A Guide to the Program of All-inclusive Care
for Elderly MassHealth Members
Commonwealth of Massachusetts
Executive Office of Health and Human Services
www.mass.gov/masshealth
March 2014
�Contents
MassHealth Program of All-inclusive Care for the Elderly............................................... 3
PACE Enrollment ............................................................................................................................ 3
Determination of MassHealth Eligibility ................................................................................... 3
Enrollment Requirements ........................................................................................................... 3
Enrollment Processing................................................................................................................. 4
Initial Enrollment ........................................................................................................................... 4
Enrollment Confirmations - HIPAA 834 Transactions .......................................................... 5
Submission of Enrollments and Disenrollments ................................................................. 5
Automatic Enrollment Adjustments........................................................................................... 6
MassHealth Enrollment Centers ................................................................................................ 6
Rate Cells .......................................................................................................................................... 6
Status Changes ............................................................................................................................... 7
Demographic Changes................................................................................................................ 7
Disenrollment ................................................................................................................................... 7
Involuntary Disenrollment ........................................................................................................... 8
Admissions and Discharges from Nursing Facilities ........................................................ 8
MassHealth Capitation Payments ............................................................................................. 8
Financial Reconciliation .............................................................................................................. 9
Payment Confirmations-HIPAA 820 Transaction .................................................................. 9
PACE Application Submissions ................................................................................................ 9
New PACE Members ................................................................................................................... 9
Reassessments........................................................................................................................... 10
Management Reports .................................................................................................................. 10
Other Provider Reports ............................................................................................................. 11
Key MassHealth PACE Contacts ............................................................................................. 11
2
�MassHealth Program of All-inclusive Care for the Elderly
PACE is the Program of All-inclusive Care for the Elderly. PACE is a fully
capitated Medicare and Medicaid managed care program authorized under
federal regulation and managed jointly by MassHealth and the Centers for
Medicare & Medicaid Services (CMS). For a MassHealth member to be eligible
to apply for enrollment in the PACE program, the member must be aged 55 or
over, reside in a geographical area served by a PACE provider, and be enrolled
in MassHealth Standard.
PACE Enrollment
PACE organizations are responsible for verifying potential PACE enrollees’
eligibility for MassHealth by checking the Eligibility Verification System. The EVS
User Manual is accessible on the MassHealth Web site at
www.mass.gov/masshealth/newmmis. Click on Read Updated Billing Guides,
Companion Guides, and Other Publications.
PACE organizations are also responsible for checking EVS monthly to ensure
that MassHealth members enrolled in PACE have not lost their MassHealth
eligibility.
Potential PACE enrollees who are not MassHealth members should be referred
to the MassHealth Enrollment Center serving their area for MassHealth eligibility
determination. For more information on enrollment centers, refer to Appendix B
of your MassHealth provider manual at the MassHealth Web site
www.mass.gov/masshealth. Click on MassHealth Regulations and Other
Publications, and then on Provider Library. Now click on MassHealth Provider
Manual Appendices.
Determination of MassHealth Eligibility
For a MassHealth member to be eligible to apply for enrollment in the PACE
program, the MassHealth member must be
�
a Massachusetts resident with a community residence in an approved
PACE service area;
�
55 years of age or older; and
�
enrolled in MassHealth Standard.
Enrollment Requirements
The MassHealth member must choose to enroll in PACE voluntarily and
�
live in the geographic area served by the PACE organization at the time of
3
�enrollment;
�
agree to receive all services from the PACE organization, except in the
case of an emergency or when traveling temporarily out of the service
area; and
�
agree to assist his or her primary care physician or primary care team in
developing an individualized plan of care.
MassHealth members are not eligible to enroll in PACE if they are
�
residents of an intermediate care facility for the developmentally disabled;
�
inpatients in a chronic disease or rehabilitation hospital; or
�
permanent residents of a nursing facility.
Note: A potential PACE enrollee may be receiving services from the Department
of Developmental Services (DDS). Before enrolling the member, the PACE
organization must contact the member’s DDS service coordinator to determine
whether PACE enrollment is appropriate. Call 617-624-7779 for information
about DDS services and PASARR regulations.
Enrollment Processing
The Provider Online Service Center is accessible via the EOHHS Virtual
Gateway. This portal allows the electronic enrollment and disenrollment of
members without the necessity of submitting enrollment forms. However, the
MassHealth PACE enrollment form must be completed by the member or his or
her eligibility representative and retained by the PACE organization.
The PACE organization must keep the original MassHealth PACE enrollment
form or an electronic image on file while the member is an active participant, and
for six years following the member’s disenrollment from PACE. All enrollment
forms are subject to review by MassHealth and CMS at any time.
