To
Re: Enhanced Claims Controls — Update and Reminder
In October 2009, AmeriChoice notified you of changes to the manner in which it would
implement controls to detect and prevent fraud, waste and abuse with regard to the TennCare
and Medicare programs utilizing a robust claims editing tool called the Ingenix Claims Editing
System or iCES. In late November or early December some of you may have received a notice
of recovery from Johnson and Rountree regarding these edits and prior claims payments.
AmeriChoice recognizes that many providers have voiced confusion and concern regarding
these recoveries. This letter addresses iCES and the recovery itself. Please read the following
information concerning the next steps in the current recovery process, as well as the references
to and the requirements for reporting your services in compliance with the claims edits (iCES
edits) as detailed in our Reimbursement policies.
The iCES edits will serve to improve the accuracy of claims payment, in accordance with the
fraud, waste and abuse protocols required for both the TennCare and Medicare programs.
These edits are drawn from a variety of sources, such as the National Correct Coding Initiative
(NCCI) which was developed by CMS to control incorrect coding in government health
programs; as well as coding conventions defined in the American Medical Association's CPT
manual, national and local policies and edits, coding guidelines developed by national
societies, and the analysis of standard medical and surgical practices. The iCES edits are more
robust than AmeriChoice's prior claims edits, which did not always identify certain coding
errors. At its core, however, iCES does not impose new billing requirements; rather iCES
merely collects into a single tool various pre-existing, generally applicable coding guidelines
which have long served to ensure program integrity standards that govern payment under the
TennCare program.
You will find a list of the AmeriChoice Policies which detail the specific claims edit(s) at the
end of this letter, on our website- go to www.Americhoice.com > Physicians>
Reimbursement Policies. It is important to note that these policies are consistent with ensuring
payment for EPSDT services.
We understand that the letters from Johnson and Rountree have caused confusion and
issues for you and your practice. AmeriChoice has chosen to suspend its current
recovery effort related to these Claims edits for the present.
As a result:
�•
Providers do not need to take any further action on the list of claims being
recovered due to iCES edits until they receive a new letter in early 2010.
•
This 2010 mailing will contain a revised claims list for recovery. AmeriChoice is
removing certain types of claims from the recovery including selected outpatient and
inpatient, Evaluation and Management services, subsequent immunization
administration services when billed with the code for the initial service, and codes for
preventive medicine visits.
•
Providers will be notified of all the claims that AmeriChoice will no longer recover
from its initial lists, and the remaining ones, if any, that are subject to recovery due to
iCES.
•
With the new notice of claims to be sent in early 2010, providers will be provided 45
days to appeal from the date of the new letters.
•
For any providers who have already submitted a check specific to this recovery to
Johnson and Rountree it will be returned to you in full.
.
•
•
Any providers that have submitted an appeal to Johnson and Rountree will also receive
a response back from them with the outcome of the appeal. Should you have any
questions regarding your appeal or a check that you submitted, please contact Johnson
and Rountree at 1-800-578-3300.
Claims that are being removed from the recovery project will show on the provider’s
remittance advice, but will not reflect a payment change.
Additional information about these controls that should be considered:
•
Fraud, waste and abuse controls are different than medical policies – whereas medical
policies reflect a level of medical evidence and necessity and may be implemented
through prior authorization or medical record reviews. The iCES program is
established to reflect correct billing practices under circumstances where multiple
services billed separately should be paid as one service (bundling edits), only once per
day (maximum frequency edits), or specific to values such as age/gender or bilateral
/unilateral services.
•
Claims or claim-lines can be denied, even if a service was approved by a priorauthorization. While the service may be approved, if the claim is not billed
appropriately, the fraud, waste and abuse controls will edit the claim per the applicable
coding protocols.
•
All fraud, waste and abuse controls have outside sourcing. These controls go through a
rigorous research and approval process to ensure that they are based on the CMS
Correct Coding Initiatives (CCI), the National Physician Fee Schedule (NPFS), or other
�external sources. For some controls such as the Anesthesia policy, these also use the
appropriate specialty society as additional references.
•
These enhanced controls are being fully implemented in the claims system and moving
forward will be applied as upfront edits.
Should you have any questions regarding these policies, you may contact us at 1-800-6901606.
