Downloaded from genesdev.cshlp.org on September 6, 2014 - Published by Cold Spring Harbor Laboratory Press
Migratory neighbors and distant invaders: tumor-associated niche
cells
Jared Wels, Rosandra N. Kaplan, Shahin Rafii, et al.
Genes Dev. 2008 22: 559-574
Access the most recent version at doi:10.1101/gad.1636908
References
Email Alerting
Service
Topic
Collections
This article cites 150 articles, 60 of which can be accessed free at:
http://genesdev.cshlp.org/content/22/5/559.full.html#ref-list-1
Receive free email alerts when new articles cite this article - sign up in the box at the top
right corner of the article or click here.
Articles on similar topics can be found in the following collections
Cancer and Disease Models (139 articles)
To subscribe to Genes & Development go to:
http://genesdev.cshlp.org/subscriptions
Copyright © 2008, Cold Spring Harbor Laboratory Press
�Downloaded from genesdev.cshlp.org on September 6, 2014 - Published by Cold Spring Harbor Laboratory Press
REVIEW
Migratory neighbors and distant invaders:
tumor-associated niche cells
Jared Wels,1,2,4 Rosandra N. Kaplan,1,2,4 Shahin Rafii,2,3,6 and David Lyden1,2,5
1
Department of Pediatrics and Department of Cell and Developmental Biology, Weill Cornell Medical College,
New York, New York 10021, USA; 2Memorial Sloan-Kettering Cancer Center, New York, New York 10021, USA;
3
Department of Genetic Medicine, Weill Cornell Medical College, New York, New York 10021, USA
The cancer environment is comprised of tumor cells as
well as a wide network of stromal and vascular cells
participating in the cellular and molecular events necessary for invasion and metastasis. Tumor secretory factors can activate the migration of host cells, both near to
and far from the primary tumor site, as well as promote
the exodus of cells to distant tissues. Thus, the migration of stromal cells and tumor cells among specialized
microenvironments takes place throughout tumor and
metastatic progression, providing evidence for the systemic nature of a malignancy. Investigations of the tumor–stromal and stromal–stromal cross-talk involved in
cellular migration in cancer may lead to the design of
novel therapeutic strategies.
missive niches that, in return, promote tumor cell survival and proliferation. The focus of this review is on the
cellular constituents of the primary and metastatic tumor microenvironments, with emphasis on their migratory pathways. We hope to convey that the tumor and
host cell interaction is truly reciprocal; while host cells
may support tumor cells, tumor cells in turn modulate
the microenvironments within which they reside. Furthermore, we highlight that cancer is a systemic disease,
encompassing collective cell movements of tumor and
stromal cells that are a prerequisite for tumor cell invasion and metastasis.
Intrinsic tumor cell migratory capabilities
Understanding the complex biological networks at play
in metastasis requires a precise detailing of the molecular and cellular pathways involved in local and systemic
migration. The long prevailing model of invasion and
metastasis has focused on the adhesive and migratory
capabilities that are intrinsic to tumor cells (Hanahan
and Weinberg 2000). Meanwhile, we are becoming increasingly aware that tumors are composed of genetically altered malignant cells along with a heterogeneous
population of stromal cells, whose dynamic interactions
can profoundly enhance tumor progression and metastasis. Through the production of chemokines, growth factors, and matrix-degrading enzymes (Table 1), supportive
cells—including fibroblasts, immune cells, and bone
marrow (BM)-derived stem and progenitor cells—support
blood vessel formation, break down basement membrane barriers, and attract tumor cells to distant sites.
Tumor cells are constantly giving instructions, not only
by direct cell–cell interactions, but also by secreted factors that “activate” normal host cells at both proximal
and distal sites to migrate, eventually developing per-
[Keywords: Endothelial cells; invasion; metastasis; migration; stem cell;
tumor microenvironment]
4
These authors contributed equally to this work.
Corresponding authors.
5
E-MAIL dcl2001@med.cornell.edu; FAX (212) 746-8423.
6
E-MAIL srafii@med.cornell.edu; FAX (212) 746-8423.
Article is online at http://www.genesdev.org/cgi/doi/10.1101/gad.1636908.
Inherent to the metastatic process is the capability of
tumor cells to migrate through connective tissue barriers
comprising cell–cell adherent junctions, basement membranes, and interstitial tissue stroma. This intrinsic migratory behavior is highly dependent on the interplay
between adhesive and proteolytic activities. Tumor cell
down-regulation of proteins mediating cell–cell interactions, such as cadherins, leads to changes in cell signaling, actin-based cytoskeletal structure, and eventual dissociation from neighboring cells of the primary tumor
(Friedl and Brocker 2000). E-cadherin-based cell–cell contacts are replaced with cell–matrix interactions promoting locomotion resembling either a slow, adhesive fibroblast-like migration or a more dynamic ameboid crawling. Fibroblast-like migration is accompanied by integrin
cluster-mediated adherence to matrix fibrils and remodeling of the extracellular matrix (ECM). Alternately,
rapid ameboid migration, associated with certain carcinoma cells as well as lymphomas and leukemias, is dependent on ROCK family kinases that promote changes
in cell shape to navigate through the dense matrix environment (Friedl and Brocker 2000; Pinner and Sahai
2008). The deposition of proteases such as plasmin and a
variety of members of the matrix metalloprotease (MMP)
family is essential in tissue remodeling, which favors
tumor cell intravasation and dissemination.
Although the importance of the intrinsic migratory
ability of tumor cells for promoting metastasis is well
GENES & DEVELOPMENT 22:559–574 © 2008 by Cold Spring Harbor Laboratory Press ISSN 0890-9369/08; www.genesdev.org
559
�Downloaded from genesdev.cshlp.org on September 6, 2014 - Published by Cold Spring Harbor Laboratory Press
Wels et al.
Table 1. Significant trafficking molecules found within BM
and peripheral niches
Migratory neighbors support primary tumor growth
Growth factors
Predominant residents: fibroblasts help make
the move
Vascular endothelial growth factor-A
(VEGF-A)
Placental growth factor (PlGF)
Granulocyte colony-stimulating factor-
(G-CSF)
Platelet-derived growth factor (PDGF)
Colony-stimulating factor 1 (CSF-1)
Migration inhibitory factor (MIF)
Fibroblast growth factor (FGF)
Hepatocyte growth factor (HGF)
Epidermal growth factor (EGF)
Angiopoietin-1,-2
Brain-derived neurotrophic factor (BDNF)
Osteopontin
Insulin growth factor (IGF-1)
Receptors
VEGFR-1,
VEGFR-2
VEGFR-1
G-CSFR
PDGFR␣, 
M-CSFR
CD74
FGFR1–4
c-Met
EGFR
Tie-2
LNGFR, TrkB
CD44, VLA-4, ␣V3
IGF-I/IIR
Chemokines
Stromal-derived factor (SDF-1/CXCL12)
Transforming growth factor  (TGF-)
CC chemokine ligand 2 (CCL2/MCP-1)
CCL5
CXCL8/IL-8
CXCL1/MIP-2
CCL22
CCL12
IL-10
S100A8/9
S100A4
CXCR4, CXCR7
TGF-R I/II
CCR2
CCR1, 3, 4, 5
CXCR1, 2
CXCR1, 2
CCR4
CXCR4, CXCL12,
CCR2
IL-10R1, 2
CD36, LTB4
S100A4R, HSPG,
annexin II
Proteases
MMP-1,2,3,9,11,14
uPA
recognized, the contribution of the tumor microenvironment including its various cellular constituents also
provides essential signals that regulate tumor cell invasion and migration. In addition, we are just beginning to
appreciate the similarities in migratory characteristics
between tumor and stromal components of cancer.
These cellular transit pathways are essential for an exchange of information, providing necessary signals to
prepare and promote tumor progression. This allows for
global communication between local and distant microenvironments and involves cellular adaptation to
promote survival and growth at far-away sites. Components of this environment include local stromal cells,
such as resident fibroblasts and macrophages, and distant recruited cells such as endothelial cells, immune
cells, and BM-derived precursor cells, as well as circulating platelets that can communicate between BM, tumor, and distant tissue sites. Here we discuss the cellular constituents of the tumor microenvironment, actively migrating from sites both local and distant that
contribute to enhanced tumor cell motility, invasiveness, and survival (Fig. 1).