You must continue to complete the standard HIPAA signature forms and keep
them in the member record so that the PACE organization knows who has the
authority to receive information and to participate in health-care decisions on the
member’s behalf. The PACE enrollment form contains a statement explaining
under what circumstances a family caregiver or other responsible person can act
as the applicant’s eligibility representative making decisions related to voluntary
enrollment in PACE on behalf of the member.
Initial Enrollment
The PACE organization must check the Eligibility Verification System (EVS) to
determine the prospective enrollee’s MassHealth eligibility status, which must be
MassHealth Standard. EVS provides important information about deductibles,
4
�spend downs, and patient-paid amount (PPA).
After confirming the prospective enrollee’s eligibility for MassHealth, the PACE
organization submits the MDS-HC to the MassHealth RN for initial clinical
screening eligibility. The MassHealth RN approves the MDS-HC for PACE
eligibility and MassHealth Operations enrolls the approved applicant into MMIS.
New enrollments must be submitted by 2PM on the last business day of the
month.
Upon receiving confirmation of enrollment into MMIS from the MassHealth RN
the PACE organization may enroll the applicant into PACE.
Note: Prospective PACE members who are nursing-home certifiable in the
community may have access to a 300% income consideration for MassHealth
eligibility. For prospective members already in MassHealth Standard the PACE
organization needs to submit the PACE waiver and PACE contact information to
the Tewksbury MassHealth Enrollment Center (MEC).
Enrollment Confirmations - HIPAA 834 Transactions
Enrollment confirmations are posted daily and are available for download from
the Provider Online Service Center. In addition to the daily enrollment
confirmations, a monthly 834 file is available for download. The monthly 834 file
contains details of all members for which a monthly capitation payment is being
made. For more information on the HIPAA 834 transaction, refer to the 834
Companion Guide available on the MassHealth Web site at
www.mass.gov/masshealth.
Submission of Enrollments and Disenrollments
The PACE organization may process new member enrollments and
disenrollments through the last business day of the month. The PACE
organization must check with the PACE Operations Unit monthly to determine
the cut-off time for processing. The cut-off may vary month to month and is
determined by the MassHealth production schedule.
All effective enrollment dates are the first of the month following enrollment. All
disenrollment dates are the last day of the month in which the disenrollment is
requested.
Retroactive effective enrollment and disenrollment dates are not generally
permitted. However, individual consideration will be given on a case-by-case
basis.
All member enrollment information is considered protected health information
(PHI) under HIPAA. If any member information is faxed, the fax cover sheet must
5
�indicate PHI is included. The PACE organization must call the PACE Operations
Unit in advance whenever PHI is being faxed.
Automatic Enrollment Adjustments
Other state agencies or MassHealth units may change MassHealth member
eligibility or demographic data. As these changes may affect a member’s rate
cell, automatic enrollment adjustments are batch processed through NewMMIS.
NewMMIS verifies and edits enrollment information on a daily and monthly basis.
PACE status and rate cells will be affected on the following conditions:
�
Addition or termination of Medicare Part A, or Part B, or both; and
�
Loss of MassHealth eligibility
These changes to PACE enrollment are reported to the PACE organization via
the HIPAA 834 enrollment confirmation transaction.
MassHealth Enrollment Centers
The MassHealth Enrollment Center locations are listed below. For more
information, refer to Appendix B of your MassHealth provider manual at the
MassHealth Web site www.mass.gov/masshealth. Click on MassHealth
Regulations and Other Publications, and then on Provider Library. Now click on
MassHealth Provider Manual Appendices.
45-47 Spruce Street
Chelsea, MA 02150
Phone: 1-888-665-9993
333 Bridge Street
Springfield, MA 01103
Phone: 1-800-332-5545
21 Spring Street Suite 4
Taunton, MA 02780
Phone: 1-800-242-1340
367 East Street
Tewksbury, MA 01876
Phone: 1-800-408-1253
Rate Cells
PACE members are assigned rate cells according to whether they are dually
eligible for Medicare Part A and MassHealth, or MassHealth only. If PACE
members have only Medicare Part B, they are considered MassHealth only.
6
�Status Changes
Demographic Changes
The PACE organization is responsible for reporting any change of address of the
participant to the MassHealth Enrollment Center.
If members are receiving MassHealth through SSI, they must report the change
in address to the local Social Security Administration office. MassHealth cannot
change SSI member records.
Note: The most common reason MassHealth members lose their eligibility is
unreported address changes, because financial redetermination forms do not
reach the members who have moved and are not completed as required.
Disenrollment
Include a disenrollment reason with all PACE disenrollment requests.
On the disenrollment panel, enter a disenrollment reason from the list below. If
the reason for disenrollment is death of the member, enter the date of death.
