Certificates of Creditable Coverage Services
(HIPAA - Health Insurance Portability and Accountability Act of 1996)
__________________________________________________________________________________________________________________
Services
Sample: Certificate of Group Health Plan Coverage
Sample: State Mandated Certificate Notice Requirements
07/01/2005
Visit our Website at http://mutualofomaha.com
1
�Certificates of Creditable Coverage Services
(Applicable to Medical Coverage(s) only)
These guidelines are being provided as information only and are not intended to be all-inclusive or to serve as
legal advice. In addition, the requirements described in this manual may change. Employers should consult
their own attorneys and advisors to determine their responsibilities under HIPAA Federal and State laws.
A general outline of services provided by Mutual of Omaha for Certificates of Creditable Coverage Services is
shown on the following pages. This outline is not intended to be definite or all-inclusive. The responsibilities of
both parties will be finalized in a written document signed by each party.
Mutual of Omaha Companies' Responsibilities
1.
Will maintain the specific rostering criteria provided by the employer/plan administrator to furnish the
certificates of creditable coverage.
Rostering Criteria: All insured employees and dependents informational data must be provided by the
employer/plan administrator for the initial and on-going enrollment of their plan.
2.
Will furnish certificates of creditable coverage to individuals who lose coverage under the plan, or an entity
requesting the certificate on behalf of such an individual, in accordance with HIPAA and in addition to
furnishing additional certificates of creditable coverage:
a)
during a 24-month period after coverage ceases, a certificate will be provided, at no additional charge, if
requested by or on behalf of the individual (whether the individual is a participant's spouse, or any other
dependent). The number of requests permitted during this period is unlimited.
b) on behalf of an individual who elected COBRA continuation.
c) at the time the individual’s COBRA continuation ends (for whatever reason), provided that you purchased
our COBRA Billing and Collection Services.
Will furnish certificates of creditable coverage with the state mandated notice requirement (i.e. AZ, MTRefer to notice samples in this section).
3.
Will charge the required monthly service fee that is payable and due on the day that your premium payment is
due.
4.
Will maintain a record of individuals to whom we have furnished certificates of creditable coverage. (A
summary report listing the participants who received certificates will not be furnished to the employer. If you
are interested in a specific participant, we can provide you with this information.)
5.
Will adhere to Mutual of Omaha’s guidelines regarding "confidentiality" before considering the release of any
information provided on the creditable coverage certificate.
07/01/2005
Visit our Website at http://mutualofomaha.com
2
�Employer/Plan Sponsors' Responsibilities
1.
Will provide to Mutual of Omaha Companies specific rostering criteria, in a format mutually agreed upon, for
the purpose to furnish certificates of creditable coverage.
a)
b)
c)
d)
Names of covered employees;
Addresses (including street address, city, state and zip code) of covered employees;
Names of covered dependents;
Addresses (including street address, city, state and zip code) of covered dependents, if different from
covered employee's address;
e) Covered dependents' dates of birth;
f) Covered dependents' relationship to covered employee;
g) Covered dependents' marital status;
h) Effective date of coverage for covered employees and dependents.
This rostering criteria must be submitted to us for the initial and on-going enrollment of your plan.
2.
Will provide notification within 72 hours after an employee and/or dependent's coverage under the plan
(including any plan through a health maintenance organization or other company affiliated with us) ceases
except for cessation of COBRA continuation coverage, or after receipt of a request from us or an individual
who has lost coverage under the plan, your organization shall provide us with the following information:
a)
b)
c)
d)
e)
f)
g)
h)
Name and address of the covered employee/dependent whose coverage terminated;
Identification number of covered employee;
Name of any dependents to whom the certificate of creditable coverage applies;
Date waiting period or affiliation period (if any) began;
Date coverage began;
Date coverage ended (or advise if coverage is continuing as of the date information is provided);
Address of dependents if different from employee's address; and
Information to furnish certificates of creditable coverage in accordance with the requirements of HIPAA.
3.
