Physical health and health risk factors in a population of
long-stay psychiatric patients
Irene Cormac, Michael Ferriter, Ram Benning and Carol Saul
Psychiatric Bulletin 2005, 29:18-20.
Access the most recent version at DOI: 10.1192/pb.29.1.18
References
Reprints/
permissions
You can respond
to this article at
Downloaded
from
This article cites 4 articles, 3 of which you can access for free at:
http://pb.rcpsych.org/content/29/1/18#BIBL
To obtain reprints or permission to reproduce material from this paper, please
write to permissions@rcpsych.ac.uk
http://pb.rcpsych.org/letters/submit/pbrcpsych;29/1/18
http://pb.rcpsych.org/ on September 6, 2014
Published by The Royal College of Psychiatrists
To subscribe to Psychiatric Bulletin go to:
http://pb.rcpsych.org/site/subscriptions/
�Cormac et al Health of long-stay psychiatric patients
Psychiatric Bulletin (20 05), 29, 18^20
original
papers
IRENE CORMAC , MIC HAEL FERRITER, R AM BENNING AND C AROL SAUL
Physical health and health risk factors in a population of
long-stay psychiatric patients
AIMS AND METHOD
To evaluate the physical health and
health risk factors in long-stay
psychiatric patients in a high secure
psychiatric hospital. A cross-sectional
survey of consenting patients was
undertaken using a semi-structured
questionnaire, a brief physical
examination and review of patient
case notes. A comparison was made
with data collected on admission and
held on the Special Hospitals’ Case
Register.
RESULTS
Main findings were: a mean increase
in weight since admission, in men of
10.62 kg and in women of 12.74 kg;
high rates of smoking, obesity
and large waist size; 54% of patients
had one or more health problems.
CLINICAL IMPLICATIONS
The study’s profile of the physical
health of psychiatric in-patients
indicates the need for health
promotion initiatives in such
hospitals and the need for primary
care services.
mine whether the patient’s psychotropic medication
carried a risk of weight gain. We noted the psychiatric
diagnoses according to ICD-10 criteria (World Health
Organization, 1992).
Central deposition of adipose tissue increases health
risk, and waist size is positively correlated with abdominal
fat content. Health risks in men are increased if waist size
exceeds 94 cm, and an intervention is needed if waist size
exceeds 102 cm. For women, waist sizes greater than
80 cm increase health risk and sizes greater than 88 cm
require intervention (Lean et al, 1995).
Measurements were taken of height, weight, waist
circumference and blood pressure using standard equipment, and body mass index (BMI) was calculated.
The Department of Health has made improvement of the
physical health of the population of the UK a priority.
Chronic psychiatric disorders are associated with
increased morbidity and premature mortality. The standardised mortality ratio of patients with schizophrenia is
nearly three times that of the general population; 60% of
the excess mortality can be attributed to the same broad
range of conditions that cause deaths in the general
population (Brown et al, 2000). The poor physical health
of psychiatric patients has been attributed to decreased
health awareness, fewer opportunities for a healthy lifestyle, high rates of smoking and the health risks associated with some psychotropic medications (Harris &
Barraclough, 1998).
Our study was designed to evaluate the physical
health of the patient population and health risk factors in
long-stay psychiatric patients in a high secure hospital.
Results
Demographics
Method
The hospital population comprised 460 patients, of
whom 31 were on trial leave, 22 were unable to give
informed consent and 159 refused to participate. Of the
248 patients who agreed to be interviewed, 214 were
men and 34 were women. Most patients in the sample
were White (200 of 248).
The age of interviewed patients ranged from 20.3
years to 80.7 years (mean 39.0 years, s.d.=10.75). The
length of stay of the patients ranged from 0.02 years to
46.20 years (mean 8.93 years, s.d.=7.98). The Mental
Health Act 1983 classifications of the sample were: 121
(49%) mental illness, 66 (27%) psychopathic disorder, 25
(10%) mental impairment or severe mental impairment;
36 (14%) had dual classifications.
The majority of the interviewed patients (131/248)
had schizophrenia and 119 had disorders of adult
personality and behaviour. There were 59 patients with
mental retardation (learning disabilities), which may be
associated with increased vulnerability to physical illness
and communication difficulties and thus compromise
access to physical healthcare. More than one form of
mental disorder was present in 115 patients.
A cross-sectional survey of the patients at Rampton
Hospital was undertaken between November 2000 and
March 2001. The local research ethics committee
approved the study. We obtained permission from the
ethics committee and the Caldicott Guardian to compare
the interviewed patients and non-interviewed patients on
key demographic variables. Permission was given to use
data held on the Special Hospitals’ Case Register; a
database holding information on all patients admitted to
Special Hospitals since 1972.