•
Moved out of service area
�
Provider network unacceptable
�
Dissatisfied with health care
�
Dissatisfied with appeal decision
�
Death (date of death is required)
�
Transportation problem
�
Difficulty contacting doctor
�
Problem receiving emergency treatment
�
Language barrier
�
Poor access for disabled members
�
Takes too long to get appointment
�
Dissatisfaction with specialty care
�
Health care needs changed
7
��
Did not meet clinical needs requirements
�
Request by PACE
�
Improperly enrolled
�
Fair hearing appeal decision
Involuntary Disenrollment
Involuntary disenrollment requests must be preapproved.
You must present a detailed explanation with all applicable documentation to the
MassHealth PACE Program Manager before entering the disenrollment
transaction. The participant has appeal rights to the Board of Hearing and that
information needs to be a part of the documentation that is sent to participant.
Admissions and Discharges from Nursing Facilities
Whenever a PACE community member is admitted to or discharged from a
nursing facility, the contracted nursing facility must submit the SC-1 form (Status
Change for a Member in a Nursing Facility, Chronic Disease and Rehabilitation
Inpatient Hospital, or Rest Home) to the appropriate MassHealth Enrollment
Center with “PACE Member” clearly indicated on the form.
If the SC-1 form is not clearly indicated as “PACE Member,” the MassHealth
Enrollment Center cannot process the status change.
When the institutional member is discharged from the nursing facility, send the
SC-1 form to the Tewksbury MassHealth Enrollment Center, 367 East Street,
Tewksbury, MA 01876, 1-800-408-1253.
MassHealth Capitation Payments
Monthly capitation payments are prospective.
Monthly Payment Cycle
Payments are sent to PACE organizations on the second Thursday of each month.
Payments are issued for all PACE members active on the first day of the payment
month. Member deductibles (spend downs) or patient-paid amounts (PPA) are
deducted from capitation payments.
Note: The PACE provider is responsible for collecting the deductibles.
The nursing home is responsible for collecting the PPA.
8
�Financial Reconciliation
Capitation payments are reconciled monthly. Retroactive enrollment changes up
to a year from the payment month will be adjusted automatically and included
with the monthly capitation payment.
Payment Confirmations-HIPAA 820 Transaction
Payment confirmations are posted monthly and are available for download from
the Provider Online Service Center in the HIPAA 820 record format.
For more information about the HIPAA 820 transaction, refer to the 820
Companion Guide available at www.mass.gov/masshealth.
PACE Application Submissions
Minimum Data Set – Home Care (MDS-HC) is the comprehensive assessment
and screening tool used for data submission to MassHealth for most services
and programs for elders residing in community settings across the state.
A registered nurse must complete the MDS-HC for PACE. A good resource link
for the specialized MDS-HC manual, updates and information is
www.interRAI.org.
Complete all submissions using MDS-HC via the Web-based electronic version.
Complete the Request for Services (RFS) form with all submissions. Also include
accurate enrollment, discharge, and assessment dates with all submissions to
coincide with other required documentation.
All medical data submitted via MDS is considered current if gathered within 30
days of submission. Determinations are effective for 12 months. The PACE
organization must request a redetermination whenever a significant status
change occurs within 30 days of application.
New PACE Members
A registered nurse from the PACE provider is responsible for the completion of
the initial MDS-HC for a prospective PACE member. A licensed Social Worker
(LSW, LCSW, and LICSW) may complete sections: AA, BB, CC, B, C, E, F, G,
and O. No other licensed or other professional may complete sections of the
MDS-HC.
A physician must sign off in Section R.
Submit the initial MDS-HC, with the RFS, to the MassHealth RN. A formal
approval and authorization notice will be issued by the MassHealth nurse. Keep
9
�this notice in the member’s record. It must be made available to MassHealth or
CMS upon request.
When the initial MDS-HC has been evaluated by the MassHealth RN, the
approval will be entered into MMIS by the MassHealth RN. PACE approval must
be recorded in NewMMIS before a new member enrollment can be submitted.
Reassessments
Annually, one month before the anniversary date of the member’s initial
enrollment, submit an MDS-HC reassessment for the member using the
electronic application located on the MassHealth Web site at
www.mass.gov/masshealth.
Management Reports
Use of the HIPAA 834 and 820 transactions is optional.
NewMMIS generates management reports that are available for download from
the NewMMIS Provider Online Service Center. These reports include enrollment
and payment information that can be used in lieu of the 834 and 820
transactions. The reports are produced monthly at the time the capitation
payments are calculated.
The following is a list of NewMMIS reports.
