California Workers Compensation Senate Bill 899
Frequently Asked Questions
Networks, HCOs, Pre-Designated Doctors & Medical Control
● Can an employee pre-designate a chiropractor?
No, a “covered” employee, being transitioned into the Medical Provider Network (MPN) cannot predesignate a chiropractor based on our current interpretation. After implementation of the MPN, if an
injured worker is treating with a pre-designated chiropractor, the case manager will begin the transfer of
care process into the MPN unless the current claim status meets one of the four existing
conditions/illness (acute, chronic serious, terminal or performance of surgery/procedure) that prevents
an immediate transfer of medical care for a limited duration.
● How does Travelers assist with the preparation of medical providers?
Travelers worked with First Health to develop its Medical Provider Network. Travelers filed its application
and received approval from the Administrative Director (AD). All customers receive appropriate
implementation information and guidance. They may access a network listing on our website at
http://www.mywcinfo.com/geosite.aspx. Customers wishing to nominate providers to the MPN should
contact their local claim professional.
● Where does California now stand with physician pre-designation?
Physician pre-designation of medical doctors, osteopaths and also chiropractors has been allowed in
California for several years. The change in SB899 is that chiropractors can continue to be predesignated only by employees who are not subject to transitioning into an MPN. They can be elected as
the treating physician only after the employee has seen the facility/physician selected by the employer.
By contrast, pre-designation of medical doctors or doctors of osteopathy by employees will continue to
be honored, but only if one of two prerequisites is met. The employer must offer either (1) a nonoccupational group health coverage in a healthcare service plan, or (2) a non-occupational health
coverage in a group health plan or group health insurance policy. In addition to meeting one of those
two criteria, the physician to be pre-designated must agree to the pre-designation, must be the
employee’s regular physician and must be the employee’s primary care physician who has previously
directed the medical treatment of the employee.
● Medical control - how long do we have control?
Medical control with SB899 changed to life of claim on 1-1-05, with options to request new physicians
from the network unless the employee pre-designates. Currently, medical control continues for 30 days
unless the employer is in an HCO that can extend control to 180 days. With the implementation of the
MPN, medical control continues for the life of the claim for covered employees, although the employer
can lose medical control if, following a medical dispute and 2nd and 3rd opinions by network physicians,
an Independent Medical Reviewer (assigned by the AD) sides with the injured worker. At that point, the
injured worker has the option of treating outside of the network for that treatment or service, but it still
must be within the ACOEM guidelines. Further, if a necessary medical specialist is not available within a
reasonable geographic distance from the employee, the employee may also then obtain a physician
from outside the network. Travelers has a very extensive network of physicians in CA.
● How is SB899 going to affect older claims that were stipulated for future medical care?
Because the treatment was already agreed to via settlement, the limits on treatment (e.g., 24
chiropractic visits) likely will not apply. However, Travelers can and will work with physicians on
appropriate medical care. We will still try to enforce application of the ACOEM guidelines on these files.
�California Workers Compensation Senate Bill 899
● Will treatment on stipulated cases be restricted to the 24/24/24 for treatment, especially if they are
post-surgical?
If treatment has not yet been rendered, the limitations on chiropractic, orthopedic and occupational
therapy are 24 visits per claim for each discipline, for dates of injury of 1/1/04 and after. If the carrier
feels that additional treatment is appropriate, additional visits can be considered. If the date of injury was
on or after 1/1/04 and stipulated before 4/19/04, we may be able to enforce the limitation depending on
the future medical award. However, if the award expressly allows for a specific number of chiropractic,
orthopedic and occupational therapy visits per year (e.g., up to 12 visits annually), this limitation does
not apply.
● How large is our medical provider network?
The Administrative Director (AD) has established specific access standards required of all medical
provider networks. A MPN must have primary care and hospital services within 30 minutes or 15 miles
from each covered employee’s residence or workplace. A MPN must also have specialists within 60
minutes or 30 miles. The network that Travelers uses in CA meets these access standards, and has
more than 280 hospitals and over 52,000 medical and ancillary providers.
