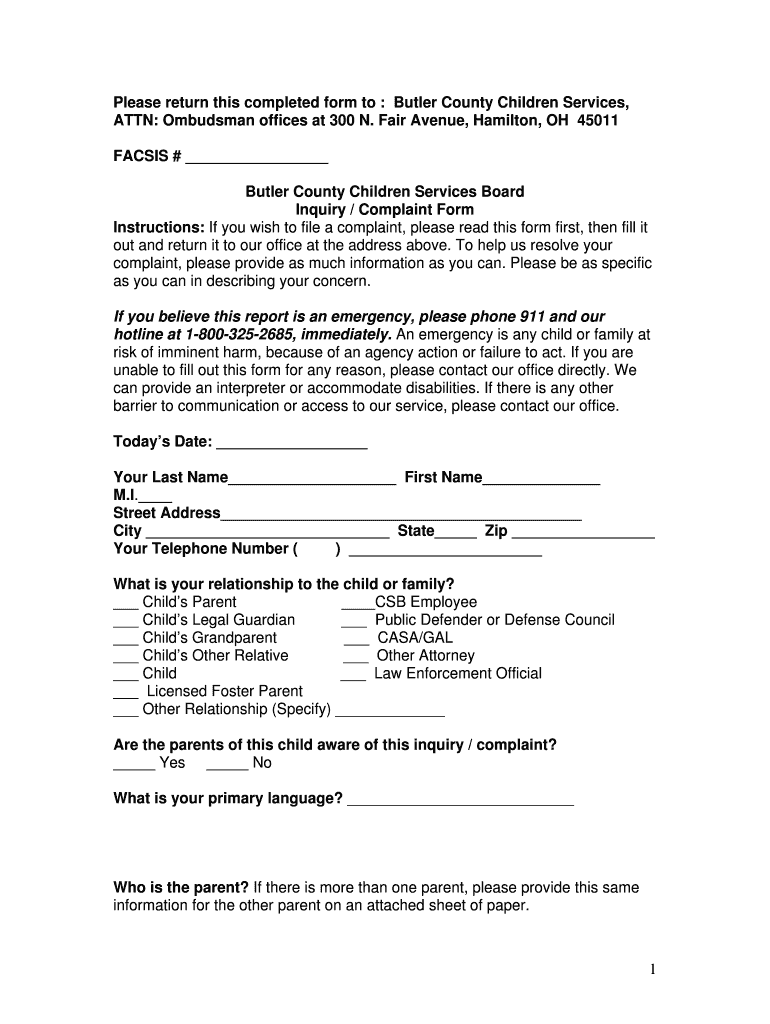
Fill and Sign the 1 Please Return This Completed Form to Butler County Children Butlercountychildrenservices
Practical tips for finalizing your ‘1 Please Return This Completed Form To Butler County Children Butlercountychildrenservices’ online
Are you fed up with the burden of managing paperwork? Look no further than airSlate SignNow, the premier eSignature service for both individuals and organizations. Bid farewell to the tedious process of printing and scanning documents. With airSlate SignNow, you can effortlessly complete and sign paperwork online. Take advantage of the extensive features available in this user-friendly and cost-effective platform and transform your approach to document management. Whether you need to approve forms or collect signatures, airSlate SignNow simplifies everything with just a few clicks.
Follow these step-by-step instructions:
- Sign in to your account or initiate a free trial with our service.
- Click +Create to upload a document from your device, cloud, or our form library.
- Open your ‘1 Please Return This Completed Form To Butler County Children Butlercountychildrenservices’ in the editor.
- Click Me (Fill Out Now) to finish the form on your end.
- Add and designate fillable fields for others (if necessary).
- Proceed with the Send Invite options to request eSignatures from others.
- Save, print your copy, or convert it into a reusable template.
No need to worry if you need to collaborate with your colleagues on your 1 Please Return This Completed Form To Butler County Children Butlercountychildrenservices or send it for notarization—our platform provides everything necessary to accomplish such tasks. Sign up with airSlate SignNow today and take your document management to the next level!
FAQs
-
What is airSlate SignNow and how can it help with document signing?
airSlate SignNow is a powerful eSignature solution that enables users to send and eSign documents seamlessly. By utilizing airSlate SignNow, you can ensure that your documents, including those that require the instruction '1 Please Return This Completed Form To Butler County Children Butlercountychildrenservices,' are processed efficiently and securely.
-
How do I return a completed form to Butler County Children Services using airSlate SignNow?
To return a completed form to Butler County Children Services, simply use airSlate SignNow to eSign your document and then follow the prompts to send it directly to the designated email address. This process ensures that your submission of '1 Please Return This Completed Form To Butler County Children Butlercountychildrenservices' is both quick and secure.
-
What are the pricing options for airSlate SignNow?
airSlate SignNow offers various pricing plans to accommodate different business needs, starting from a free trial to affordable monthly subscriptions. Each plan provides unique features that help streamline your document signing process, including the ability to manage forms like '1 Please Return This Completed Form To Butler County Children Butlercountychildrenservices' effectively.
-
Can I integrate airSlate SignNow with other applications?
Yes, airSlate SignNow supports integration with numerous applications, allowing you to enhance your workflow. You can easily connect it with popular tools to manage your documents, ensuring you can handle requests like '1 Please Return This Completed Form To Butler County Children Butlercountychildrenservices' more efficiently.
-
What security measures does airSlate SignNow provide for document signing?
airSlate SignNow prioritizes security with advanced encryption and authentication protocols to protect your documents. When you send a document that includes '1 Please Return This Completed Form To Butler County Children Butlercountychildrenservices,' you can trust that it is safeguarded against unauthorized access.
-
How does airSlate SignNow improve my document management process?
airSlate SignNow simplifies the document management process by enabling users to create, send, and track documents electronically. This streamlining is essential for managing forms such as '1 Please Return This Completed Form To Butler County Children Butlercountychildrenservices,' ensuring you stay organized and efficient.
-
Is airSlate SignNow user-friendly for beginners?
Absolutely! airSlate SignNow is designed with user experience in mind, making it easy for beginners to navigate. Whether you need to eSign documents or manage submissions like '1 Please Return This Completed Form To Butler County Children Butlercountychildrenservices,' the platform is intuitive and straightforward.
Related searches to 1 please return this completed form to butler county children butlercountychildrenservices
Find out other 1 please return this completed form to butler county children butlercountychildrenservices
- Close deals faster
- Improve productivity
- Delight customers
- Increase revenue
- Save time & money
- Reduce payment cycles