Current Reimbursement Policies 12/13/2009 (include date of letter)
Add-On Codes (R0071)
This policy describes reimbursement for physician claims submitted with add-on codes. This
policy applies to services reported using the 1500 Health Insurance Claim Form (a/k/a CMS1500) or its electronic equivalent or its successor form.
Age and Gender to Diagnosis Code Policy (R0086)
This policy addresses edits involving diagnosis (ICD-9) codes with age and gender limitations.
This policy applies to services reported using the 1500 Health Insurance Claim Form (a/k/a
CMS-1500) or its electronic equivalent or its successor form.
Anesthesia Policy (R0032)
This policy describes reimbursement for anesthesia and pain management services. This
policy applies to services reported using the 1500 Health Insurance Claim Form (a/k/a CMS1500) or its electronic equivalent or its successor form.
Assistant Surgeon Policy (R5000)
This policy describes services provided by assistant surgeons that are reimbursable services
and the method for determining reimbursement amounts for assistant surgeon services.
Audiologic Vestibular Function Testing Code List - ICD 9 Filter (R0090)
This policy identifies circumstances in which reimbursement will be made to physicians or
other health care professionals for audiologic/ vestibular function testing to identify problems
with balance or hearing.
B Bundle Codes Policy (R0100)
This policy describes reimbursement of status "B" codes found on the National Physician Fee
Schedule (NPFS). This policy applies to services reported using the 1500 Health Insurance
Claim Form (a/k/a CMS-1500) or its electronic equivalent or its successor form.
Bilateral Procedures Policy (R0023)
This policy describes bilateral procedures and the application of multiple procedure
reductions. This policy applies to services reported using the 1500 Health Insurance Claim
Form (a/k/a CMS-1500) or its electronic equivalent or its successor form.
�Current Reimbursement Policies 12/13/2009 (include date of letter)
Form (a/k/a CMS-1500) or its electronic equivalent or its successor form.
CCI Editing Policy (R0105)
This policy describes National Correct Coding Initiative (NCCI) edits not otherwise addressed
in reimbursement policies to determine whether CPT and/or HCPCS codes reported together
are eligible for separate reimbursement. This policy applies to services reported using the
1500 Health Insurance Claim Form (a/k/a CMS-1500) or its electronic equivalent or its
successor form.
Care Plan Oversight Policy (R0033)
This policy describes reimbursement for Care Plan Oversight Services. This policy applies to
services reported using the 1500 Health Insurance Claim Form (a/k/a CMS-1500) or its
electronic equivalent or its successor form.
Co-Surgeon Team-Surgeon Policy (R0052)
This policy identifies the method of reimbursement for co-surgeons (modifier 62) and team
surgeons (modifier 66), and describes the circumstances under which assistant surgeon
services are reimbursable services in conjunction with services provided by a co-surgeon.
Contrast and Radiopharmaceutical Materials Policy (R0104)
This policy describes reimbursement for high and low osmolar contrast materials (Healthcare
Common Procedural Coding System [HCPCS] codes A4641, A4642. A9500-A9700, J1245,
Q3001, Q9951, Q9958, Q9959, Q9960, Q9961, Q9962, Q9963, Q9964, Q9965, Q9966 and
Q9967). This policy applies to services reported using the 1500 Health Insurance Claim Form
(a/k/a CMS-1500) or its electronic equivalent or its successor form.
Discontinued Procedure Policy (R0110)
This policy describes reimbursement for claims submitted with modifier 53 (discontinued
procedure). This policy does not apply to anesthesia services other than for Procedure Pain
Management Codes (PPMC). To report anesthesia services where a procedure has been
discontinued, see Anesthesia policy. This policy applies to services reported using the 1500
Health Insurance Claim Form (a/k/a CMS-1500) or its electronic equivalent or its successor
form.
Durable Medical Equipment, Orthotics and Prosthetics Multiple Frequency Policy
(R0109)
This policy describes the appropriate billing guidelines for reporting HCPCS (Healthcare
Common Procedural Coding System) codes with modifiers to indicate the rental, purchase,
and maintenance and service of equipment for participating network Durable Medical
Equipment (DME), orthotics or prosthetic vendors. The policy also addresses the frequency
limitations concerning the rental, rental to purchase, and maintenance and service of this
equipment. This policy applies to services reported using the 1500 Health Insurance Claim
Form (a/k/a CMS-1500) or its electronic equivalent or its successor form. This policy does not
apply to non-network DME, orthotics or prosthetic vendors, or home health services/home
health agencies, or to any physician or other health care professionals reporting DME,
orthotics or prosthetics services. Refer to the "Maximum Frequency per Day" policy for
information pertaining to reimbursement for physician claims submitted with multiple units
for the same CPT or HCPCS code on the same date of service.