● What is the role of the HCO under the new law? Have HCOs been eliminated?
HCOs were not eliminated under the reform legislation. HCOs offer up to 180 days of medical control,
and the reform offers lifetime medical control, with options for injured workers to select a new physician
from the network, without the use of an HCO.
● How does the new law apply to old law cases? Can the ACOEM guidelines apply to those claims?
The new laws apply to old cases in various ways. However, the new guidelines can be used for cases
for which there have been no settlements or judgments concerning medical care.
● Will we have better control over treatment by doctors outside our system?
The reform provides employer medical control for the life of the claim. Injured workers who request a
new treating physician will need to choose from the network. Doctors outside of the network must still
comply with the ACOEM guidelines, as well as the Administrative Director (AD) guidelines, once
established.
● Explain about the new designated doctors situation. What is in effect right now?
We are assuming this refers to pre-designation by the employee. An employee can already predesignate. What’s new is that now the physician must agree to the pre-designation. Also, a prerequisite
for pre-designation is that the employer must offer either (1) non-occupational group health coverage in
a healthcare service plan or (2) non-occupational health coverage in a group health plan or a group
health insurance policy.
● If an employee has been going to her own physician or medical treatments and wants to make the
injury work related, do we send her to our physician?
Yes, if an employee wants to have workers compensation considered on a condition that was being
treated outside of workers compensation, then he or she would need to use the network provider of the
employer’s choice for the initial visit—assuming there was no valid pre-designation.
● How does the new legislation decrease "treatment time" on litigated claims? What avenues are
opened to diminish them?
The legislation already limits physical therapy, chiropractic and occupational therapy treatment to 24
�California Workers Compensation Senate Bill 899
visits per claim for dates of injury of 1/1/04 and after. Also, new medical treatment guidelines are being
instituted where in general no clear guideline existed. These items, plus the utilization review that has
already been established in CA and is in use by Travelers, should promote faster recovery times for
injured workers. The process for resolving medical disputes has also been streamlined.
Investigation
● What is the new process for denied claims?
The process for investigating a claim remains unchanged. However, during the delay period, if the
injured worker has completed and returned a DWC-1 Employee Claim form, the medical treatment will
be paid from the claim file until a compensability decision is made or $10,000.00 has been spent,
whichever comes first. Travelers has already undertaken additional training for our investigative
adjusters and nurses to ensure prompt and accurate decisions on compensability.
● How are the appeals boards handling apportionment?
It is too early to make any clear statements about how the WCAB views apportionment under the new
legislation. However, we have already experienced instances where the WCAB has required new
reports that address apportionment in accordance with SB899. Now, causation has to be addressed for
the report to be admissible. While there is a dispute about the ability to apportion to pathology, we
believe that this is now permitted, and we ask the doctors to discuss such apportionment.
● Since apportionment is now allowed, how does Travelers recommend we ask employees about
their pre-existing conditions? How is Travelers handling apportionment on existing claims?
Travelers believes pre-employment physicals are still appropriate. We do not advocate inappropriate
questions to employees. Changes to an employer’s internal processes should be discussed with
appropriate professionals such as labor attorneys or human resource experts. However, in the normal
course of claim investigation, you may be asked by our claim personnel for the name of the employee’s
health insurance carrier as well as a contact for same. On cases that have not been settled, Travelers
may seek new opinions on apportionment in line with the new legislation.
● What steps are being taken to address suspected fraudulent claims?
Travelers already possesses robust investigative capabilities in CA. We have a separate Special
Investigations unit as well as an extensive network of providers and facilities for investigation. Because
every claim must be reviewed on its own merits, we recommend any cases of concern be discussed
with your claim adjuster.
● How will this new legislation influence the number of add-on body parts and injuries after initial
filing?
The legislation does not prevent an injured worker from requesting that body parts be added. However,
because treatment will be with network physicians, it is possible that this practice could decrease.