Two researchers (I.C. and R.B.) invited patients to
take part in the study. Patients were not approached if
their mental state was too disturbed or if they were
deemed incapable of giving informed consent. After
obtaining written consent, the researchers conducted a
semi-structured interview and examined the case notes,
collecting information on smoking habits, past history of
physical illness, current health problems and current
psychotropic and non-psychotropic medication. The
Maudsley criteria (Taylor et al, 2001) were used to deter-
18
�Cormac et al Health of long-stay psychiatric patients
Where data were available in the Special Hospitals’
Case Register, we compared weight on admission with
current weight. This showed that 70 of 430 (16%)
patients were admitted to Rampton Hospital with a BMI
of 30 kg/m2 or over. There was a substantial increase in
weight in most patients during their admission. In women
the mean gain was 12.74 kg (s.d.=17.02) and in men it
was 10.62 kg (s.d.=17.19).
Regarding waist size, 112 of 214 (53%) of male
patients and 26 of 34 (76%) female patients in the
sample had a waist size that required an intervention to
reduce health risk. The mean waist size in male patients
was 103.1cm (s.d.=14.4, range 68.5-156) and in female
patients it was 110.0 cm (s.d.=18.8, range 77.0-143.0).
Both of these means fall in the category of risk for which
an intervention is recommended.
Comparison of interviewed and
non-interviewed patients
There was no significant difference between the interviewed and non-interviewed patients in terms of age,
gender, ethnicity, Mental Health Act 1983 classification
or on data collected on admission on smoking habits,
alcohol problems and BMI. Non-interviewed patients had
a significantly greater mean length of stay than the
interviewed patients: 10.14 years (s.d.=9.04) compared
with 7.90 years (s.d.=6.80); t=12.97, P=0.003, 95% CI
73.73 to 70.76. This finding was not significant when
patients on trial leave were eliminated from the analysis.
Smoking
Seventy-one per cent of both male patients (152/214) and
female patients (24/34) reported smoking tobacco,
compared with 28% of the combined male and female
general population; 63% smoked loose tobacco (155/
248). The average daily consumption of cigarettes or
cigarette equivalents was 15.6. At this rate of tobacco
consumption, an individual is 13 times more likely to die
prematurely than a non-smoker (Action on Smoking and
Health, 2002).
Body mass index and psychotropic
medication
Table 1 shows the relationship between current medication and age, gender, ethnicity, length of stay, Mental
Health Act 1983 classification, current BMI and weight
change since admission. Those taking medication associated with side-effects of weight gain were significantly
more likely to be female, non-White, to have a shorter
length of stay, a classification of mental illness and a
higher mean BMI. There was no significant relationship
with BMI increase since admission.
There was no statistical difference between the
mean waist size for women taking medication with a risk
of weight gain and women not taking medication or
taking medication with no risk of weight gain. Male
Obesity and body shape
The rate of obesity in the hospital sample was 36% in
men and 75% in women. This should be compared with
rates of obesity in the UK population of 17% in men and
22% in women (Peterson et al, 2000). Just three patients
(1.2%) were underweight.
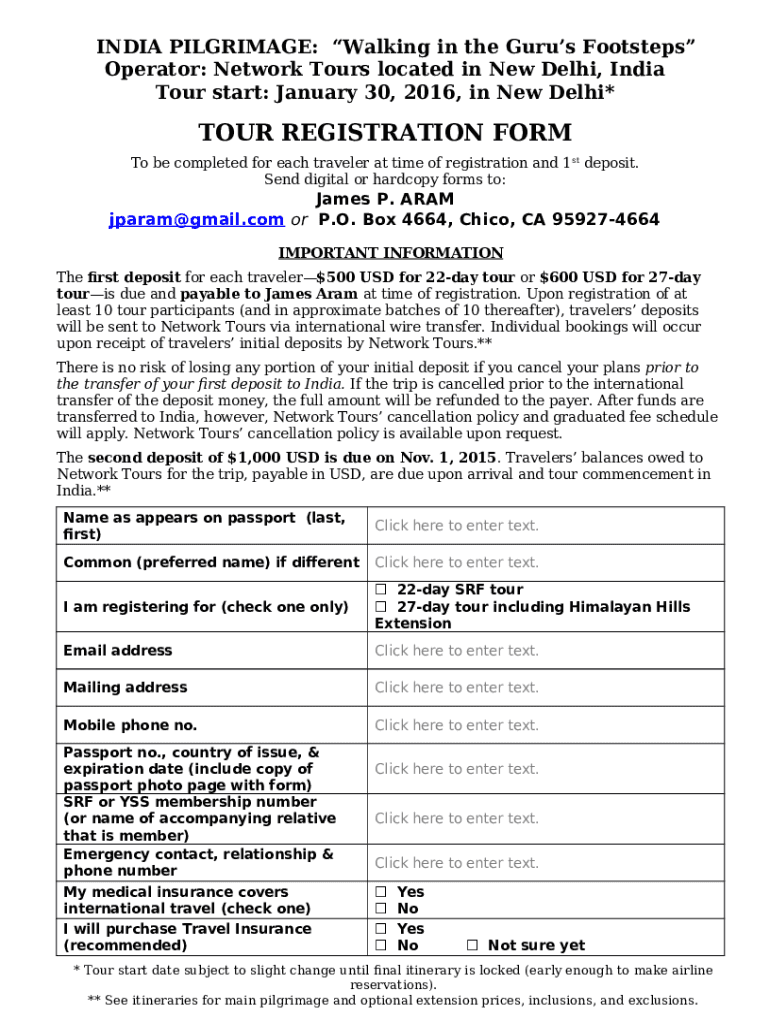
Table 1. Comparison of patients taking medication with potential for weight gain and those not taking such medication
Age, years: mean (s.d.)