�Current Reimbursement Policies 12/13/2009 (include date of letter)
apply to non-network DME, orthotics or prosthetic vendors, or home health services/home
health agencies, or to any physician or other health care professionals reporting DME,
orthotics or prosthetics services. Refer to the "Maximum Frequency per Day" policy for
information pertaining to reimbursement for physician claims submitted with multiple units
for the same CPT or HCPCS code on the same date of service.
Facet Joint - ICD 9 Filter (R0091)
This policy describes circumstances in which reimbursement will be provided for facet joint
nerve blocks. This policy applies to services reported using the 1500 Health Insurance Claim
form (a/k/a CMS-1500) or its electronic equivalent or its successor form.
Global Days Policy (R0005)
This policy identifies the global period of a procedure and the reimbursement for Evaluation
and Management (E/M) or other related services performed by a physician or other health care
professional that are included in that global period, as well as the use of modifiers to indicate
services that are not included in the global package. This policy does not apply to home health
care/home health agencies. This policy applies to services reported using the 1500 Health
Insurance Claim Form (a/k/a CMS-1500) or its electronic equivalent or its successor form.
Increased Procedural Services Policy (R0061)
This policy was formerly the Unusual Services Policy. This policy describes reimbursement
for claims submitted with modifier 22 (increased procedural services) or modifier 63
(procedure performed on infants less than 4 kg), but does not describe reimbursement for use
of modifier 22 in connection with anesthesia delivery services. See Anesthesia Policy. This
policy applies to services reported using the 1500 Health Insurance Claim Form (a/k/a CMS1500) or its electronic equivalent or its successor form.
Injections into the Tendon Sheath and Ligament, Ganglion Cyst, Carpal and Tarsal
Tunnel (R0070)
This policy describes circumstances in which reimbursement will be provided for injection(s)
to treat problems in the tendon/tendon sheath, ligament, ganglion cyst, carpal tunnel or tarsal
tunnel. This policy applies to services reported using the 1500 Health Insurance Claim Form
(a/k/a CMS-1500) or its electronic equivalent or its successor form.
Interventional Radiology Policy (R0011)
This policy describes reimbursement for interventional radiology procedures. This policy
applies to services reported using the 1500 Health Insurance Claim Form (a/k/a CMS-1500) or
its electronic equivalent or its successor form. This policy does not apply to anesthesiologists
or CRNAs. Please refer to the Anesthesia policy.
Laboratory Rebundling Policy (R0010)
This policy describes reimbursement of laboratory panels and component codes. This policy
applies to services reported using the 1500 Health Insurance Claim Form (a/k/a CMS-1500) or
its electronic equivalent or its successor form.
�Current Reimbursement Policies 12/13/2009 (include date of letter)
its electronic equivalent or its successor form.
Maximum Frequency Per Day Policy (R0060)
This policy describes reimbursement for physician claims submitted with multiple units for
the same Current Procedural Terminology (CPT®) or Healthcare Common Procedure Coding
System (HCPCS) code on the same date of service. This policy does not apply to: network
home health services and supplies/home health agencies; anesthesia services other than for
Procedure Pain Management Codes (PPMC) which are subject to the Maximum Frequency
per Day Policy; ambulance services; network physicians and other health care professionals
contracted at a case rate (in some markets known as a flat rate). For HCPCS codes reported
with rental modifiers (KH, KI, KJ, KR, or RR) or the Maintenance and Service modifier (MS)
by participating network durable medical equipment (DME), orthotics or prosthetics vendor,
please refer to Durable Medical Equipment, Orthotics and Prosthetics Multiple Frequency
Policy. This policy applies to services reported using the 1500 Health Insurance Claim Form
(a/k/a CMS-1500) or its electronic equivalent or its successor form.
Microsurgery Policy (R0038)
This policy describes the code ranges allowed for separate reimbursement for microsurgical
technique. This policy applies to services reported using the 1500 Health Insurance Claim
Form (a/k/a CMS-1500 ) or its electronic equivalent or its successor form.