Another potential outcome is that the changes could cause an increase in the number of cumulative
trauma claims in an effort to bypass the limitations on physical therapy, occupational therapy,
chiropractic visits and application of the AMA Guides for Rating Permanent Impairments. Travelers is
prepared to effectively manage such situations should they arise.
● We also do mandatory drug screening when an associate has an injury. Are ALL of the medical
providers going to do post-accident drug screening?
Post injury drug screening is not required under CA law. Because it is not used to cure or relieve an
injury, such screening is generally not done by medical providers as a normal course of business, and it
�California Workers Compensation Senate Bill 899
is not generally payable from a workers compensation claim. The exception is if there is a suspicion of
impairment leading to accident causation. However, in most cases if the employer wishes a postaccident drug screen, the employer arranges for that service with the physician and also pays for that
service.
Financial Impact
● Will the new law lead to reduced premiums for workers compensation insurance for large, mid-
size and small employers?
We believe that the current law has the potential to reduce the cost of claims in California. There are
many other items that affect insurance pricing. You should discuss pricing with your agent or broker,
who can address the issue specifically in view of your company’s unique circumstances.
● Will a rate reduction simply result in higher experience modifications?
Discussions related to rates and pricing should be held with your agent or broker.
● Do you think that reform can control the doctors and lawyers?
The objective of the reform is to ensure that injured workers are still treated and compensated
appropriately for their injuries. The changes in the reform appear to have the potential for reducing claim
costs.
● Will carriers who did not write workers compensation use this opportunity to write new business
and start cutting the price?
Unfortunately, it isn’t possible for us to predict what other companies will do.
● The PD amounts can be either increased or decreased by 15% depending on the ability of the
employer to provide a modified position for more than one year. Are the payments either
increased or decreased, or is the total award increased or decreased? What is the difference?
The increase or decrease applies to the weekly payment on any unaccrued permanent disability. It does
not increase the permanent disability percentage. For instance, if the employer offers permanent
modified duty within the 60-day time frame and there are 11 weeks of permanent disability still owing at
$100 per week, the weekly rate would be reduced to $85. If modified duty were not available, the rate
would be increased to $115.
● If you bring a staff member back to work in another position that meets with their physical
limitations, does their pay still have to stay at 85% of their current salary?
One way an alternate position qualifies as a viable position due to an employee’s limitations as result of
a work-related injury is that pay be within 85% of their pre-injury pay.
● What are the guidelines for receiving the 15% reduction?
The guideline for the 15% reduction is to offer a modified/alternate duty position within 60 days of
permanent and stationary status, and the position must last for at least 12 months, pay at least 85% of
pre-injury wage, and be within a reasonable commuting distance of the employee’s residence at the
time of injury.
Miscellaneous
● Do you think most of the insurance companies will have the same interpretation or the same
�California Workers Compensation Senate Bill 899
approach?
Unfortunately, it isn’t possible for us to predict what other companies will do. We do believe that there
will be litigation on some aspects of the reform as well as the potential for clean-up legislation.
● What has already gone into effect, and what is still to come?
Because of the length of the legislation, we recommend reviewing the prepared communications
available on SB899.
● Are there anymore changes coming?
We expect that there will be litigation on the reform as well as clean-up legislation.
● What has been the reaction of applicant attorneys?
All information we have in general is anecdotal. As indicated previously and as occurs with most law
changes concerning workers compensation in CA, some litigation is probable related to the changes.
● What policies and practices should we be following to be in compliance?
To obtain the most benefit from SB899, Travelers recommends prompt reporting, effective record
keeping, use of the physician network and a consistent and effective stay-at-work/return-to-work policy.
● How are reporting and documentation procedures affected?
Travelers recommends reporting claims as promptly as possible, providing the employee claim form
immediately when an injury is known or suspected, using the Travelers physician network in CA and
having an effective and consistent stay-at-work/return-to-work policy. All discussions with an injured
worker related to their claim should be documented.
● Do any of the changes affect existing open claims?