Will provide the information described in 2. above by registered or certified mail or by facsimile, addressed as
set forth below (or at such other address as may be provided by us):
Mutual of Omaha Insurance Company
Mutual of Omaha Plaza
Omaha, Nebraska 68175
Attention: S4 - Group Premium and Enrollment Services - HIPAA
Facsimile: (402) 997-1995
4.
Will remit to us any required fees for service. This fee shall be due and payable on the day that your premium
payment is due, if applicable.
5.
In the event the Certificates of Creditable Coverage Service agreement terminates, your organization remains
responsible for providing certificates of creditable coverage in accordance with HIPAA. The service agreement
will terminate upon the earliest of:
a) with respect to your group health plan insured by our company, the date on which such group health plan
terminates; and with respect to a group health plan you may have through a health maintenance
organization or other company affiliated with us, the date on which such group health plan terminates; or
b) the date we advise you that this agreement is terminated due to your failure to comply with your
obligations; or
c) at any time by either party upon 30 days' advance written notice to the other party.
07/01/2005
Visit our Website at http://mutualofomaha.com
3
�Certificate of Group Health Plan Coverage – Sample
(Mutual of Omaha’s Certificate Sample)
CERTIFICATE OF GROUP HEALTH PLAN COVERAGE
IMPORTANT – KEEP THIS CERTIFICATE. This certificate is evidence of your coverage under this plan.
Under a federal law knows as HIPAA, you may need evidence of your coverage to reduce a preexisting condition.
exclusion period under another plan, to help you get special enrollment in another plan, or to get certain types of
individual health coverage even if you have health problems.
S
[FORMER EMPLOYEE/DEPENDENT’S NAME]
[ADDRESS LINE ONE]
[ADDRESS LINE TWO]
[CITY, STATE, ZIP]
A
1. Date of this certificate: _____________________
2. Name of group health plan: _____________________
3. Name of participant:
Plan Number: _____________________
A. Last: _____________________ First: _____________________
M
MI: _____
4. Name of any dependents to whom this certificate applies:
Last
First
MI
B.
___________________________
________________
_____
C.
___________________________
________________
_____
D.
___________________________
________________
_____
E.
___________________________
________________
_____
F.
___________________________
________________
_____
G.
___________________________
________________
_____
P
L
5. Name and address of plan administrator or issuer responsible for providing this certificate:
Mutual of Omaha
Mutual of Omaha Plaza
Omaha, NE 68175
E
6. For further information, call: (800) 365-1181
7. If the individual(s) identified in line 3 and line 4 has at least 18 months of creditable coverage (disregarding
periods of coverage before a 63-day break), check here ______ and skip lines 8 and 9.
8. Date waiting period or affiliation period (if any) began: _________
9. Date coverage began:
A. _____________________
B. _____________________
C. _____________________
D. _____________________
E. _____________________
F. _____________________
G. _____________________
07/01/2005
10. Date coverage ended:
A. _____________________
B. _____________________
C. _____________________
D. _____________________
E. _____________________
F. _____________________
G. _____________________
OR
Coverage is continuing as
of the date of this certificate:
A. _____________________
B. _____________________
C. _____________________
D. _____________________
E. _____________________
F. _____________________
G. _____________________
Visit our Website at http://mutualofomaha.com
4
�STATEMENT OF HIPAA PORTABILITY RIGHTS
IMPORTANT – KEEP THIS CERTIFICATE
Preexisting condition exclusions. Some group health plans restrict coverage for medical conditions present before an individual’s enrollment.
These restrictions are known as “preexisting condition exclusions.” A preexisting condition exclusion can apply only to conditions for which
medical advice, diagnosis, care, or treatment was recommended or received within 6 months before your “enrollment date.” Your enrollment
date is your first day of coverage under the plan, or, if there is a waiting period, the first day of your waiting period (typically, your first day of
work). In addition, a preexisting condition exclusion cannot last for more than 12 months after your enrollment date (18 months if you are a late
enrollee). Finally, a preexisting condition exclusion cannot apply to pregnancy and cannot apply to a child who is enrolled in health coverage
within 30 days after birth, adoption or placement for adoption.