560
GENES & DEVELOPMENT
Fibroblasts constitute the majority of stromal cells
within the primary tumor bed in various types of human
carcinomas (Sappino et al. 1988). Until recently, the role
of these cells in tumor progression was unknown. As
with fibroblasts associated with wound healing, carcinoma-associated fibroblasts (CAFs) are referred to as “activated fibroblasts,” or myofibroblasts (Olumi et al.
1999), and are characterized by the production of
␣-smooth muscle actin. The role of CAFs in tumor progression was highlighted by several experiments demonstrating that fibroblasts in tumor stroma have unique
cancer-promoting properties compared with fibroblasts
elsewhere in the body. Early studies determined the effect on tumor progression after analyzing grafts of tumorigenic epithelial cells mixed with either normal fibroblasts or fibroblasts that were immortalized, transformed, or tumor-associated (Camps et al. 1990; Gleave
et al. 1991; Atula et al. 1997). More recent studies in
which CAFs were coimplanted with nontumorigenic
prostate epithelial cells showed that these activated fibroblasts could induce tumorigenesis in immunocompromised mice (Hayward et al. 2001). Similarly, CAFs
isolated from invasive human breast carcinomas were
shown to be more competent than normal fibroblasts in
promoting growth of breast cancer cells in a murine
model of breast carcinoma (Orimo et al. 2005). This effect was shown to be largely due to increased secretion of
the stromal-derived chemokine stromal-derived factor-1
(SDF-1) by fibroblasts. SDF-1 can enhance tumor progression by directly stimulating the growth of carcinoma
cells expressing its cognate receptor, CXCR4, and by
initiating the recruitment of angiogenesis-enhancing
CXCR4+ endothelial progenitor cells (EPCs) (Orimo et al.
2005). The SDF-1–CXCR4 axis utilized by activated fibroblasts also directly promotes tumor cell motility
based on chemokine gradients of SDF-1 and CXCR4 expression on most tumor cells.
Besides the role of the SDF-1–CXCR4 axis, relatively
little is known about the molecular determinants that
enable CAFs to promote tumor and stromal cell migration. In response to tumor cell stimulation, the production of fibronectin, a key extracellular adhesion molecule, may increase, promoting the migratory capability
of fibroblasts themselves as well as certain tumor types.
Various fibronectin isomers arise through alternate
splicing of three exons from one gene locus. During normal physiology, fibronectin isoforms, including extra domain A (ED-A) and extra domain B (ED-B) regions, are
expressed at low levels; however, pathological conditions can significantly up-regulate isoforms containing
these domains. As such, invasive tumors are well known
to express isoforms containing ED-A and ED-B domains
(Oyama et al. 1989; Midulla et al. 2000; Castellani et al.
2002; Mhawech et al. 2005). A unique truncated isoform
of fibronectin has also been shown to be produced by
�Downloaded from genesdev.cshlp.org on September 6, 2014 - Published by Cold Spring Harbor Laboratory Press
Migratory neighbors and distant invaders
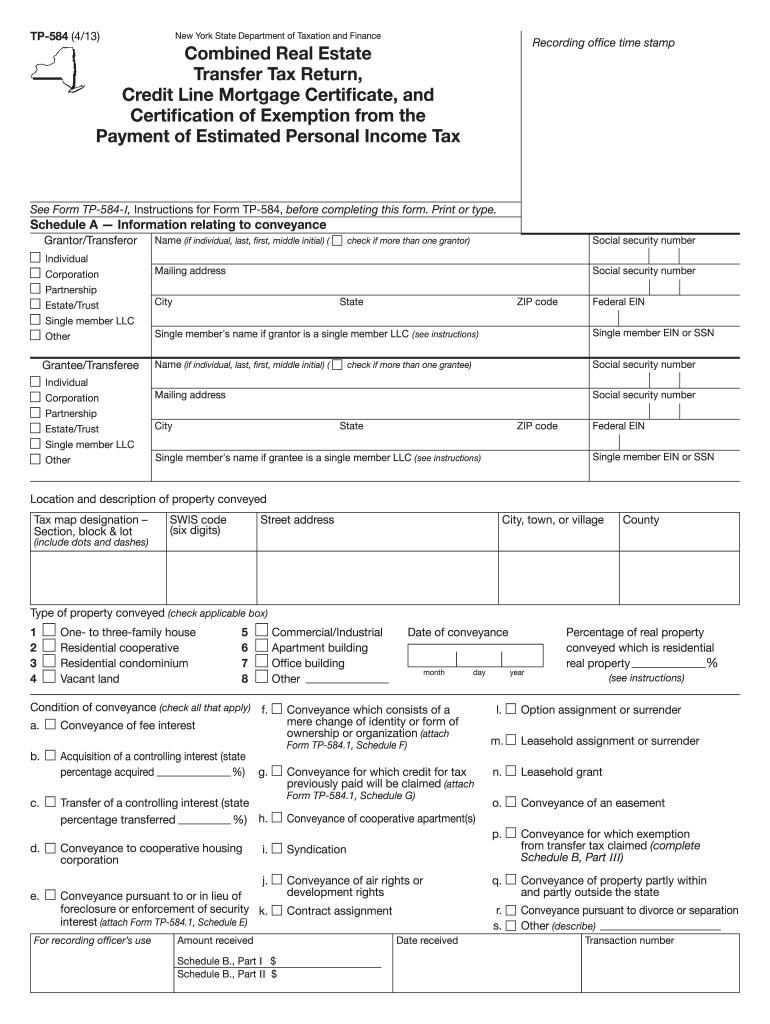
Figure 1. Stromal cell recruitment at primary
and metastatic sites. (A, top left) Early-stage stromal cell recruitment at the primary tumor includes immune infiltrates such as TEMs, TAMs,
BMDCs (HPCs and EPCs), MDSC cells, and recruited CAFs. (Top middle) The production of
matrix proteases and secretion of proangiogenic
chemokines promotes local endothelial cell proliferation and chemotaxis. Blood vessel maturation is promoted via pericyte investment at vascular endothelium, although vessels remain
leaky and disorganized. (Top right) Intravasation
of tumor cells into the circulation, as well as invasion into surrounding tissue, is mediated by
paracrine signaling exchange between fibroblasts, macrophages, and tumor cells. (B, bottom
left) Stromal cell alterations at distant future
metastatic organs include the activation of fibroblasts and the recruitment of HPCs and myeloid
precursor cells. (Bottom middle) The secretion of
inflammatory chemokines and matrix-degrading
enzymes results in tumor cell adherence and proliferation at these sites. (Bottom right) Finally,
the acquisition of blood supply via EPC and EC
recruitment results in the progression of micrometastatic to macrometastatic disease.
embryonic fibroblasts and CAFs and is capable of inducing both tumor and fibroblast cell migration (Schor et al.
2003). These studies suggest an active role of distinct
fibronectin isoforms in promoting tumor and CAF migration.
It is still under debate whether these stromal fibroblasts are recruited into the tumor and subsequently activated by tumor cells into myofibroblasts in order to
support growth, or alternatively, tumor progression is
accelerated as a physiological response to a previously
altered resident stromal environment (Farber 1984; Barcellos-Hoff 1998; Tlsty 1998; Bissell and Radisky 2001).
CAFs may be derived from several different mobilized
cell types, including normal fibroblasts, preadipocytes,
smooth muscle cells, or BM-derived cells (BMDCs) (Ishii
et al. 2003; Direkze et al. 2004). It is also apparent that
there may be several different fibroblast populations associated with tumors with both overlapping and
nonoverlapping expression patterns of markers such as
␣SMA, PDGFR, and NG2 (Sugimoto et al. 2006). These
different sets of markers most likely delineate unique
cellular populations, including myofibroblasts and pericytes, with separate functions in tumor progression. Understanding the molecular events for the generation of
CAFs from normal fibroblasts in either distant or local
environments is one of the queries that remain unresolved.