Moderate Sedation Policy (R0035)
This policy was formerly the Intravenous/Conscious Sedation policy. The Moderate Sedation
policy describes reimbursement for moderate (conscious) sedation procedures. This policy
applies to services reported using the 1500 Health Insurance Claim Form (a/k/a CMS-1500) or
its electronic equivalent or its successor form.
Modifier 25 Policy (R0050)
This policy describes reimbursement for claims submitted with modifier 25 (Significant,
Separately Identifiable Evaluation and Management Service by the Same Physician on the
Same Day of the Procedure or Other Service). This policy applies to services reported using
the 1500 Health Insurance Claim Form (a/k/a CMS-1500) or its electronic equivalent or its
successor form.
Modifier 76 and 77 Policy (R0066)
This policy is a reference tool to guide readers to reimbursement policies in which the use of
modifier 76 (Repeat Procedure or Service by Same Physician) and/or modifier 77 (Repeat
Procedure by Another Physician) is discussed. This policy applies to services reported using
the 1500 Health Insurance Claim Form (a/k/a/ CMS-1500) or its electronic equivalent or its
successor form.
Multiple Procedure Policy (R0034)
This policy describes reimbursement related to multiple procedure reduction percentages,
which CPT and HCPCS codes are subject to multiple procedure reductions, and the method by
which procedures are determined to be primary versus secondary or subsequent. This policy
applies to services reported using the 1500 Health Insurance Claim Form (a/k/a CMS-1500) or
its electronic equivalent or its successor form.
�Current Reimbursement Policies 12/13/2009 (include date of letter)
This policy describes reimbursement related to multiple procedure reduction percentages,
which CPT and HCPCS codes are subject to multiple procedure reductions, and the method by
which procedures are determined to be primary versus secondary or subsequent. This policy
applies to services reported using the 1500 Health Insurance Claim Form (a/k/a CMS-1500) or
its electronic equivalent or its successor form.
New Patient Visit Policy (R0004)
This policy describes the appropriate use of new office/outpatient Evaluation and Management
(E/M) CPT and HCPCS codes. Home Health Care/ Home Health Agencies are excluded from
this policy.
Physical Medicine and Rehabilitation Policy Maximum Combined Frequency Per Day
(R0101)
This policy addresses reimbursement for certain timed therapy services provided in an office
or outpatient place of service. This policy applies to services reported using the 1500 Health
Insurance Claim Form (a/k/a CMS-1500) or its electronic equivalent or its successor form.
Physical Medicine and Rehabilitation Policy PT, OT and Evaluation and Management
(R0098)
This policy describes reimbursement for physical and occupational therapy evaluations. This
policy applies to services reported sing the 1500 Health Insurance Claim Form (a/k/a CMS1500) or its electronic equivalent or its successor form.
Physical Medicine and Rehabilitation Policy Speech Therapy (R0097)
This policy addresses procedure codes that will and will not be reimbursed for speech therapy.
This policy applies to services reported using the 1500 Health Insurance Claim Form (a/k/a
CMS-1500) or its electronic equivalent or its successor form.
Professional-Technical Component Policy (R0012)
This policy describes the professional and technical components of a global procedure code
and other matters related to professional, technical and global reimbursement. This policy
applies to services reported using the 1500 Health Insurance Claim Form (a/k/a CMS-1500) or
its electronic equivalent or its successor form.
Prolonged Services (R0003A)
This policy describes reimbursement of prolonged physician services involving direct (faceto-face) patient contact that are beyond the usual service in either the inpatient or outpatient
setting. This policy applies to services reported using the 1500 Health Insurance Claim Form
(a/k/a CMS-1500) or its electronic equivalent or its successor form.
RAST Testing - ICD 9 Filter (R0092)
This policy describes circumstances in which reimbursement will be provided for
radioallergosorbent (RAST) type tests.
�Current Reimbursement Policies 12/13/2009 (include date of letter)
radioallergosorbent (RAST) type tests.
Radiology Multiple Imaging Reduction Policy (R0085)
This policy describes reimbursement related to multiple imaging reduction percentages, which
CPT and HCPCS codes are subject to multiple imaging reductions, and the method by which
procedures are determined to be primary versus secondary or subsequent. This policy applies
to services reported using the 1500 Health Insurance Claim Form (a/k/a CMS-1500) or its
electronic equivalent or its successor form.