If a plan imposes a preexisting condition exclusion, the length of the exclusion must be reduced by the amount of your prior creditable coverage.
Most health coverage is creditable coverage, including group health plan coverage, COBRA continuation coverage, coverage under an individual
health policy, Medicare, Medicaid, State Children’s Health Insurance Program (SCHIP), and coverage through high-risk pools and the Peace
Corps. Not all forms of creditable coverage are required to provide certificates like this one. If you do not receive a certificate for past coverage,
talk to your new plan administrator.
S
You can add up any creditable coverage you have, including the coverage shown on this certificate. However, if at any time you went for 63 days
or more without any coverage (called a break in coverage) a plan may not have to count the coverage you had before the break.
¾
A
Therefore, once your coverage ends, you should try to obtain alternative coverage as soon as possible to avoid a 63-day break. You
may use this certificate as evidence of your creditable coverage to reduce the length of any preexisting condition exclusion if you
enroll in another plan.
M
Right to get special enrollment in another plan. Under HIPAA, if you lose your group health plan coverage, you may be able to get into
another group health plan for which you are eligible (such as a spouse’s plan), even if the plan generally does not accept late enrollees, if you
request enrollment within 30 days. (Additional special enrollment rights are triggered by marriage, birth, adoption, and placement for adoption.)
¾
Therefore, once your coverage ends, if you are eligible for coverage in another plan (such as a spouse’s plan), you should request
special enrollment as soon as possible.
P
Prohibition against discrimination based on a health factor. Under HIPAA, a group health plan may not keep you (or your dependents) out of
the plan based on anything related to your health. Also, a group health plan may not charge you (or your dependents) more for coverage, based
on health, than the amount charged a similarly situated individual.
Right to individual health coverage. Under HIPAA, if you are an “eligible individual,” you have a right to buy certain individual health
policies (or in some states, to buy coverage through a high-risk pool) without a preexisting condition exclusion. To be an eligible individual, you
must meet the following requirements:
•
•
•
•
•
L
You have had coverage for at least 18 months without a break in coverage of 63 days or more;
Your most recent coverage was under a group health plan (which can be shown by this certificate);
Your group coverage was not terminated because of fraud or nonpayment of premiums;
You are not eligible for COBRA continuation coverage or you have exhausted your COBRA benefits (or continuation coverage under a
similar state provision); and
You are not eligible for another group health plan, Medicare, or Medicaid, and do not have any other health insurance coverage.
The right to buy individual coverage is the same whether you are laid off, fired, or quit your job.
¾
E
Therefore, if you are interested in obtaining individual coverage and you meet the other criteria to be an eligible individual, you
should apply for this coverage as soon as possible to avoid losing your eligible individual status due to a 63-day break.
Special Information for people on FMLA leave. If you are taking leave under the Family and Medical Leave Act (FMLA) and you drop health
coverage during your leave, any days without health coverage while on FMLA leave will not count towards a 63-day break in coverage. In
addition, if you do not return from leave, the 30-day period to request special enrollment in another plan will not start before your FMLA leave
ends.
¾ Therefore, when you apply for other health coverage, you should tell your plan administrator or health insurer about any prior
FMLA leave.
State flexibility. This certificate describes minimum HIPAA protections under federal law. States may require insurers and HMOs to provide
additional protections to individuals in that state.
For more information. If you have questions about your HIPAA rights, you may contact your state insurance department or the U.S.
Department of Labor, Employee Benefits Security Administration (EBSA) toll-free at 1-866-444-3272 (for free HIPAA publications ask for
publications concerning changes in health care laws). You may also contact CMS publication hotline at 1-800-633-4227 (ask for “Protecting
Your Health Insurance Coverage”). These publications and other useful information are also available on the Internet at:
http://www.dol.gov/ebsa, the DOL’s interactive web pages – Health Elaws, or http://www.cms.hhs.gov/hipaa1.