Infiltrating inflammatory cells
One of the most well-characterized types of tumor-infiltrating inflammatory cells is the macrophage, or tumorassociated macrophage (TAM) (Nagasawa et al. 1996).
Since the late 1970s, the infiltration of TAMs has been
well documented and, for the most part, associated with
poor prognosis. TAMs associated with solid tumor tissue
have been reported to constitute up to 50% of the tumor
mass and have strong implications in tumor progression
and metastasis (Kelly et al. 1988; Leek et al. 1994).
Colony-stimulating factor 1 (CSF-1) is the main growth
factor associated with macrophage survival, proliferation, differentiation, and chemotaxis. Importantly, CSF1-deficient mice lack macrophages and have significantly lower rates of tumor progression and metastasis
formation in models of breast cancer (Lin et al. 2001). In
breast cancer patients, CSF-1 was expressed significantly
in 74% of the tumors associated with poor prognosis
(Scholl et al. 1994). Thus, recruitment of TAMs to tumor
sites via CSF-1 and other chemokines appears to be crucial for tumor progression in many types of cancers (Pollard 2004).
The role of TAMs at the primary tumor is multifaceted and, in many cases, provides a supportive environment for pre-existing malignant cells. However, there is
an increasing amount of evidence supporting the role of
GENES & DEVELOPMENT
561
�Downloaded from genesdev.cshlp.org on September 6, 2014 - Published by Cold Spring Harbor Laboratory Press
Wels et al.
TAMs in stimulating tumor growth and inducing oncogenic mutations in surrounding epithelial cells associated with the earliest stages of carcinogenesis. Indeed,
TAMs are likely recruited to tumor sites as a part of an
innate immune response, and their continuous presence
parallels chronic inflammation, which can be a causative
event for many types of cancer. TAMs can produce high
amounts of reactive compounds, including reactive oxygen and nitrogen species that can interact with DNA,
inducing mutations in surrounding epithelium (Maeda
and Akaike 1998; Lin et al. 2001). This property may
explain mutations seen in local tumor endothelium and
stromal cells (Pelham et al. 2006). Alternatively, TAMs
can produce cytokines that are capable of inducing genetic abnormalities. For instance, generation of migration inhibitory factor (MIF) suppresses p53 transcription
in tumor cells, resulting in defective DNA damage repair
and the accumulation of genetic mutations (Hudson et
al. 1999). TAMs can also produce several growth factors
capable of directly promoting the growth of tumor cells.
These include fibroblast growth factor (FGF), hepatocyte
growth factor (HGF), epidermal growth factor (EGF),
platelet-derived growth factor (PDGF), and transforming
growth factor- (TGF-) (Pollard 2004). EGF appears to
be especially important in many types of cancers, including breast cancer, in which it has been shown to enhance
tumor-cell migration via direct regulation of integrinbinding focal adhesion proteins, tensin-3 and cten (Katz
et al. 2007). Together, these studies provide a substantial
link between inflammation associated with macrophage
infiltration and tumorigenesis.
As the number of studies on TAMs grows, it has become clear that characteristics bestowed upon TAMs in
the literature likely describe a heterogeneous population
of cells whose common origin is still controversial.
Likely precursors of TAMs are monocytes that are actively recruited to the tumor from the blood. Monocytes
were originally shown to be recruited to these sites in
response to a tumor-derived chemokine, CC chemokine
ligand 2 (CCL2/MCP-1), where they then differentiated
into TAMs (Mantovani et al. 2002). Subsequent studies
have identified additional factors involved in attracting
monocytes to the tumor. Chemokines such as CCL2,
CCL5, CXCL8/IL-8, and SDF-1 expressed by tumor cells,
fibroblasts, endothelial cells, and TAMs act as monocyte
chemoattractants (Murdoch et al. 2004). Cytokines and
growth factors, including CSF-1, vascular endothelial
growth factor-A (VEGF-A), and placental growth factor
(PlGF) have also been implicated in initiating monocyte
infiltration (Barleon et al. 1996; Goswami et al. 2005;
Nakao et al. 2005). In addition to promoting cell migration of peripheral monocytes to the tumor microenvironment, certain chemoattractants may also indirectly
enhance monocyte infiltration through indirect means.
For instance, both CCL2 and CCL5 have been shown to
stimulate monocytes to secrete MMP-9, MMP-19, and
uPA, which act to degrade the basement membrane and
ECM components to further promote monocyte infiltration (Cross and Woodroofe 1999; Azenshtein et al. 2002;
Locati et al. 2002; Robinson et al. 2002). The accumula-
562
GENES & DEVELOPMENT
tion of TAMs into hypoxic regions of tumors is well
documented and is likely regulated by a hypoxic-mediated chemoattractive gradient involving hypoxia-inducible factor 1 (HIF-1)-induced growth factors such as
VEGF (Murdoch et al. 2004). Not surprisingly, high expression of monocyte chemoattractants is associated
with increased macrophage infiltration (Sica et al. 2006).
Thus, strategies to prevent TAM migration to the tumor
microenvironment are under investigation. Recent work
has implicated angiostatins in inhibiting TAM recruitment, acting to block migration by disruption of actindriven filipodia and lamellipodia (Perri et al. 2007). Alternately, given the ability of macrophages to home into
the tumor microenvironment, several studies have aimed
to use TAMs as delivery vehicles for anti-tumor genes including IFN-␥, CSF-1, or the immunosuppressive and antiangiogenic cytokine IL-10 (Murdoch et al. 2004).
Recruited stromal players in angiogenesis
The expansion of a tumor mass beyond a microscopic
size is dependent on its ability to obtain its own blood
supply. Tumor vasculature can be developed through angiogenesis, the sprouting of new blood vessels, or cooption of pre-existing vessels (Hanahan and Folkman
1996). The formation of new vessels within the tumor
requires the proliferation and directional migration of
endothelial cells through basement membrane and perivascular stroma toward proangiogenic stimuli. Endothelial cell migration occurs via chemotaxis (migration toward a gradient of soluble chemoattractants such as
VEGF-A, bFGF [FGF-2], or angiopoietins), haptotaxis
(migration toward a gradient of immobilized ligands
present in the ECM), and/or mechanotaxis (migration
activated in response to fluid shear stress induced by
blood flow) (Lamalice et al. 2007). Lymph vessel recruitment is also a critical factor in metastatic spread, as
many types of cancers first metastasize to sentinel
lymph nodes. VEGF-C-dependent lymphangiogenesis at
the primary tumor as well as the expansion of vessel
networks at distant lymph nodes appear to set the stage
for lymphatic tumor spread (Hirakawa et al. 2005, 2007;
Harrell et al. 2007). In addition to endothelial and lymphatic cell migration, there are accumulating reports implicating the involvement of numerous cell types that
play a role in blood vessel development, support, and
growth, including monocytes, TAMs, and pericytes (Fig.
1A). Furthermore, these general mechanisms of endothelial cell movement are likely utilized by other cells such
as fibroblasts, immune cells and pericytes.
Pericytes promote angiogenesis via blood vessel
stabilization
Pericytes are multifunctional cells that closely associate
with the abluminal side of vascular endothelium
through many tight cell–cell contacts that maintain microvessel stability. During angiogenesis, pericytes are recruited to sites of newly forming vessels through an extracellular gradient of PDGF (PDGF-B) (Abramsson et al.
�Downloaded from genesdev.cshlp.org on September 6, 2014 - Published by Cold Spring Harbor Laboratory Press
Migratory neighbors and distant invaders
2003). However, in contrast to pericytes associated with
physiological vessels, pericytes associated with tumor
vessels are less abundant and exhibit an abnormal phenotype. This abnormality contributes to the leakiness
associated with neovessels (Jain and Booth 2003), however, it is generally agreed that pericytes play a supportive role. Accordingly, pericytes recently have become an
attractive target for anti-angiogenic therapy (Jain and
Booth 2003; Baluk et al. 2005). Indeed, by blocking
VEGF-A and PDGF pathways, studies combining target
strategies for both endothelial cells and pericytes have
shown promising anti-tumor and anti-angiogenic effects
(Bergers et al. 2003). These blocking studies illustrate the
critical and complex role that pericytes play in tumor
progression and suggest that there may be yet-unknown
mechanisms that these cells possess to promote tumorigenesis.
