Streamline Your Sickness Billing Format for Client for Teams with airSlate SignNow
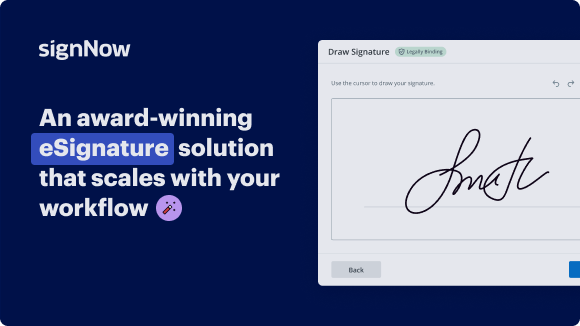
See airSlate SignNow eSignatures in action
Choose a better solution
Move your business forward with the airSlate SignNow eSignature solution
Add your legally binding signature
Integrate via API
Send conditional documents
Share documents via an invite link
Save time with reusable templates
Improve team collaboration
Our user reviews speak for themselves






airSlate SignNow solutions for better efficiency
Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.

Sickness billing format for client for teams
In today's fast-paced business environment, managing client documentation effectively is essential for maintaining professionalism and operational efficiency. The sickness billing format for client for teams can be seamlessly executed using airSlate SignNow, a platform that simplifies document workflows while enhancing collaboration among team members.
Using sickness billing format for client for teams with airSlate SignNow
- Access the airSlate SignNow platform by entering its web address in your preferred browser.
- Create a free trial account or log in to your existing account.
- Select the document you need to sign, or initiate the upload process for new files.
- If you anticipate using this document repeatedly, consider converting it into a reusable template.
- Open the uploaded file to make necessary adjustments, such as adding fillable fields or inserting text where needed.
- Affix your signature to the document and designate where others need to sign.
- Click 'Continue' to finalize your document setup and dispatch an electronic signature request.
With airSlate SignNow, businesses benefit from a rich feature set that maximizes return on investment, with no hidden costs and a straightforward pricing structure. Its user-friendly design ensures that even small to mid-sized businesses can efficiently scale using the platform.
Moreover, users enjoy dependable 24/7 support with all paid plans, ensuring assistance whenever necessary. Experience the difference today by trying airSlate SignNow and streamline your document management process!
How it works
Get legally-binding signatures now!
FAQs
-
What is a sickness billing format for client for teams?
A sickness billing format for client for teams is a structured template designed to document and manage billing processes related to employee sick leave. It ensures accurate invoicing and record-keeping, which is crucial for maintaining financial and operational integrity within teams. -
How can airSlate SignNow help with sickness billing format for client for teams?
airSlate SignNow offers an intuitive platform that allows teams to create, send, and eSign documents using a sickness billing format for client for teams. This streamlines the entire billing process, making it easier for teams to collaborate and manage sick leave documentation efficiently. -
Is there a free trial available for airSlate SignNow?
Yes, airSlate SignNow offers a free trial that allows prospective customers to explore its capabilities, including how to utilize a sickness billing format for client for teams. During the trial, users can experience the platform's features without any commitment. -
What are the pricing options for airSlate SignNow?
airSlate SignNow provides various pricing plans tailored to suit the needs of teams, including those looking for a sickness billing format for client for teams. Each plan is designed to offer value based on the size and requirements of the organization, ensuring cost-effective solutions. -
Can I integrate airSlate SignNow with other software for billing purposes?
Absolutely! airSlate SignNow seamlessly integrates with several other applications, enhancing the use of a sickness billing format for client for teams. This interoperability allows teams to synchronize their workflows, improving efficiency and consistency in billing processes. -
What features does airSlate SignNow offer for document management?
airSlate SignNow includes advanced features such as templates, eSigning, document tracking, and automated workflows, which are essential for implementing a sickness billing format for client for teams. These tools simplify document management, making it easier for teams to stay organized. -
How does airSlate SignNow ensure the security of sensitive billing information?
airSlate SignNow prioritizes security by employing advanced encryption and authentication protocols, which protect sensitive information associated with sickness billing format for client for teams. This ensures that all documents are securely managed, safeguarding user data from unauthorized access.
What active users are saying — sickness billing format for client for teams
Get more for sickness billing format for client for teams
- Invoice letter template word for Engineering
- Invoice Letter Template Word for Export
- Invoice letter template word for Shipping
- Invoice Letter Template Word for Public Relations
- Invoice letter template word for Production
- Invoice Letter Template Word for Supervision
- Invoice letter template word for Product quality
- Invoice Letter Template Word for Inventory
Find out other sickness billing format for client for teams
- Easily add signature to PDF without Acrobat for ...
- Discover free methods to sign a PDF document online ...
- How to add electronic signature to PDF on iPhone with ...
- How to sign PDF files electronically on Windows with ...
- How to sign a PDF file on phone with airSlate SignNow
- Experience seamless signing with the iPhone app for ...
- Easily sign PDF without Acrobat for seamless document ...
- Easily email a document with a signature using airSlate ...
- How to sign a document online and email it with ...
- How to use digital signature certificate on PDF ...
- How to use e-signature in Acrobat for effortless ...
- How to use digital signature on MacBook with airSlate ...
- Discover effective methods to sign a PDF online with ...
- Effortlessly sign PDFs with the linux pdf sign command
- Easily sign PDF documents on Windows with airSlate ...
- Easily sign a PDF file and email it back with airSlate ...
- Effortlessly sign PDF documents on phone
- Sign PDF document with certificate effortlessly
- Easily signing a PDF document on my iPhone
- Sign PDF online with electronic signature easily and ...