07/01/2005
Visit our Website at http://mutualofomaha.com
5
�The Health Insurance Portability and Accountability Act of 1996 (HIPAA) requires all Group Health
Plans and Insurance Companies to provide the enclosed certificate of creditable coverage and Statement
of HIPAA Portability Rights when you lose your coverage under a group health plan. In order to assist
you in understanding the enclosed certificate, we are providing you with answers to some commonly
asked questions:
Q. What is the purpose of receiving this certificate?
S
A. This certificate provides evidence of your prior health coverage (or creditable coverage), in addition to
your portability rights under HIPAA. This certificate may reduce any preexisting condition exclusion period
imposed by your new health plan. When you enroll in a new health plan that applies a preexisting condition
exclusion period you will need to provide this certificate at the time of enrollment. You should ensure this
information is correct.
A
Q. Why does the certificate show only one plan number when I also had coverage under your alternative
health plan before changing coverage to the current plan number shown?
M
A. We will only show the most current plan number you were covered under prior to your termination or loss
of coverage.
P
Q. Why does the certificate not include my dependent(s)’ names?
A. If the health plan did not provide us with specific dependent information, we have indicated “family”
coverage on the certificate.
Q. Why does the certificate not include my identification number?
L
E
A. As the result of state legislation impacting the display of social security number (commonly used for
insurance identification purposes), we have removed the identification number to safeguard the identity of our
customers.
Q. Who do I call if I have questions regarding the information provided or need to request another
certificate?
A. Call the phone number provided on the certificate for assistance.
Q. Why does the "date coverage began" not reflect the actual effective date insurance began under the plan
for my dependent(s) &/or myself?
A. This Certificate is only required to show at least 18 months of creditable coverage. However, if you have at
least 18 months of continuous coverage (disregarding periods of coverage before a 63 day break) the date
coverage began may only reflect two years of coverage or less. Otherwise, this Certificate will reflect the
actual date coverage began.
07/01/2005
Visit our Website at http://mutualofomaha.com
6
�State Mandated Certificate Notice Requirements and Samples
The State mandates are being provided as information only and are not intended to be all-inclusive or to
serve as legal advice. In addition, the requirements described in this manual may change. Employers should
consult their own attorneys and advisors to determine their responsibilities under HIPAA federal and state
laws.
The following states have mandated additional requirements that are to be included on the certificates of creditable
coverage.
Arizona Certificate Notice – Sample (The notice must be at least 14pt type)
Important Notice!
Keep this Certificate with your important personal records to protect your rights
under the Health Insurance Portability and Accountability Act of 1996 ("HIPAA").
This Certificate is proof of your prior health insurance coverage. You may need to
show this Certificate to have a guaranteed right to buy new health insurance
("Guaranteed Issue"). This Certificate may also help you avoid waiting periods or
exclusions for preexisting conditions. Under HIPAA, these rights are guaranteed
only for a very short time period. After your group coverage ends, you must apply
for new coverage within 63 days to be protected by HIPAA. If you have questions,
call the Arizona Department of Insurance.
The Consumer Assistance telephone number for the Department is 602-912-8444
or 1-800-325-2548.
Montana Certificate Notice – Sample
Notice To Montana Residents
You may have the option to apply to the Montana Comprehensive Health Care Association for an association
portability plan by contacting the Association within 63 days of termination of creditable coverage. The telephone
number and address of the Association is:
Montana Comprehensive Health Association
c/o Blue Cross and Blue Shield of Montana
404 Fuller Avenue
P .O. Box 4309
Helena, MT 59604
1-800-447-7828, extension 8537
COBRA continuation coverage may be available to you. Please refer to your group health plan to determine whether
COBRA continuation coverage is available to you or call the phone number provided in item 7. on page 1 of the
Certificate for more information.
You may be entitled to convert to an individual health insurance policy. Please refer to your group health plan to
determine whether conversion rights are available to you or call 1-800-826-8054 for more information.
conversion rights are available to you or call 1-800-826-8054 for more information.