Inflamed players in angiogenesis
TAMs have also been shown to regulate the switch of a
tumor to an angiogenic stage. Although anti-angiogenic
functions of macrophages have been reported, TAMs
generally play a proangiogenic role. In the polyoma
middle T oncoprotein model of mammary tumors, a significant infiltration of macrophages occurs at stages directly preceding those changes associated with angiogenesis (Lin et al. 2003). When given tumors, mice deficient
in macrophages, through genetic deletion of the CSF-1
gene, manifest a delayed angiogenic switch (Lin et al.
2006). TAMs are an important producer of VEGF-A
within the tumor (Leek et al. 2000; Lewis et al. 2000),
which may be regulated by hypoxia as well as CSF-1
activation. Transgenic mice made to express GFP under
the control of the human VEGF-A promoter illustrate
that both stromal cells as well as BM-derived macrophages are a large source of this growth factor (Fukumura
et al. 1998). The release of MMPs that break down the
ECM also serves as a mechanism to release bound VEGFA. TAMs synthesize urokinase-type plasminogen activator (uPA), which acts to break down the ECM and may
also serve to function during vascular remodeling
(Hildenbrand et al. 1995). TAMs tend to infiltrate regions
of poor vascularization, which induces transcriptional activation of HIF-1- and HIF-2-regulated promoters, resulting
in the up-regulation of proteins such as VEGF-A, MMPs,
interleukins, and chemokines. Thus, it appears that TAMs
not only function to promote vascular sprouting through
the direct or indirect release of angiogenic factors, but also
provide enzymes capable of vascular remodeling after vessel formation.
A population of peripheral, tumor-infiltrating monocytes, considered precursors to TAMs, has been shown
to play an essential role in angiogenesis as well. Monocytes expressing the angiopoietin receptor Tie2, referred
to as Tie2-expressing monocytes (TEMs), associate
closely with tumor blood vessels. Elimination of TEMs
by means of a suicide gene significantly impairs tumor
growth and vascularity in mouse glioma models (De
Palma et al. 2005). Although the molecular mechanisms
behind the proangiogenic role of TEMs need to be elucidated, the human counterpart of TEMs has been identified recently in the peripheral blood of cancer patients,
with angiogenic activity in xenotransplanted human tumors (Venneri et al. 2007). Thus, TEMs represent a distinct myeloid subpopulation of monocyte/macrophages
that may prove to be an attractive anti-angiogenic target.
Young and restless: BM-derived precursors
in angiogenesis
EPCs are BMDCs mobilized in response to chemotherapy, injury, ischemia, or tumor growth (Kopp et al.
2006). During early stages of tumor growth, cytokines,
including VEGF-A, act to mobilize EPCs from the BM to
become circulating endothelial progenitor cells (CEPs),
ultimately infiltrating and incorporating into the newly
forming tumor vasculature (Lyden et al. 2001). Although
still under debate, the cell surface antigens used to identify these cells include markers for primitive hematopoietic cells as well as endothelial cells including c-kit,
CD133, Sca-1, VE-cadherin, VEGFR-2, and endoglin
(Rafii and Lyden 2003; Kopp et al. 2006; Case et al. 2007).
The identity and relative contribution of EPCs to newly
forming tumor vasculature have been less obvious in certain tumors, with some reports detecting only minimal
contribution to tumor vessels (Voswinckel et al. 2003;
Gothert et al. 2004; He et al. 2004; Ziegelhoeffer et al.
2004; De Palma et al. 2005; Kopp et al. 2006). However,
recent reports have provided further evidence supporting
the involvement of these cells in early blood vessel development during neoangiogenesis (Nolan et al. 2007;
Gao et al. 2008). Using genetically marked GFP+ BM
cells in a series of BM transplantation experiments, Nolan et al. (2007) have demonstrated that BM-derived
EPCs, as defined by GFP+ VE-cadherin+ CD31low
CD11b−, comprise ∼25%–35% of total endothelium during the early stages of tumor growth. High-resolution
confocal micrography was used to show physical incorporation of EPCs in three separate syngeneic as well as
one spontaneous tumor model. Finally, specific targeting
of EPCs with an ␣-particle-emitting antibody for VE-cadherin, which fails to target mature endothelial cells, impaired tumor growth and reduced levels of vascularization (Nolan et al. 2007). These reports confirm that, at
least in the early phases of angiogenesis, BM-derived
EPCs are a critical component of the forming vasculature.
Just as the up-regulation of local chemoattractants
within the BM microenvironment leads to tumor cell
homing and retention within the bone, the release of
secreted growth factors and chemokines by the tumor
also results in the proliferation and recruitment of BMderived accomplices to support angiogenesis and metastasis. In addition to VEGF-A, tumor cells may also secrete PlGF, which signals exclusively through VEGFR-1
and is associated with more aggressive disease (Li et al.
2006). VEGF receptor signaling directs tumor growth and
angiogenesis, recruiting VEGFR-1+ hematopoietic progenitor cells (HPCs) in addition to VEGFR-2+ EPCs to
GENES & DEVELOPMENT
563
�Downloaded from genesdev.cshlp.org on September 6, 2014 - Published by Cold Spring Harbor Laboratory Press
Wels et al.
neoangiogenic sites in the tumor (Lyden et al. 2001). The
necessity of both HPCs and EPCs for tumor vasculature
is demonstrated in the angiodeficient Id (inhibitor of differentiation) mutant mouse model, which is resistant to
tumor progression due to a failure of BM progenitor mobilization and consequential defective angiogenesis.
Transplantation of wild-type BM or VEGF-mobilized
stem cells restores tumor angiogenesis and growth in
this model (Lyden et al. 1999). In addition to EPC incorporation into neovessels, VEGFR-1+ HPCs also appear to
lie in close association with forming vasculature. Indeed,
VEGFR-1 inhibition diminished investment of vessels
with perivascular cells, suggesting that VEGFR-1+ HPCs
confer vessel stability and promote tumor progression.
One mechanism by which HPCs may promote angiogenesis is by the paracrine release of angiogenic factors,
thereby enhancing the recruitment and incorporation of
EPCs to new tumor vessels (Grunewald et al. 2006). Activated HPCs can release angiogenic factors such as
VEGF-A, PDGF, angiopoietins, and brain-derived neurotrophic factor (BDNF), which serve to enhance vessel
formation and stability (Donovan et al. 2000; Otani et al.
2002; Okamoto et al. 2005).
There is evidence that other BM-derived immature
cells such as immunosuppressive CD11b+ GR1+ myeloid
cells may also contribute to neovascularization. Presently referred to as myeloid-derived suppressor cells
(MDSCs), these undifferentiated myeloid cells, expressing CD11b and Gr-1, accumulate rapidly in the primary
tumor microenvironment (Bronte et al. 1999; Melani et
al. 2003; Kusmartsev et al. 2004; Sinha et al. 2005; Sica
and Bronte 2007). Inherent anti-VEGF refractoriness is
associated with infiltration of CD11b+ Gr1+ cells, which
indirectly promotes and stabilizes new blood vessels in
the primary tumors (Shojaei et al. 2007). Several studies
also support the notion that MDSC precursors can infiltrate tumors and differentiate into F4/80+ TAMs, furthering support for their proangiogenic role (Kusmartsev
et al. 2004, 2005). In addition, MDSCs have also been
shown to have a profound effect on immune evasion of
tumors in their undifferentiated state. As a mixture of
immature monocytic and granulocyte populations, these
cells have high potential to suppress immune response
both in vitro and in vivo (Kusmartsev and Gabrilovich
2006; Sica and Bronte 2007).
Stromal–tumor cell interactions that promote invasion
and metastasis
The interplay of tumor cells and stromal fibroblasts at
the invasive front can result in distinct migratory signals
for both cell types. Also, tumor cells that have acquired
genetic alterations can confer signals that enhance migration of local tumor-associated host cells as well as in
distant sites such as the BM.