Rebundling Policy (R0056)
This policy provides an overview of coding relationships through rebundling edits. This
policy applies to services reported using the 1500 Health Insurance Claim Form (a/k/a CMS1500) or its electronic equivalent or its successor form.
Reduced Services Policy (R0065)
This policy describes reimbursement for claims submitted with modifier 52 (reduced
services). This policy applies to services reported using the 1500 Health Insurance Claim
Form (a/k/a CMS-1500) or its electronic equivalent or its successor form.
Remicade Policy (D0004)
This policy provides information about the use of Remicade (infliximab) and its recommended
use in the treatment of Crohn's disease, ulcerative colitis, rheumatoid arthritis, plaque
psoriasis, psoriatic psoriasis, and treatment-resistant sarcoidosis.
Respiratory Therapy Services Code List - ICD 9 Filter (R0093)
This policy describes circumstances in which reimbursement will be provided for respiratory
therapy services. This policy applies to services reported using the 1500 Health Insurance
Claim Form (a/k/a CMS-1500) or its electronic equivalent or its successor form.
Same Day-Same Service Policy (R0002)
This policy describes reimbursement for multiple medical services, including Evaluation and
Management (E/M) services, provided on the same date of service for the same patient by the
same physician or other health care professional. This policy applies to services reported using
the 1500 Health Insurance Claim Form (a/k/a CMS-1500) or its electronic equivalent or its
successor form.
Split Surgical Package Policy (R0106)
This policy describes reimbursement for services constituting components of the global
surgical package. This policy applies to services reported using the 1500 Health Insurance
Claim Form (a/k/a CMS-1500) or its electronic equivalent or its successor form.
Stand By Physician Policy (R3003)
This policy describes reimbursement for physician standby services. This policy applies to
services reported using the 1500 Health Insurance Claim Form (a/k/a CMS-1500) or its
electronic equivalent or its successor form.
�Current Reimbursement Policies 12/13/2009 (include date of letter)
This policy describes reimbursement for physician standby services. This policy applies to
services reported using the 1500 Health Insurance Claim Form (a/k/a CMS-1500) or its
electronic equivalent or its successor form.
Supply Policy (R0006)
This policy describes reimbursement for supplies and surgical trays. This policy applies to
services reported using the 1500 Health Insurance Claim Form (a/k/a CMS-1500) or its
electronic equivalent or its successor form.
T Status Codes Policy (R0107)
This policy describes reimbursement of codes with a status of "T" found on the Centers for
Medicare and Medicaid Services (CMS) National Physician Fee Schedule (NPFS). This policy
applies to services reported using the 1500 Health Insurance Claim form (a/k/a CMS-1500) or
its electronic equivalent or its successor form.
Telemedicine Policy (R0046)
This policy describes reimbursement for medical services delivered other than in-person (such
as over the phone, Internet or other communication devices), but does not include care plan
oversight services (see instead the Care Plan Oversight Policy). This policy applies to services
reported using the 1500 Health Insurance Claim Form (a/k/a CMS-1500) or its electronic
equivalent or its successor form.
Therapeutic and Diagnostic Injection Policy (R0009)
This policy describes reimbursement for therapeutic and diagnostic injection services (Current
Procedural Terminology (CPT®) codes 96372, 96373, 96374, 96375, 96376 and 96379) when
submitted with medications and/or evaluation and management (E/M) services. This policy
does not apply to DME and home health care/home health agencies. This policy applies to
services reported using the 1500 Health Insurance Claim Form (a/k/a CMS-1500) or its
electronic equivalent or its successor form.
Transforaminal Epidural Injections Policy (R0094)
This policy describes circumstances in which reimbursement will be provided for nerve block
transforaminal epidural injections. This policy applies to services reported using the 1500
Health Insurance Claim Form (a/k/a CMS-1500) or its electronic equivalent or its successor
form.
Trigger Point Injections Policy (R0067)
Document Size: (64 KB) Revised: 2009-05-18
This policy describes circumstances in which reimbursement will be provided for trigger point
injections. This policy applies to services reported using the 1500 Health Insurance Claim
form (a/k/a CMS-1500) or its electronic equivalent or its successor form.