07/01/2005
Visit our Website at http://mutualofomaha.com
7
�
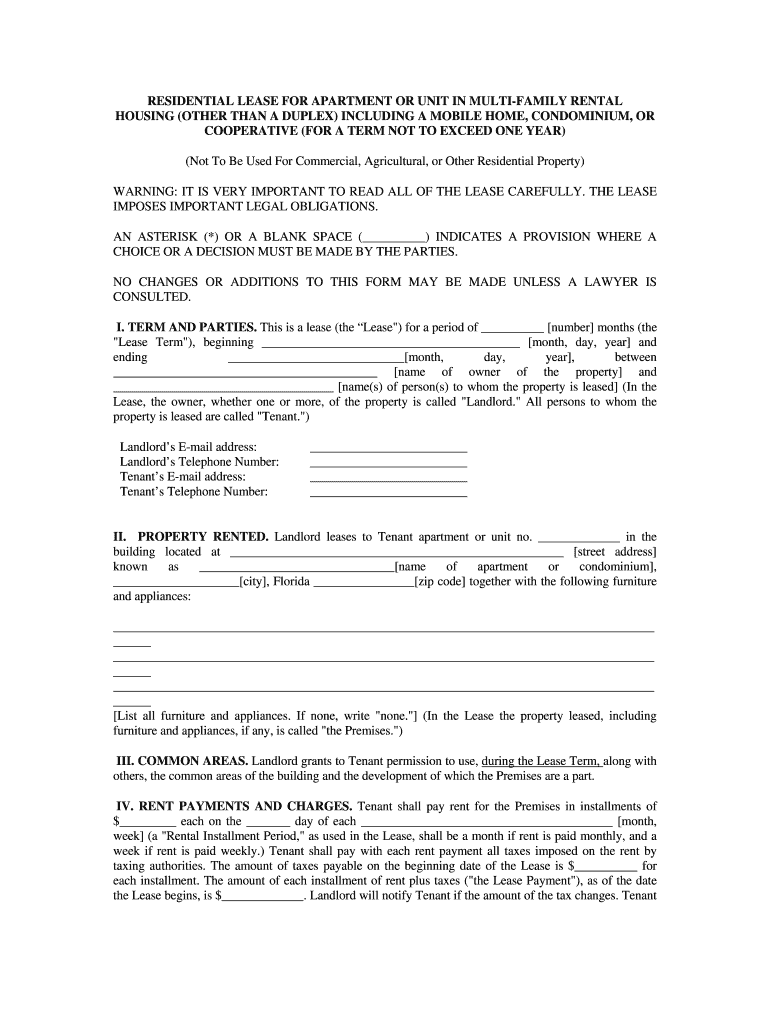
Valuable advice on finalizing your ‘Residential Lease Rental Form’ digitally
Are you fed up with the inconvenience of managing paperwork? Look no further than airSlate SignNow, the premier eSignature solution for both individuals and businesses. Bid farewell to the tedious task of printing and scanning documents. With airSlate SignNow, you can seamlessly complete and sign documents online. Utilize the powerful features integrated into this intuitive and affordable platform and transform your method of document administration. Whether you need to sign forms or gather electronic signatures, airSlate SignNow takes care of everything effortlessly, with just a few clicks.
Adhere to these comprehensive steps:
- Access your account or register for a complimentary trial with our service.
- Select +Create to upload a document from your device, cloud storage, or our form repository.
- Open your ‘Residential Lease Rental Form’ in the editor.
- Click Me (Fill Out Now) to set up the document on your end.
- Add and designate fillable fields for other participants (if necessary).
- Proceed with the Send Invite settings to solicit eSignatures from others.
- Download, print your version, or convert it into a reusable template.
No need to worry if you have to collaborate with your peers on your Residential Lease Rental Form or send it for notarization—our platform provides all the tools you need to accomplish these tasks. Sign up with airSlate SignNow today and take your document management to the next level!