CAFs and the epithelial-to-mesenchymal transition
(EMT)
In addition to promoting angiogenesis and the proliferative capacity of tumor cells, CAFs have been implicated
564
GENES & DEVELOPMENT
in enhancing tumor cell invasiveness, possibly through
the induction of EMT. EMT, associated with the loss of
E-cadherin-based cell adhesions and the acquisition of
migratory and invasive properties, is now well recognized as a key determinant for cancer progression. Although cell-autonomous mechanisms for EMT exist,
several exogenous factors have been shown to promote
EMT of carcinoma cells, many of which are produced by
CAFs (Bhowmick et al. 2004; Mueller and Fusenig 2004;
Kalluri and Zeisberg 2006). Breast carcinoma cells incubated with CAF-conditioned media have been characterized by a loss of E-cadherin-dependent adhesion and enhanced motility (Lebret et al. 2007). Growth factors such
as FGF, HGF, and members of the TGF- superfamily, all
of which are produced by CAFs, have been shown to be
important stimuli of EMT (Lochter et al. 1997; Muller et
al. 2002; Thiery 2002; Kalluri and Zeisberg 2006). In addition, the secretion of fibroblast-derived matrix-degrading enzymes plays an essential role in EMT and subsequent tumor invasion. MMP-1, MMP-2, MMP-3, MMP9, MMP-11, MMP-14, and uPA have all been shown to be
secreted by fibroblast-like cells in the tumor microenvironment in mouse models, serving to mediate the breakdown of basement membrane barriers (Okada et al. 1995;
Heppner et al. 1996; Friedl and Brocker 2000; Stuelten et
al. 2005). MMP-3, in particular, is highly expressed in
activated fibroblasts and has been shown to promote normal epithelial cells to undergo EMT via cleavage of the
extracellular domain of E-cadherin (Lochter et al. 1997).
MMP-1 has also been shown to promote tumor cell migration and invasion by cleaving and activating the protease-activated receptor PAR1 expressed in breast carcinoma cells (Boire et al. 2005).
Undifferentiated BM cells: mesenchymal stem cells
(MSCs) and CD11b+ GR-1+ MDSCs
MSCs are pluripotent BMDCs that give rise to a variety
of connective tissue cell types including those that form
bone, adipose, cartilage, and muscle (Pittenger et al.
1999). Recent studies have shown that BM-derived
MSCs are recruited in significant number to primary tumor sites and contribute to invasion and metastasis of
several tumor cell lines (Hall et al. 2007; Karnoub et al.
2007). Using a human breast cancer xenograft model,
Weinberg and colleagues (Karnoub et al. 2007) have
shown that the metastatic potential of breast cancer cell
lines becomes greatly enhanced when coinjected with
MSCs. Karnoub et al. (2007) demonstrated that paracrine
signaling events induce a transiently enhanced metastatic capability in tumor cells, suggesting that metastatic and invasive phenotypes are contextual and require direct MSC association. Specifically, MSC-derived
CCL5 appears to be an essential factor, as shRNA knockdown of its receptor (CCR5) in tumor cells abrogates
metastasis formation. Although overexpression of
CCL5, an important chemokine involved in monocyte/
macrophage recruitment, appears not to affect the levels
of macrophage investment at the primary tumor site, it
will be interesting to determine the effect of MSC-de-
�Downloaded from genesdev.cshlp.org on September 6, 2014 - Published by Cold Spring Harbor Laboratory Press
Migratory neighbors and distant invaders
rived CCL5 expression on other CCR5-expressing stromal cells at distant secondary sites.
Convincing evidence supporting the role of another
immature BMDC type, CD11b+ Gr-1+ MDSCs, in tumor
invasion and metastasis has emerged recently. Using a
mammary carcinoma model lacking the type II TGF
receptor gene, Moses and colleagues (Yang et al. 2008)
have demonstrated a significant infiltration of MDSCs at
the tumor invasive front. These cells appear to be recruited via SDF-1/CXCR4 and CXCL5/CXCR2 axes and
contribute to tumor invasion through metalloproteinase
secretion (Yang et al. 2008). Given the implications of
CD11b+ GR-1+ MDSCs in suppressing tumor immunosurveillance, angiogenesis, and tumor invasion, targeting
the homing or function of this cell type may prove to be
therapeutically effective.
TAMs break down barriers and elicit movement
In later stages during tumor progression, tumor cells
must break down basement membrane and ECM components that act to provide structural integrity in order
to invade surrounding tissue and intravasate into the circulation. Macrophages have been reported to be present
at high frequency at the invasive front, where the breakdown of ECM occurs (Fig. 1A). TAMs accomplish this by
secreting several MMPs, including MMP2 and MMP9,
which degrade matrix components such as collagen,
laminin, and fibronectin. They can also secrete several
other factors—such as TGF, urokinase plasminogen activator, tissue-type plasminogen activator, and cathepsins—that also play a role in the degradation of the ECM.
In addition to secreting proteases and factors to break
down the ECM, macrophages have been shown to directly promote the invasion of tumor cells. Multiphoton
imaging techniques have been used to directly visualize
the interaction between tumor cells, macrophages, and
surrounding blood vessels (Condeelis and Segall 2003;
Wyckoff et al. 2007). These studies have suggested that
tumor cells are attracted to macrophages lying in close
association with vessels. This attraction is thought to be
mediated through a paracrine signaling loop between tumor cells and macrophages, where tumor cells secrete
CSF-1, leading to macrophage secretion of EGF, which
acts as a chemoattractant for tumor cells (Goswami et al.
2005). Inhibiting either CSF-1 or EGF signaling blocks
the migration of both cell types in vivo. Thus, it is believed that activated CSF-1/EGFR signaling induces coordinated polarization and cell migration of both macrophages and tumor cells. These studies may help explain
why high expression of CSF-1 in patients correlates with
poor outcome (Scholl et al. 1994). A similar paracrine
loop is likely involved between tumor cells and activated
fibroblasts within the tumor. This is shown in irradiated
fibroblasts, where coinjection with lung, mammary, or
pancreatic epithelial cells can alter the growth factor
profile of the fibroblasts with a concomitant increase in
the invasiveness of tumor cells (Barcellos-Hoff and Ravani 2000; Bhowmick et al. 2004; Ohuchida et al. 2004).
Pericytes suppress intravasation
Pericytes help maintain relative vascular integrity during angiogenesis, and studies have implicated pericytes
as negative regulators of metastasis. Xian et al. (2006)
show that mice deficient in neural cell adhesion molecule (NCAM), which do not normally produce metastases in the RIP-TAG model of tumorigenesis, develop
metastases to distant organs and lymph nodes due to
deficiencies in pericyte recruitment and function. After
manipulating NCAM expression in two independent tumor models, Xian et al. (2006) found that NCAM production by tumor cells is essential for pericyte recruitment and integration into vessel walls. Importantly,
pericyte function appeared to correlate with levels of metastases in both models. Furthermore, tumors implanted
in mice deficient in PDGF-B, which have disrupted pericyte recruitment, show enhanced metastatic progression. Thus, these experiments provide compelling evidence supporting the role of pericytes in preventing tumor metastasis. Given the opposing roles of pericytes in
angiogenesis and metastasis, therapeutic targeting of
these cells may be a double-edged sword and may only
prove beneficial in the right temporal conditions.
The platelet shuttle
Platelets, in addition to immune and endothelial cells,
may play an important role in tumor metastasis. The
first event in tumor cell invasion at distant sites is lodgment at and adhesion to the local vasculature, and the
formation of platelet microthrombi has been implicated
in this process. Platelets may encompass disseminating
tumor cells while in the circulation, acting as a “shield”
to prevent immune attack. More recently, platelets have
emerged as key players in directing homing and retention signals for BMDCs and tumor cells. Platelet-deployed SDF-1␣ was shown to be critical for the recruitment and retention of CXCR4+ HPCs and EPCs in revascularization of ischemic tissue and to sites of tumor
angiogenesis (Jin et al. 2006). Local activation and release
of SDF-1␣ by platelets may also govern migration patterns of CXCR4+ tumor cells (Jin et al. 2006; Massberg et
al. 2006). Furthermore, platelets are major storage vehicles for both pro- and anti-angiogenic factors (Mohle et
al. 1997; Li et al. 2001; Kopp and Rafii 2007). Megakaryocytes and platelets carry the potent natural anti-angiogenic factor thrombospondin, identified as a determinant
of the angiogenic phenotype. In keeping with the cell
movement from primary tumor to distant metastatic
sites and mobilization of immune cells from the BM to
each of these sites, platelets may shuttle growth factors
from one site to the other. This mechanism further connects these sites while transmitting malignant phenotype from normal mechanisms into pathological ones,
thus confirming the systemic nature of these processes.
