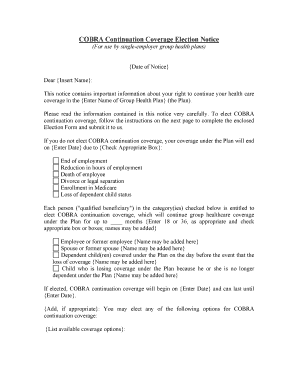
COBRA Continuation Coverage Election Notice
(For use by single-employer group health plans){Date of Notice}
Dear {Insert Name}:
This notice contains important information about your right to continue your health care
coverage in the {Enter Name of Group Health Plan} (the Plan).
Please read the information contained in this notice very carefully. To elect C OBRA
continuation coverage, follow the instructions on the next page to complete the enclose d
Election Form and submit it to us.
If you do not elect COBRA continuation coverage, your coverage under the Plan will end
on {Enter Date} due to {Check Appropriate Box}:
End of employment
Reduction in hours of employment
Death of employee
Divorce or legal separation
Enrollment in Medicare
Loss of dependent child status
Each person ("qualified beneficiary") in the category(ies) checked below is entitled t o
elect COBRA continuation coverage, which will continue group healthcare coverage
under the Plan for up to ____ months {Enter 18 or 36, as appropriate and check
appropriate box or boxes; names may be added}
Employee or former employee {Name may be added here}
Spouse or former spouse {Name may be added here}
Dependent child(ren) covered under the Plan on the day before the event that the
loss of coverage {Name may be added here}
Child who is losing coverage under the Plan because he or she is no longer
dependent under the Plan {Name may be added here}
If elected, COBRA continuation coverage will begin on {Enter Date} and can last until
{Enter Date}.
{Add, if appropriate}: You may elect any of the following options for COBRA
continuation coverage:
{List available coverage options}:
COBRA continuation coverage will cost: {Enter amount each qualified beneficiary will
be required to pay for each option per month of coverage and any other permitted
coverage periods}. You do not have to send any payment with the Election Form.
Important additional information about payment for COBRA continuation coverage is
included in the pages following the Election Form.
If you have any questions about this notice or your rights to COBRA continuation
coverage, you should contact {Enter name of party responsible for COBRA
administration for the Plan, with telephone number and address}.
COBRA Continuation Coverage Election Form
Instructions: To elect COBRA continuation coverage, complete this Election Form and
return it to us. Under federal law, you must have 60 days after the date of this notice to
decide whether you want to elect COBRA continuation coverage under the Plan.
Send completed Election Form to:{Enter name and address}.
This Election Form must be completed and returned by mail {or describe other means of
submission and due date}. If mailed, it must be post-marked no later than {Enter date}.
If you do not submit a completed Election Form by the due date shown above, you will
lose your right to elect COBRA continuation coverage. If you reject COBRA
continuation coverage before the due date, you may change your mind as long as you
furnish a completed Election Form before the due date. However, if you change your
mind after first rejecting COBRA continuation coverage, your COBRA continuation
coverage will begin on the date you furnish the competed Election Form.
Read the important information about your rights included in the pages after the Elec tion
Form.
I (We) elect COBRA continuation coverage in [enter name of plan] (the Plan) as
indicated below:
I (We) elect to continue our coverage in the [enter name of plan] (the Plan) as indicated
below:
Name:
Date of Birth:
Relationship to Employee:
SSN (or other identifier):
Coverage option elected:
[Add if appropriate]
Name:
Date of Birth:
Relationship to Employee:
SSN (or other identifier):
Coverage option elected:
[Add if appropriate]
Name:
Date of Birth:
Relationship to Employee:
SSN (or other identifier):
Coverage option elected:
[Add if appropriate]
Name:
Date of Birth:
Relationship to Employee:
SSN (or other identifier):
Coverage option elected:
[Add if appropriate]
Name:
Date of Birth:
Relationship to Employee:
SSN (or other identifier):
Coverage option elected:
[Add if appropriate]
Signature: ____________________________________________________________________
Print Name:
Relationship to individual(s) listed above:
Print Address:
Telephone Number:
Important Information About Your COBRA Continuation Coverage Rights
What Is Continuation Coverage?
Federal law requires that most group health plans (including this Plan) give employees
and their families the opportunity to continue their healthcare coverage when there is a
"qualifying event" that would result in a loss of coverage under an employer's plan.
Depending on the type of qualifying event, "qualified beneficiaries" can include the
employee (or retired employee) covered under the group health plan, the covered
employee's spouse, and dependent children of the covered employee.