�Current Reimbursement Policies 12/13/2009 (include date of letter)
Viral Hepatitis Serology Testing - ICD 9 Filter (R0096)
This policy describes circumstances in which reimbursement will be provided for viral
hepatitis serology testing.
�
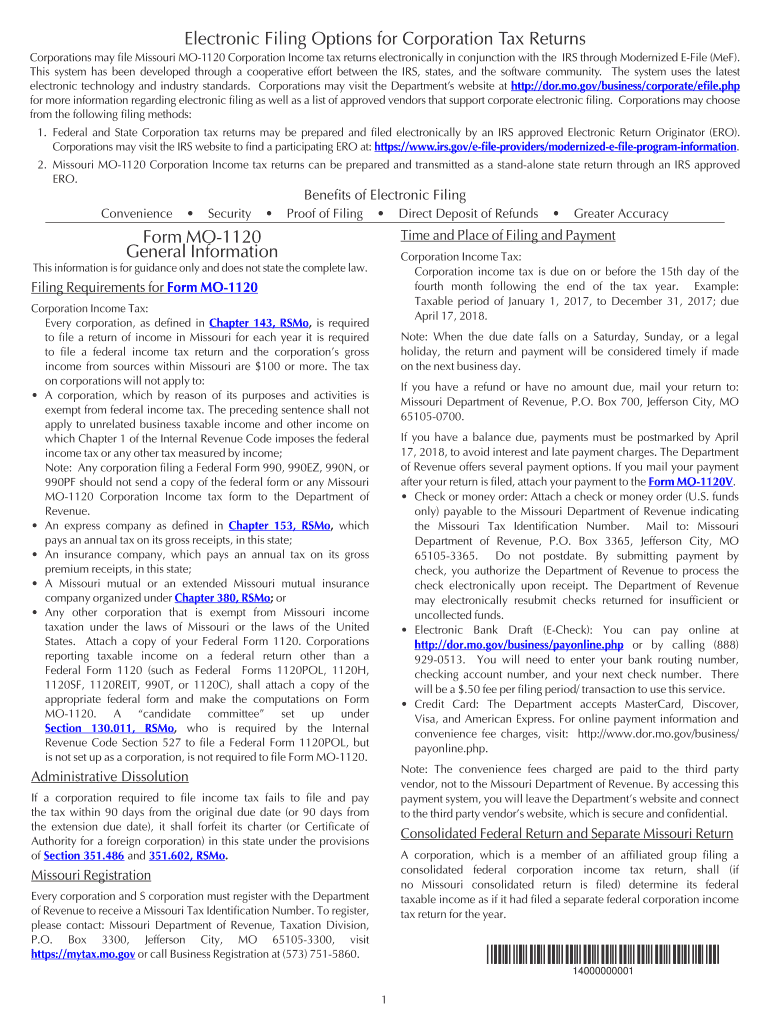
Valuable advice on preparing your ‘Corporations May File Missouri Mo 1120 Corporation Income Tax Returns Electronically In Conjunction With The Irs Through’ online
Are you exhausted by the burdens of handling paperwork? Look no further than airSlate SignNow, the premier eSignature tool for individuals and organizations. Bid farewell to the lengthy process of printing and scanning documents. With airSlate SignNow, you can seamlessly complete and endorse paperwork online. Utilize the extensive features embedded in this user-friendly and cost-effective platform to transform your approach to paperwork organization. Whether you need to authorize forms or collect electronic signatures, airSlate SignNow manages it all effortlessly, with just a few clicks.
Follow this comprehensive guide:
- Sign in to your account or sign up for a complimentary trial with our service.
- Click +Create to upload a file from your device, cloud storage, or our template library.
- Open your ‘Corporations May File Missouri Mo 1120 Corporation Income Tax Returns Electronically In Conjunction With The Irs Through’ in the editor.
- Click Me (Fill Out Now) to prepare the document on your end.
- Add and designate fillable fields for others (if necessary).
- Proceed with the Send Invite settings to solicit eSignatures from others.
- Save, print your copy, or convert it into a reusable template.
Don't fret if you need to collaborate with your colleagues on your Corporations May File Missouri Mo 1120 Corporation Income Tax Returns Electronically In Conjunction With The Irs Through or send it for notarization—our solution provides everything you require to accomplish such tasks. Create an account with airSlate SignNow today and elevate your document management to a new standard!