Collective cell movement: making tracks
The dialog between tumor cells and stroma conferring
migratory properties raises the possibility of a collection
GENES & DEVELOPMENT
565
�Downloaded from genesdev.cshlp.org on September 6, 2014 - Published by Cold Spring Harbor Laboratory Press
Wels et al.
of cells, including tumor cells and stroma, moving in
concert from the primary tumor site to new metastatic
stations. It has been recently suggested that stromal fibroblasts and endothelial cells may acquire genetic alterations similar to those seen in tumor cells and this
coevolution may provide growth and migratory advantages to both cell types (Pelham et al. 2006). In vivo,
migrant cell clusters retain cell–cell junctions, protrude
into adjacent tissue driven by leading “pathfinder” cells,
and can be detected in lymphatic vessels (Carr 1983) and
in peripheral blood (Liotta et al. 1976; Brandt et al. 1996;
Friedl and Brocker 2000). Such coordinated cell migration of neoplastic cell clusters from primary explants can
also be visualized using time-lapse videomicroscopy in
three-dimensional (3D) collagen matrices (Friedl et al.
1995). Additionally, an intriguing study by Gaggioli et al.
(2007) has uncovered a key mechanism by which these
stromal “pathfinder” cells and invasive tumor cells interact. Using an in vitro 3D organotypic culture, Gaggioli et al. (2007) observed that fibroblasts enable collective invasion of squamous cell carcinoma (SSC) cells by
both proteolytic and structural modification of the ECM,
thus creating a path through which cancer cells can
travel (Gaggioli et al. 2007). Proteolysis of the ECM by
fibroblasts appears to be dependent on ␣3 and ␣5 integrins as well as Rho regulation of myosin light chain
(MLC) activity (Gaggioli et al. 2007). Further evidence
supporting the idea of leading cells paving the way for
collective tumor cell migration was provided by studies
using time-resolved confocal microscopy by Wolf et al.
(2007). These authors showed that the collective invasion of HT-1080 fibrosarcoma cells involves anterior
physical fibrillar collagen matrix remodeling and posterior proteolytic fiber breakdown by leading cells, ultimately resulting in the production of an oriented scaffold
(Wolf et al. 2007). This collagen scaffold can then be used
by chains of following cells. Collectively, these studies
support a model for multicellular migration of tumor
Figure 2. Niche-to-niche migration of BM and tumor
cells. The transit of BM and tumor cells from their respective niches is a multidirectional pathway. Hematopoietic cells are mobilized from the BM niche in response to tumor-secreted chemokines and subsequently home to both the primary tumor microenvironment and peripheral niches. BMDCs homing to
the primary tumor niche may remain in an undifferentiated state in the form of HPCs, EPCs, MSCs, or GR-1+
CD11b+ MDSCs; or may differentiate into more specialized cell types including TAMs. Early BMDCs in
transit to premetastatic peripheral niches likely possess
an undifferentiated status as HPCs or myeloid-precursor cells, and at later stages involve homing of EPCs.
Metastasizing tumor cells subsequently travel to peripheral niches occupied by BMDCs.
566
GENES & DEVELOPMENT
cells involving either tumor or stromal cell-mediated
generation of a pathway by which following groups of
tumor cells can travel.
Activation and mobilization at distal sites
Changes in the BM microenvironment
Cancer cells secrete a multitude of chemokines and
growth factors that not only induce changes in local tumor stroma, but also direct significant changes in the
BM microenvironment. An intricate vascular network
and a dense mesenchymal-derived stroma cell scaffold
exist within the BM. The stromal matrix includes many
essential growth factors, cytokines, chemokines, and
ECM components that regulate HSC/HPC proliferation
and differentiation, a process that can be intensely amplified during tumor burden.
There is a significant amount of overlap in the molecular machinery between metastasizing tumor-initiating cancer cells and physiological HSCs. Therefore, it is
not surprising that many cancers show a proclivity to
establish in bone and BM, the natural home of HSCs (Fig.
2). Throughout development and the adult life span, the
SDF-1 chemokine receptor axis is the master regulator of
HSC/HPC homing and retention, both within the BM
and at sites in the periphery (Nagasawa et al. 1996; Ara et
al. 2003; Dar et al. 2005). As with genetic profiling, specific chemokine repertoires may predict tissue-specific
tropism in tumor metastasis. SDF-1 gradients mediate
HSC retention within BM niches, and growing evidence
suggests that CXCR4-expressing cancer cells home to
bone in a similar fashion, where they may lodge in the
pre-existing supportive stromal microenvironment
(Muller et al. 2001; Kaifi et al. 2005). Bone expresses
particularly high levels of SDF-1, and osteotropic cancers
such as breast, ovarian, prostate, and neuroblastoma metastasize to bones in a CXCR4-dependent manner (Ge-
�Downloaded from genesdev.cshlp.org on September 6, 2014 - Published by Cold Spring Harbor Laboratory Press
Migratory neighbors and distant invaders
minder et al. 2001; Muller et al. 2001; Sun et al. 2003;
Porcile et al. 2004).
Furthermore, neutralization of the SDF-1/CXCR4 axis
can block prostate metastasis and growth in osseous
sites (Nakamura et al. 2006). Differentiating osteoclasts
constitutively produce chemokine CCL22 and may promote bone metastasis of lung cancer cells expressing its
receptor CCR4 (Nakamura et al. 2006). Similarly, chemokine CCL12 also mediates site-specific metastatic
homing of CCR7+ breast cancer cell lines (Moore 2001;
Muller et al. 2001). Liquid tumors also display site-specific homing to microdomains within marrow, and this
may result in dormant “residual” disease and consequent relapse following treatment. High expression of
SDF-1 in perivascular microdomains within the BM can
mediate highly specific localization patterns of acute
lymphoblastic leukemia cells expressing CXCR4 (Sipkins et al. 2005).
In addition to producing large amounts of SDF-1, osteoblasts also express anchorage molecules—including
angiopoietin (Ang-1) and osteopontin (Opn)—that contribute to tumor cell recruitment to bone. Opn, often
characterized as a cytokine, is a glycophosphoprotein
with multiple functions including the ability to stimulate HSC and osteoclast adherence to bone matrix (Asou
et al. 2001). At the endosteal surface, Opn is a key molecule in the trans-marrow migration, retention, and
negative regulation of HSC cycling within the osteoblastic niche (Nilsson et al. 2005). Recently, substantial data
have linked Opn with the regulation of metastatic spread
in tumors of the breast, prostate, colon, and liver (Wai
and Kuo 2004), and it is consistently found to be highly
expressed within metastatic cells and in surrounding tissue stroma (Kang et al. 2003). Induced expression of recombinant Opn confers a migratory and invasive phenotype in human mammary epithelial cells (Tuck et al.
2003).
Far-away fibroblasts: setting the scene
Fibroblasts at the metastatic site, similar to fibroblasts
associated with the primary tumor, appear to provide an
environment supportive of tumor cell proliferation (Fig.