Monthly New Enrollments
Monthly Disenrollments
Monthly Capitation Payments
Monthly Member Lost Eligibility
Monthly Other Insurance (members with Medicare Hospice or Medicare Advantage)
Daily 834 batch Enrollment Errors (if inbound 834s were submitted)
Monthly Capitation Errors
Quarterly Capitation Payments
Annual Capitation Payments
Capitation Demographics
e-Learning Reports
10
�Other Provider Reports
Monthly Grievance Logs
Monthly Appeal Logs
Key MassHealth PACE Contacts
The Coordinated Care Systems Unit, MassHealth Office of Long Term Supports
and Services, manages the PACE program. The office is located at One
Ashburton Place, 5th Floor, Boston, MA 02108.
PACE Director of Coordinated Care - 617-222-7466
PACE Program Manager - 617-222-7485
PACE Operations Coordinator - 617-222-7518
PACE Clinical Coordinator - 617-222-7425
Toll-free telephone and TTY lines are available for members.
Toll-free telephone number:
1-888-885-0484
TTY number (for people with partial or total hearing loss): 1-888-821-5225
11
�
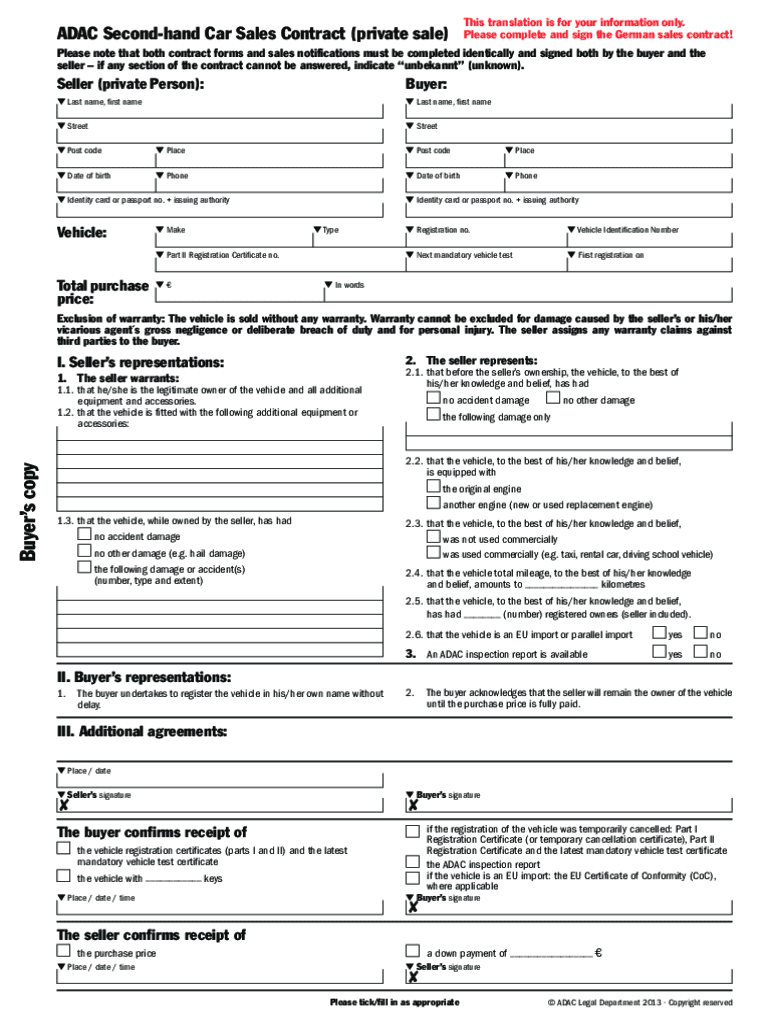
Valuable tips for preparing your ‘Adac Second Hand Car Sales Contract’ online
Are you fed up with the burden of handling paperwork? Look no further than airSlate SignNow, the premier eSignature solution for individuals and small to medium-sized businesses. Bid farewell to the tedious routine of printing and scanning documents. With airSlate SignNow, you can easily complete and sign paperwork online. Utilize the extensive features packed into this user-friendly and cost-effective platform and transform your method of document management. Whether you need to sign forms or collect eSignatures, airSlate SignNow takes care of it all effortlessly, with just a few clicks.
Follow this comprehensive guide:
- Log into your account or register for a free trial with our service.
- Click +Create to upload a document from your device, cloud storage, or our template repository.
- Open your ‘Adac Second Hand Car Sales Contract’ in the editor.
- Click Me (Fill Out Now) to prepare the document on your end.
- Add and designate fillable fields for others (if needed).
- Proceed with the Send Invite settings to solicit eSignatures from others.
- Download, print your copy, or convert it into a reusable template.
No need to worry if you need to collaborate with your colleagues on your Adac Second Hand Car Sales Contract or send it for notarization—our platform provides everything you require to complete such tasks. Sign up with airSlate SignNow today and elevate your document management to new levels!