Continuation coverage is the same coverage that the Plan gives to other participants or
beneficiaries under the Plan who are not receiving continuation coverage. Each qualified
beneficiary who elects continuation coverage will have the same rights under the Plan as
other participants or beneficiaries covered under the Plan, including {Add if applicable:
open enrollment and} special enrollment rights.
How Long Will Continuation Coverage Last?
In the case of a loss of coverage due to end of employment or reduction in hours of
employment, coverage generally may be continued only for up to a total of 18 months. In
the case of losses of coverage due to an employee's death, divorce or legal separation, the
employee's becoming entitled to Medicare benefits, or a dependent child ceasing to be a
dependent under the terms of the Plan, coverage may be continued for up to a total of 36
months. When the qualifying event is the end of employment or reduction of the
employee's hours of employment, and the employee became entitled to Medicare benefits
less than 18 months before the qualifying event, COBRA continuation coverage for
qualified beneficiaries other than the employee lasts until 36 months after the date of
Medicare entitlement. This notice shows the maximum period of continuation coverage
available to the qualified beneficiaries.
Continuation coverage will be terminated before the end of the maximum period if:Any required premium is not paid on time;
A qualified beneficiary becomes covered, after electing continuation coverage,
under another group health plan that does not impose any pre-existing condition
exclusion for a preexisting condition of the qualified beneficiary;
A qualified beneficiary becomes entitled to Medicare benefits (under Part A, Part
B, or both) after electing continuation coverage; or
The employer ceases to provide any group health plan for its employees.
Continuation coverage may also be terminated for any reason the Plan would terminate
coverage of a participant or beneficiary not receiving continuation coverage (such as
fraud).
[If the maximum period shown on page 1 of this notice is less than 36 months, add the
following three paragraphs.]
How Can You Extend the Length of Continuation Coverage?
If you elect continuation coverage, an extension of the maximum period may be available
if a qualified beneficiary is disabled or a second qualifying event occurs. You must notify
{Enter name of party responsible for COBRA administration} of a disability or a second
qualifying event in order to extend the period of continuation coverage. Failure to provide
notice of a disability or second qualifying event may affect the right to extend the period
of continuation coverage.
Disability
An 11-month extension of coverage may be available if any of the qualified beneficiaries
is determined by the Social Security Administration (SSA) to be disabled. The disability
has to have started at some time before the 60th day of COBRA continuation coverage
and must last at least until the end of the 18-month period of continuation coverage.
{Describe Plan provisions for requiring notice of disability determination, inlcuding time
frames and procedures}. Each qualified beneficiary who has elected continuation
coverage will be entitled to the 11-month disability extension if one of them qualifies. If
the qualified beneficiary is determined by SSA to no longer be disabled, you must notify
the Plan of that fact within 30 days after SSA's determination.
Second Qualifying Event
An 18-month extension of coverage will be available to spouses and dependent children
who elect continuation coverage if a second qualifying event occurs during the first 18
months of continuation coverage. The maximum amount of continuation coverage
available when a second qualifying event occurs is 36 months. Such second qualifying
events include the death of a covered employee, divorce or separation from the covered
employee, the covered employee's becoming entitled to Medicare benefits (under Part A,
Part B, or both), or a dependent child's ceasing to be eligible for coverage as a dependent
under the Plan. These events can be a second qualifying event only if they would have
caused the qualified beneficiary to lose coverage under the Plan if the first qualifying
event had not occurred. You must notify the Plan within 60 days after a second qualifying
event occurs if you want to extend your continuation coverage.
How Can You Elect Continuation Coverage?
To elect continuation coverage, you must complete the Election Form and furnish it
according to the directions on the form. Each qualified beneficiary has a separate right to
elect continuation coverage. For example, the employee's spouse may elect continuation
coverage even if the employee does not. Continuation coverage may be elected for only
one, several, or for all dependent children who are qualified beneficiaries. A parent may
elect to continue coverage on behalf of any dependent children. The employee or the
employee's spouse can elect continuation coverage on behalf of all of the qualified
beneficiaries.