1B). Enhanced fibronectin expression and an increase in
PDGFR-expressing cells were localized to premetastatic
sites early in tumor progression, prior to the arrival of
BM-derived HPCs (Kaplan et al. 2005). These findings
were likely mediated by tumor-secreted growth factors
as similar effects were seen with administration of B16
melanoma-conditioned media. Several studies of hepatic
metastasis of B16 melanoma have shown that factors
secreted by melanoma cells appear to activate hepatic
stellate cells to a myofibroblast-like state associated
with SMA expression and cytoskeletal changes (Olaso et
al. 1997). Thus, active infiltration of this myofibroblast
population is likely induced by melanoma-secreted factors in order to support the growth of incoming tumor
cells. Follow-up studies by Olaso et al. (2003) have described a role for these activated hepatic stellate cells in
promoting the angiogenic switch of nascent hepatic me-
tastases. The infiltration of activated myofibroblasts precedes the recruitment of vascular endothelial cells in the
hypoxic avascular metastatic environment. Melanoma
signals, as well as hypoxic conditions, were shown to
induce VEGF-A production by myofibroblasts, thus promoting angiogenesis and transition to a vascular stage
(Olaso et al. 2003). Further evidence supporting the importance of fibroblast motility in cancer metastasis
comes from tumor studies in mice lacking the S100A4
gene. S100A4 is a member of the S100 family of small
Ca2+-binding proteins, many of which have been implicated in cytoskeletal–membrane interactions, calcium
signal transduction, and cellular proliferation and differentiation (Heizmann et al. 2002). Fibroblasts lacking
S100A4 have impaired motility and invasive properties
compared with wild-type fibroblasts (Grum-Schwensen
et al. 2005). Furthermore, mice lacking S100A4 have impaired tumor development and do not metastasize. Importantly, coinjection of tumor cells with S100A4 (+/+)
fibroblasts restores metastatic capabilities in mice
(Grum-Schwensen et al. 2005). Thus, the ability of fibroblasts to mobilize and actively associate with tumor
cells within the metastatic microenvironment is vital
for tumor cell survival and progression to full-blown metastases.
A paracrine exchange between tumor cells and distant
or local fibroblasts can provide insight into how tumor
cells modulate the microenvironment and potentially
create systemic changes in distant tissues (Fig. 2). Through
the secretion of IL-1, FGF-2, and PDGF, several carcinoma cell lines have been shown to induce HGF secretion from fibroblasts. HGF can then bind to c-Met expressed in many cancer cells and can increase their invasive and migratory capacity (Nakamura et al. 1997).
The MMP inhibitor TIMP-1 may also act as a key regulator of HGF/c-Met signaling through suppression of metalloproteinase-10 (ADAM-10) (Kopitz et al. 2007). Other
paracrine signals involving TGF-, EGF, and insulin
growth factor (IGF), as well as Wnt1, likely mediate mutually supportive cross-talk between the stromal cells
and tumor cells (Bhowmick et al. 2004).
Hematopoietic progenitors and the premetastatic
niche
According to Paget’s theory, the colonization and proliferation of a particular tumor type are dependent on a
receptive microenvironment within distant target organs. This idea is currently of direct relevance, as it addresses one of the most intriguing aspects of malignancy;
that is, the organ specificity of metastatic progression.
The favorable interaction between disseminated tumor
cells and the stromal environment is necessary for survival and eventual outgrowth of macrometastases. A poignant question is: Are future metastatic organs intrinsically permissive for tumor growth, or is “conditioning”
of these sites dictated by primary tumor burden necessary for metastatic colonization? Although tumor-secreted signals, including chemokines and proteases, have
been shown to induce dynamic alterations of the adja-
GENES & DEVELOPMENT
567
�Downloaded from genesdev.cshlp.org on September 6, 2014 - Published by Cold Spring Harbor Laboratory Press
Wels et al.
cent tumor microenvironment, it is now recognized that
systemic changes arise in response to primary tumor
growth. An essential role for BM-derived progenitor cells
in priming distant tissues for tumor cell implantation
and proliferation has recently been revealed (Hiratsuka
et al. 2002, 2006; Kaplan et al. 2005). In response to a
unique array of chemokines released by the primary tumor, specific cells of hematopoietic origin mobilize from
the BM and engraft as cellular clusters into distant organ
tissue before the arrival of tumor cells (Fig. 1B). These
BMDCs express lineage markers such as VEGFR-1, c-Kit,
Sca-1, and CD11b, suggesting an immature status within
the tissue parenchyma (Kaplan et al. 2005). Recruitment
of VLA-4-expressing BMDCs is associated with the local
deposition of fibronectin, providing a highly receptive
environment for circulating tumor cells. Inhibiting the
incorporation of BMDCs to form the premetastatic sites
through antibody administration or depletion of these
cells from the BM was sufficient to block metastatic progression (Kaplan et al. 2005). Importantly, tumor-secreted chemokines were able to orchestrate the formation of the premetastatic niche, thus containing the imprints of the tumor cell necessary to dictate the pattern
of tumor spread.
Mechanisms promoting the homing of both BMDCs
and tumor cells to metastatic sites have come to light
recently. Once present within the target tissue, BMDCs
appear to interact with and alter the surrounding tissue,
in part through the expression of matrix-degrading enzymes such as MMP-9, making a more receptive environment for tumor cell implantation and growth (Hiratsuka et al. 2002; Kaplan et al. 2005). The secretion of
hypoxia-induced factors, such as lysyl oxidase, from the
primary tumor further promotes metastatic growth at
distant sites and may similarly enhance fibronectin production at distant sites prior to tumor cell spread (Kaplan
et al. 2005; Erler et al. 2006; Giaccia et al. 2007). In addition, Hiratsuka et al. (2006) have demonstrated that
primary tumor cells secrete VEGF-A, TGF-, and TNF␣,
which induce the expression of inflammatory chemokines, S100A8 (MRP8/Calgranulin A) and S100A9
(MRP14, Calgranulin B), by both lung epithelium and
myeloid cells in distant premetastatic organs (Hiratsuka
et al. 2006; Rafii and Lyden 2006). These chemoattractants were shown to increase the mobility of Mac1-expressing myeloid cells in a p38-mediated fashion, thus
increasing the infiltration of myeloid cells to premetastatic sites. Similarly, the invasive phenotype of circulating tumor cells appears to be promoted through
MAPK p38-mediated pseudopodia formation (Hiratsuka
et al. 2006). Thus, S100A8 and S100A9 may be an essential pathway necessary for both myeloid and tumor cell
recruitment to future metastatic tissues. Furthermore,
BMDCs also express CXCR4, and their interaction with
resident fibroblasts can induce localized increase of
SDF-1 production, serving as a chemokine gradient and a
docking site for CXCR4+ tumor cells.
Expanding on investigations of the premetastatic
niche at distant sites, recent work has demonstrated evidence for the preconditioning of local lymph nodes as a
568
GENES & DEVELOPMENT
common initial metastatic site for many tumor types.
This metastatic site is proposed to act as a gateway to
distant metastasis (Hirakawa et al. 2007).
Although the role of EPCs at the metastatic site has
not been greatly characterized, there is evidence that this
cell type contributes toward the angiogenic stage after
metastatic initiation (Fig. 1B). Targeting VEGFR-2+ EPCs
via administration of VEGFR-2-blocking antibodies results in the formation of small micrometastases without
vascularization (Kaplan et al. 2005). In addition, recent
studies that inhibit EPC mobilization after metastatic
colonization, via knockdown of Id1, report angiogenesis
inhibition and impaired macrometastasis formation
(Gao et al. 2008; Rafii and Lyden 2008). Such reports
support the idea that recruitment of EPCs is necessary
for vessel formation and maturation to a fully developed
metastatic lesion.
Perspective: the niche as an immature privileged
refuge
BM-derived hematopoietic progenitor and immature myeloid cells (CD11b+ GR-1+) contribute to neo-angiogenesis within the primary tumor and have been found to
promote lymphangiogenesis and metastatic spread in
their strategic location at the invasive edge of the tumor
(Lyden et al. 2001; Yang et al. 2004). Given the association of immature hematopoietic cell types with enhanced tumor progression and metastasis, it is possible
that tumor cells secrete factors that maintain an immature state as a means to promote immune invasion. Immature myeloid cells can suppress differentiation of mature tumor antigen-presenting dendritic cells evading
the host adaptive immune response (Lin et al. 2002).
These data suggest a biological selection for promoting
an immature phenotype, resulting in immune dysfunction and diminished surveillance in response to tumor
cells.
