Streamline Your Sickness Billing Format for R&D with airSlate SignNow
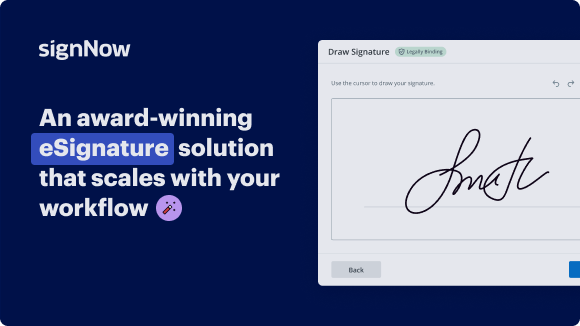
See airSlate SignNow eSignatures in action
Choose a better solution
Move your business forward with the airSlate SignNow eSignature solution
Add your legally binding signature
Integrate via API
Send conditional documents
Share documents via an invite link
Save time with reusable templates
Improve team collaboration
Our user reviews speak for themselves






airSlate SignNow solutions for better efficiency
Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.

Using sickness billing format for R&D with airSlate SignNow
The sickness billing format for R&D can be efficiently managed using airSlate SignNow. This popular eSignature tool streamlines the document signing process, allowing businesses to focus on their core activities while ensuring compliance and speed. With airSlate SignNow, users can create, edit, and send important documents for electronic signing quickly and effortlessly.
Steps to utilize sickness billing format for R&D with airSlate SignNow
- Visit the airSlate SignNow website on your preferred browser.
- Create a free account or log into your existing one.
- Select and upload the document meant to be signed or sent for signatures.
- If you plan to use the document repeatedly, convert it into a reusable template.
- Access your document and make necessary modifications: insert fillable fields or other required information.
- Sign your document and designate areas where recipients can add their signatures.
- Click on 'Continue' to configure settings and dispatch your eSignature invitation.
airSlate SignNow delivers exceptional value for businesses by providing an intuitive platform that’s cost-effective and suitable for small to mid-sized organizations. Its transparent pricing structure ensures you won't encounter unexpected fees, while its impressive feature set maximizes your return on investment.
With dedicated support available around the clock for all paid plans, airSlate SignNow becomes an indispensable asset for any business. Start streamlining your document processes today!
How it works
Get legally-binding signatures now!
FAQs
-
What is the sickness billing format for rd?
The sickness billing format for rd is a structured template designed for accurately documenting and billing sick leave for registered doctors. This format ensures that all necessary information is included, streamlining the billing process and ensuring compliance with industry standards. -
How can airSlate SignNow help with the sickness billing format for rd?
airSlate SignNow simplifies the process of generating and sending the sickness billing format for rd. Our platform allows users to create, edit, and send custom documents quickly, making it easier to manage sick leave billing efficiently. -
Is there a free trial available for using airSlate SignNow?
Yes, airSlate SignNow offers a free trial that allows potential users to explore the features, including those specific to the sickness billing format for rd. This trial will enable you to experience firsthand how our solution can improve your document management. -
What features does airSlate SignNow offer for billing documentation?
Our platform includes electronic signatures, customizable templates, and document tracking features that are ideal for creating the sickness billing format for rd. These tools help ensure that your documentation is accurate, professional, and legally binding. -
Are there specific integrations available for the sickness billing format for rd?
Yes, airSlate SignNow integrates seamlessly with various healthcare management systems to enhance the use of the sickness billing format for rd. This compatibility ensures that you can manage all aspects of billing within a unified system. -
How does airSlate SignNow ensure data security for sensitive billing information?
airSlate SignNow prioritizes data security by employing top-tier encryption and compliance measures when handling sensitive information like the sickness billing format for rd. This ensures that your data remains confidential and secure during the entire billing process. -
What are the pricing options for airSlate SignNow?
airSlate SignNow offers flexible pricing plans designed to accommodate various business needs, including options for utilizing the sickness billing format for rd. Our pricing is transparent, allowing users to select a plan that best suits their organization's requirements.
What active users are saying — sickness billing format for rd
Get more for sickness billing format for rd
- Federal Contract Management for Production
- Streamline Federal Contract Management for Supervision
- Federal Contract Management for Product Quality
- Federal Contract Management for Inventory
- Federal Contract Management for Security
- Federal Contract Management for RD
- Federal Contract Management for Personnel
- Free Contract Management for Facilities
Find out other sickness billing format for rd
- Unlock the Power of eSignature: free eSignature app
- Unlock the Power of eSignature: free eSignature ...
- Find All You Need to Know: free fill and sign PDF ...
- Start Your eSignature Journey: free HIPAA compliant ...
- Explore Your Digital Signature – Questions Answered: ...
- Unlock the Power of eSignature: free online electronic ...
- Unlock the Power of eSignature: free online electronic ...
- Unlock the Power of eSignature: free online form ...
- Unlock the Power of eSignature: free online handwritten ...
- Unlock the Power of eSignature: free online HTML ...
- Find All You Need to Know: free online PDF editor ...
- Find All You Need to Know: free online PDF fill and ...
- Find All You Need to Know: free online PDF sign and ...
- Start Your eSignature Journey: free online signature
- Start Your eSignature Journey: free online signature ...
- Start Your eSignature Journey: free online signature ...
- Enjoy Flexible eSignature Workflows: free online ...
- Start Your eSignature Journey: free online signature ...
- Unlock the Power of eSignature: free online signature ...
- Unlock the Power of eSignature: free online signature ...