In considering whether to elect continuation coverage, you should take into account that a
failure to continue your group health coverage will affect your future rights under federal
law. First, you can lose the right to avoid having preexisting condition exclusions applied
to you by other group health plans if you have more than a 63-day gap in health coverage,
and election of continuation coverage may help you not have such a gap. Second, you
will lose the guaranteed right to purchase individual health insurance policies that do not
impose such pre-existing condition exclusions if you do not get continuation coverage for
the maximum time available to you. Finally, you should take into account that you have
special enrollment rights under federal law. You have the right to request special
enrollment in another group health plan for which you are otherwise eligible (such as a
plan sponsored by your spouse's employer) within 30 days after your group health
coverage ends because of the qualifying event listed above. You will also have the same
special enrollment right at the end of continuation coverage if you get continuation
coverage for the maximum time available to you.
How Much Does COBRA Continuation Coverage Cost?
Generally, each qualified beneficiary may be required to pay the entire cost of
continuation coverage. The amount a qualified beneficiary may be required to pay may
not exceed 102 percent (or, in the case of an extension of continuation coverage. due to a
disability, 150 percent) of the cost to the group health plan (including both employer and
employee contributions) for coverage of a similarly situated plan participant or
beneficiary who is not receiving continuation coverage. The required payment for each
continuation coverage period for each option is described in this notice.
{If employees might be eligible for trade adjustment assistance, the following
information may be added}: The Trade Act of 2002 created a new tax credit for certain
individuals who become eligible for trade adjustment assistance and for certain retired
employees who are receiving pension payments from the Pension Benefit Guaranty
Corporation (PBGC) (eligible individuals). Under the new tax provisions, eligible
individuals can either take a tax credit or get advance payment of 65 percent of premiums
paid for qualified health insurance, including continuation coverage. If you have
questions about these new tax provisions, you may call the Health Care Tax Credit
Customer Contact Center toll-free at 866-628-4282. TTD/TTY callers may call toll-free
at 866-626-4282. Further information about the Trade Act is also available at:
http:// www.doleta.gov/tradeact/2002act_index.cfm.
When and How Must Payment for COBRA Continuation Coverage be Made?
First payment for continuation coverage. If you elect continuation coverage, you do
not have to send any payment with the Election Form. However, you must make your
first payment for continuation coverage no later than 45 days after the date of your
election. (This is the date the Election Notice is post-marked, if mailed.) If you do not
make your first payment for continuation coverage in full no later than 45 days after the
date of your election, you will lose all continuation coverage rights under the Plan. You
are responsible for making sure that the amount of your first payment is correct. You may
contact {Enter appropriate contact information for the party responsible for COBRA
administration under the Plan} to confirm the correct amount of your first payment.
Periodic payments for continuation coverage. After you make your first payment for
continuation coverage, you will be required to pay for continuation coverage for each
subsequent coverage period. The amount due for each coverage period for each qualified
beneficiary is shown in this notice. The periodic payments can be made on a monthly
basis. Under the Plan, each of these periodic payments for continuation coverage is due
on the {Enter due date for each monthly payment}for that coverage period. [If Plan offers
other payment schedules, enter the following with appropriate dates: You may instead
make payments for continuation coverage for the following coverage periods, due on the
following dates.] If you make a periodic payment on or before the first day of the
coverage period to which it applies, your coverage under the Plan will continue for that
coverage period without any break. The Plan [will or will not] send periodic notices of
payments due for these coverage periods.
Grace periods for periodic payments . Although periodic payments are due on the dates
shown above, you will be given a grace period of 30 days [or enter longer period
permitted by Plan] to make each periodic payment. Your continuation coverage will be
provided for each coverage period as long as payment for that coverage period is made
before the end of the grace period for that payment . [If Plan suspends coverage during
grace period for nonpayment, enter and modify as necessary: However, if you pay a
periodic payment later than the first day of the coverage period for which it applies, but
before the end of the grace period for the coverage period, your coverage under the Plan
will be suspended as of the first day of the coverage period and then retroactively
reinstated (going back to the first day of the coverage period) when the periodic payment
is received. This means that any claim you submit for benefits while your coverage is
suspended may be denied and may have to be resubmitted once your coverage is
reinstated.]
If you fail to make a periodic payment before the end of the grace period for that
coverage period, you will lose all rights to continuation coverage under the Plan.
Your first payment and all periodic payments for continuation coverage should be sent to:
{Enter Appropriate Payment Address}
For More Information
This notice does not fully describe continuation coverage or other rights under the Plan.
More information about continuation coverage and your rights under the Plan is available
in your summary plan description or from the Plan Administrator.
If you have questions concerning the information in this notice, your rights to coverage,
or if you want a copy of your summary plan description, you should contact [enter name
of party responsible for COBRA administration for the Plan, with telephone number and
address].