The premetastatic niche, similar to the hematopoietic
stem cell niche within the BM, may also create a microenvironment preventing differentiation of tumor cells. A
niche can alter the cells within its space. Therefore, tumor cells that localize to these sites may be more apt to
grow and survive similar to normal stem cell niche dynamics, where niche occupancy confers a survival advantage to cells. Moreover, these tumor cells may be
altered by this specialized microenvironment and gain
stem-like properties. Such characteristics may promote
further tumor recruitment and immune evasion. Tumor
cell occupation of such a site might, in turn, have a reciprocal role within the microenvironment, altering its
conditions to further promote pathology. In an altered
microenvironment, a so-called pathological niche, cells
can obtain new genetic alterations and acquire new functions leading to tumor promotion, progression, and
metastatic niche formation. The migration of cells from
niche to niche may result in transmission of this deregulation, and such cell dynamics may be central to targeting this process in order to prevent metastatic spread.
Cancer stem cells or pathological niches, like physiologi-
�Downloaded from genesdev.cshlp.org on September 6, 2014 - Published by Cold Spring Harbor Laboratory Press
Migratory neighbors and distant invaders
cal stem cells and their niches, may maintain cells in a
quiescent state and minimize cell division, and can
therefore evade traditional anti-mitotic chemotherapy or
radiotherapy that target cells with a high turnover. For
example, as has been shown in gliomas, cancer stem
cells are resistant to radiotherapy due to an increased
capacity for DNA repair (Liu et al. 2006). This finding
may be a result of reciprocal alterations in tumor cells
and their pathological microenvironment.
Potential therapeutic implications
Scientific advances in the understanding of metastasis
are opening up a new area of cancer therapeutics. In order
for anti-metastatic therapy to be successful, several key
concepts must be incorporated. The cells that mediate
the mobile nature of tumor progression are crucial for
targeting these early and fundamental events. Inhibition
of metastasis requires targeting of both the metastasizing cell and its supportive microenvironment. Recognition that the preparatory changes in the premetastatic
microenvironment occur very early in tumorigenesis
suggests that anti-metastatic agents must be used together with the primary therapy. Furthermore, therapy
that focuses on the dynamic nature of tumors and their
supportive cells may be critical to preventing tumor progression. Therefore, a strategy that manipulates the migrating BMDCs themselves, as well as their signaling
pathways, might prove quite successful. The BMDCs
that home to the tumor neovasculature and premetastatic sites could be used as “magic bullets,” delivery
vehicles for anti-cancer strategies (Arafat et al. 2000).
The feasibility of integrating a suicide gene into BMderived progenitors to reduce tumor size and vascularity
has already been confirmed in several animal studies
(Komarova et al. 2006; Lotem and Sachs 2006). Not only
HPCs and EPCs, but also fibroblasts and stromal progenitors that migrate to tumor sites might prove particularly useful as carriers of oncolytic adenoviruses or as
direct targets of “activated” or genetically altered stromal cells.
Alternatively, targeting the homing mechanisms by
which cancer stem cells migrate to metastatic sites or
the factors that govern the cellular dynamics within
these “pathological niches” may be feasible. Identifying
and inhibiting those cytokines or growth factors, which
promote cellular migration, as recently demonstrated
with antibodies to PlGF (Fischer et al. 2007), may provide an additional arsenal for abrogation of these early
and evolving processes of tumor spread. Characterization of cancer stem cells and their “pathological niches”
in solid malignancies may reveal potential therapeutic
targets to inhibit metastasis.
Conclusion
Although often a late presentation of carcinogenesis, the
metastatic process need not be a final event. The basic
tenets of metastasis as a late event may be, in fact, over-
turned as the evolution of a malignancy is elucidated.
Through a series of small steps leading to subtle changes
in distant tissues, metastasis likely has an early initiation that reflects its true systemic nature. Unraveling
the details of these subtle systemic changes that commence with malignant transformation may lead to a
paradigm shift in the design of therapies and has implications in how host stromal and immune response mediates the development of carcinogenesis as well. Longstanding players in metastatic growth have been neglected in order to focus on the precise detailing of the
migrating cancer cell and the genetic alterations allowing for its dissemination. However, new evidence is
emerging on how supporting cells composing the tumor
microenvironment promote disease progression and metastasis. The underlying mechanisms of how a tumor
cell alters its local and distant microenvironment are
also receiving more attention. Dissecting these individual pieces will provide valuable insights and direct
future investigations. The ecology of a metastatic tumor
includes genetically altered tumor cells and their heterotypic interactions with nonmalignant cells and their
stromal support structure. Focus on the dynamic exchange of cells from local and distant environments, to
the invasive front of the tumor, to the premetastatic and
metastatic niches can provide novel strategies for successfully targeting these processes.
Acknowledgments
This work was supported by NCI R01CA098234 (to D.L.), the
Emerald Foundation (to D.L.), the Nancy C. and Daniel P.
Paduano Fund (to D.L.), the Charles and Meryl Witmer Family
Foundation (to D.L.), the Malcolm Hewitt Wiener Foundation
(to D.L.), National Foundation for Cancer Research (to D.L.),
AHEFA Foundation (to D.L. and R.K.), the Doris Duke Charitable Foundation (to R.K.), Hope Street Kids Foundation (to
R.K.), Charles, Lillian and Betty Neuwirth Scholar Program (to
R.K.), the Butler Foundation (to R.K.), Association for Research
of Childhood Cancer (to R.K.), the American Society of Clinical
Oncology (to R.K.), the Childern’s Cancer and Blood Foundation
(to J.W., R.K., and D.L.), Howard Hughes Medical Institution
(to S.R.), and the National Heart, Lung, and Blood Institution
(to S.R.).
References
Abramsson, A., Lindblom, P., and Betsholtz, C. 2003. Endothelial and nonendothelial sources of PDGF-B regulate pericyte
recruitment and influence vascular pattern formation in tumors. J. Clin. Invest. 112: 1142–1151.
Ara, T., Tokoyoda, K., Sugiyama, T., Egawa, T., Kawabata, K.,
and Nagasawa, T. 2003. Long-term hematopoietic stem cells
require stromal cell-derived factor-1 for colonizing bone
marrow during ontogeny. Immunity 19: 257–267.
Arafat, W.O., Casado, E., Wang, M., Alvarez, R.D., Siegal, G.P.,
Glorioso, J.C., Curiel, D.T., and Gomez-Navarro, J. 2000.
Genetically modified CD34+ cells exert a cytotoxic bystander effect on human endothelial and cancer cells. Clin.
Cancer Res. 6: 4442–4448.
Asou, Y., Rittling, S.R., Yoshitake, H., Tsuji, K., Shinomiya, K.,
Nifuji, A., Denhardt, D.T., and Noda, M. 2001. Osteopontin
GENES & DEVELOPMENT
569
�Downloaded from genesdev.cshlp.org on September 6, 2014 - Published by Cold Spring Harbor Laboratory Press
Wels et al.
facilitates angiogenesis, accumulation of osteoclasts, and resorption in ectopic bone. Endocrinology 142: 1325–1332.
Atula, S., Grenman, R., and Syrjanen, S. 1997. Fibroblasts can
modulate the phenotype of malignant epithelial cells in
vitro. Exp. Cell Res. 235: 180–187.
Azenshtein, E., Luboshits, G., Shina, S., Neumark, E., Shahbazian, D., Weil, M., Wigler, N., Keydar, I., and Ben-Baruch, A.
2002. The CC chemokine RANTES in breast carcinoma progression: Regulation of expression and potential mechanisms of promalignant activity. Cancer Res. 62: 1093–1102.
Baluk, P., Hashizume, H., and McDonald, D.M. 2005. Cellular
abnormalities of blood vessels as targets in cancer. Curr.
Opin. Genet. Dev. 15: 102–111.
Barcellos-Hoff, M.H. 1998. The potential influence of radiationinduced microenvironments in neoplastic progression. J.
Mammary Gland Biol. Neoplasia 3: 165–175.
Barcellos-Hoff, M.H. and Ravani, S.A. 2000. Irradiated mammary gland stroma promotes the expression of tumorigenic
potential by unirradiated epithelial cells. Cancer Res. 60:
125