Yes. Apportionment, permanent disability, vocational rehabilitation and treatment can all be affected on
existing claims which have not been the subject of settlements or judgments.
�
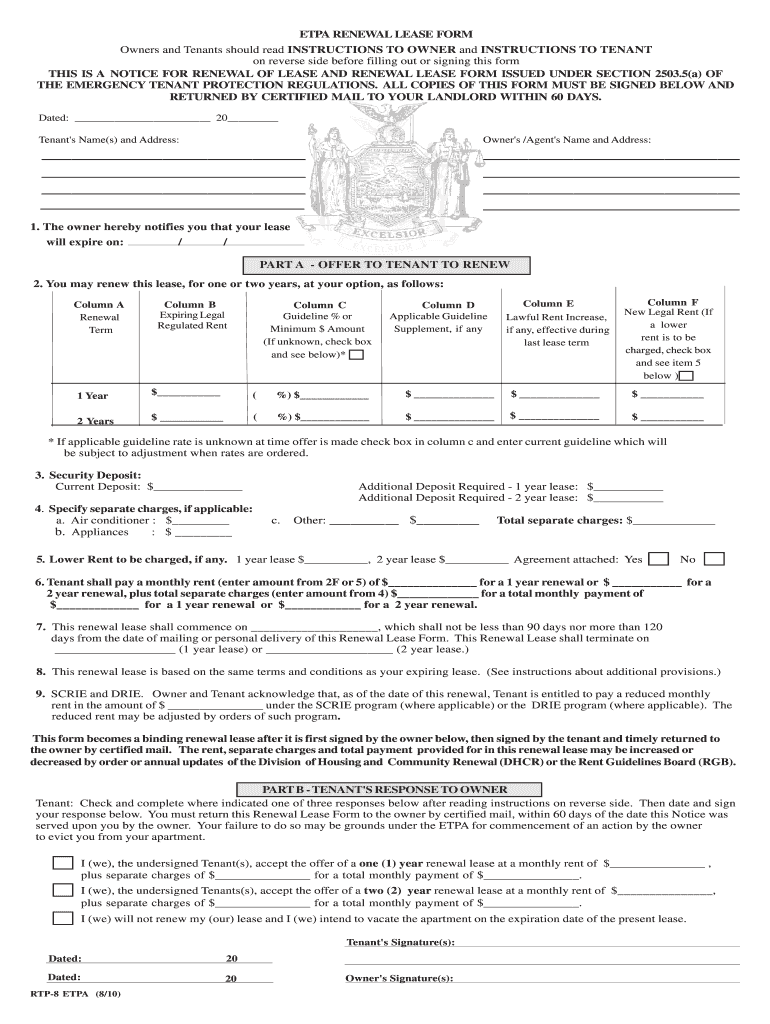
Convenient tips for preparing your ‘Rtp 8 Form’ online
Are you fed up with the inconvenience of handling paperwork? Look no further than airSlate SignNow, the premier electronic signature solution for both individuals and organizations. Bid farewell to the monotonous task of printing and scanning documents. With airSlate SignNow, you can effortlessly complete and sign documents online. Take advantage of the extensive features integrated into this user-friendly and affordable platform and transform your paperwork management approach. Whether you need to approve documents or collect signatures, airSlate SignNow handles everything with ease, needing just a few clicks.
Follow this guide step by step:
- Log into your account or sign up for a complimentary trial with our service.
- Click +Create to upload a file from your device, cloud storage, or our template library.
- Open your ‘Rtp 8 Form’ in the editor.
- Click Me (Fill Out Now) to finalize the form on your end.
- Add and designate fillable fields for others (if needed).
- Proceed with the Send Invite settings to request eSignatures from others.
- Save, print your version, or transform it into a reusable template.
Don’t worry if you need to collaborate with your colleagues on your Rtp 8 Form or send it for notarization—our platform provides you with everything necessary to accomplish such tasks. Register with airSlate SignNow today and elevate your document management to new levels!