For more information about your rights under ERISA, including COBRA, the Health
Insurance Portability and Accountability Act (HIPAA), and other laws affecting group
health plans, contact the U.S. Department of Labor's Employee Benefits Security
Administration (EBSA) in your area or visit the EBSA website at
http://www.dol.gov/ebsa. (Addresses and phone numbers of regional and district EBSA
offices are available through EBSA's website.
Keep your plan informed of address changes
In order to protect your family's rights, you should keep the Plan Administrator informed
of any changes in your address and the addresses of family members. You should also
keep a copy, for your records, of any notices you send to the Plan Administrator.
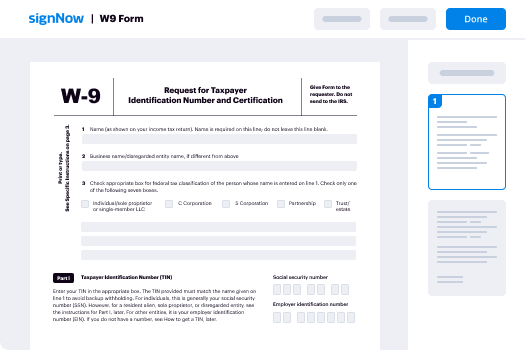
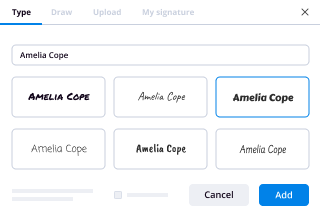
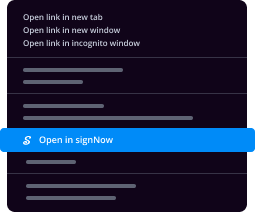
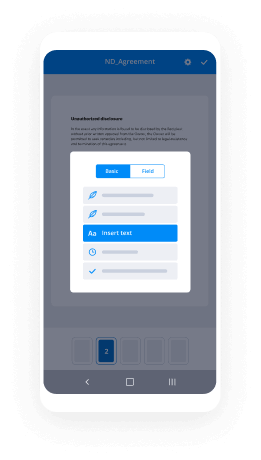
Convenient instructions for setting up your ‘Pension And Employee Benefits Erisa Law And Regulations Related ’ online
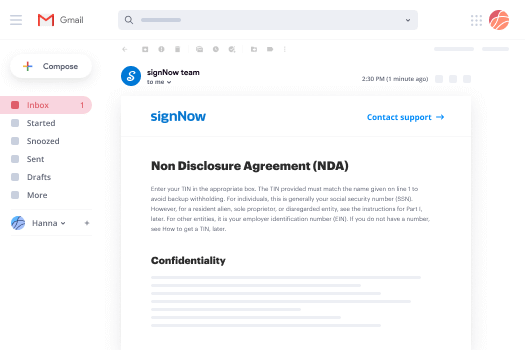
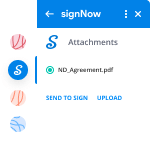
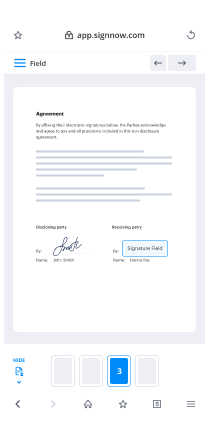
Are you fed up with the burden of handling paperwork? Look no further than airSlate SignNow, the leading digital signature platform for individuals and organizations. Bid farewell to the tedious task of printing and scanning documents. With airSlate SignNow, you can effortlessly complete and sign documents online. Take advantage of the extensive features embedded in this user-friendly and cost-effective platform and transform your method of document handling. Whether you need to approve forms or gather digital signatures, airSlate SignNow simplifies the process, needing just a few clicks.
Follow this step-by-step guide:
- Sign in to your account or initiate a free trial with our service.
- Click +Create to upload a file from your device, cloud, or our form repository.
- Open your ‘Pension And Employee Benefits Erisa Law And Regulations Related ’ in the editor.
- Click Me (Fill Out Now) to get the form ready on your end.
- Add and assign fillable fields for others (if needed).
- Proceed with the Send Invite settings to request electronic signatures from others.
- Download, print your copy, or convert it into a reusable template.
No need to worry if you have to collaborate with your team on your Pension And Employee Benefits Erisa Law And Regulations Related or send it for notarization—our platform provides you with all you need to complete such tasks. Register with airSlate SignNow today and elevate your document management to a higher level!