has just turned simpler! With airSlate SignNow’s user-friendly platform, you can easily upload and send invoices for eSignatures. No more producing a hard copy, signing by hand, and scanning. Start our platform’s free trial and it optimizes the whole process for you.
How it works
Open & edit your documents online
Create legally-binding eSignatures
Store and share documents securely
be ready to get more
Get legally-binding signatures now!
FAQs
-
What is a pharmacy bill format for rd?
A pharmacy bill format for rd is a structured document used for billing in the pharmacy industry, specifically for registered distributors. This format ensures compliance with regulations and facilitates seamless transactions between pharmacies and suppliers. -
How can airSlate SignNow help with pharmacy bill format for rd?
airSlate SignNow streamlines the creation and signing process for pharmacy bill format for rd. With our user-friendly platform, you can easily generate, edit, and securely eSign your pharmacy bills, enhancing efficiency and compliance. -
What features does airSlate SignNow offer for managing pharmacy bills?
airSlate SignNow includes features such as customizable templates for pharmacy bill formats for rd, secure cloud storage, and integration with other systems. These features help streamline your billing process while ensuring the integrity of your documents. -
Is airSlate SignNow cost-effective for small pharmacies looking for pharmacy bill format for rd?
Yes, airSlate SignNow offers flexible pricing plans suitable for small pharmacies. By using our solution for pharmacy bill format for rd, businesses can save on administrative costs and reduce paperwork, making it an economical choice. -
Can I integrate airSlate SignNow with other software for pharmacy bill format for rd?
Absolutely! airSlate SignNow easily integrates with various software applications commonly used in pharmacies. This integration capability ensures that you can manage your pharmacy bill format for rd alongside your other business processes efficiently. -
What are the benefits of using airSlate SignNow for pharmacy bills?
Using airSlate SignNow for pharmacy bills streamlines your workflow, enhances security, and improves document accessibility. By adopting a digital pharmacy bill format for rd, your team can focus more on patient care rather than paperwork. -
Is there customer support for creating pharmacy bill format for rd in airSlate SignNow?
Yes, airSlate SignNow provides excellent customer support to help you with pharmacy bill format for rd. Our dedicated support team is available to assist you with any questions or challenges you may encounter during setup and use.
What active users are saying — pharmacy bill format for rd
Get more for pharmacy bill format for rd
- Top Contract Management Vendors for Sport Organisations
- Top Contract Management Vendors for Pharmaceutical
- Top Contract Management Vendors for Human Resources
- Top Contract Management Vendors for HR
- Top Contract Management Vendors for Entertainment
- Top Contract Management Vendors for Education
- Contract Analytics Software for Accounting and Tax
- Contract Analytics Software for Communications Media
Find out other pharmacy bill format for rd
- ESignature Legality for Non-Compete Agreement in UAE
- Ensure eSignature Legality for Advertising Agreement in ...
- ESignature Lawfulness for Cease and Desist Letter in ...
- Unlock the Power of eSignature Legitimateness for ...
- ESignature Legitimateness for Business Associate ...
- ESignature Legitimateness for Non-Compete Agreement in ...
- Enhance eSignature Legitimateness for Polygraph Consent ...
- Unlock the power of eSignature licitness for Stock ...
- Unlocking the Power of Digital Signature Legality for ...
- Ensuring Compliance with Australian Digital Signature ...
- Digital Signature Legitimacy for Sick Leave Policy in ...
- Enhance Digital Signature Legitimateness for Commercial ...
- Digital Signature Legitimateness for Addressing ...
- Ensuring digital signature licitness for Toll ...
- Understanding Electronic Signature Legality for ...
- Ensuring Electronic Signature Lawfulness for Contract ...
- Understanding the Lawfulness of Electronic Signatures ...
- Unlocking the Power of Electronic Signature Legitimacy ...
- Enhance Freelance Contract Legitimacy with Electronic ...
- Electronic Signature Legitimateness for Contracts in ...