Gender, n / N (%)
Male
Female
Ethnicity, n / N (%)
White
Non-White
Length of stay, years: mean (s.d.)
Mental Health Act 1983 classification, n / N (%)
Mental illness
Personality disorder
Mental impairment/severe
mental impairment
Other
Current body mass index, kg/m2: mean (s.d.)
Taking weight-gaining
medication ( n=181)
Not taking weightgaining medication
( n=67)
37.5 (10.4)
40.2 (10.7)
t=1.79, d.f.=246,
P=0.074 (95% CI
70.27 to 5.7)
149/214 (70)
32/34 (94)
65/214 (30)
2/34 (6)
w2=8.92, d.f.=1,
P=0.003
139/200 (70)
42/48 (88)
7.4 (6.3)
61/200 (30)
6/48 (12)
9.4 (7.8)
w2=6.36, d.f.=1,
P=0.012
t=2.10, d.f.=246,
P=0.037 (95% CI 0.95
to 0.13)
106/121 (88)
28/66 (42)
16/25 (64)
15/121 (12)
38/66 (58)
9/25 (36)
w2=48.55, d.f.=3,
P=0.0001
31/36 (86)
29.8 (7.4)
5/36 (14)
27.5 (5.8)
19
Significance
t=72.33, d.f.=246,
P=0.020 (95% CI 1.0
to 74.3)
original
papers
�Cormac et al Health of long-stay psychiatric patients
Table 2. Medical conditions of patients interviewed
original
papers
Illness category
Gastroenterology
Neurological
Respiratory
Rheumatology/bone
Cardiovascular
Diabetes and metabolic
Dermatology
Ear, nose and throat (including deafness)
Ophthalmology
Endocrinology
The study findings have raised serious concerns
about avoidable health risks in a population of long-stay
psychiatric patients. These risks include high rates of
smoking, obesity, central weight distribution and excessive weight gain. The results of this study should be seen
in the context of increased health risks, morbidity and
mortality in psychiatric populations elsewhere and in the
general population.
There are well-developed and proven strategies for
decreasing health risk factors that could be implemented
in long-stay psychiatric facilities (Cormac et al, 2004).
Since the completion of this study, Rampton Hospital has
developed interventions for health promotion for longstay psychiatric patients. Further research is needed in
this important area of patient care.
Psychiatric hospitals have a responsibility for the
physical health of their patients. Hospitals should
promote healthy living and provide the same standard of
healthcare that is available to the general population. This
paper shows the need for the provision of primary care
services and health promotion for psychiatric patients
with mental disorders.
Patients with
health problems
n (%)
40 (16)
37 (15)
36 (14)
29 (12)
27 (11)
23 (9)
19 (8)
9 (4)
7 (3)
7 (3)
patients taking medication with a risk of weight gain had
a statistically significant greater mean waist size
( t=72.874, P=0.004) than male patients on no medication or taking medication with no risk of weight gain.
Hypertension
We found that 103 (48%) of the 214 interviewed male
patients and 3 (9%) of the 34 interviewed female
patients might be at risk due to hypertension. In
comparison, the levels of hypertension in the British
population are 41% of men and 33% of women (Britton
& McPherson, 2002).
Declaration of interest
None.
References
ACTION ON SMOKING AND HEALTH
(2002) Passive Smoking. Fact Sheet No.
8. London: ASH.
General patient morbidity
We found that 90 (36%) of our sample reported being
breathless after climbing one flight of stairs; 134 (54%)
had one or more diagnosed significant health problems.
Table 2 shows the number and percentage of patients
with health problems in the ten most frequently reported
medical categories.
BRITTON, A. & McPHERSON, K. (2002)
Coronary Heart Disease: Estimating
the Impact of Changes in Risk Factors.
London: National Heart Forum.
BROWN, S., INSKIP, H. &
BARRACLOUGH, B. (2000) Causes of
the excess mortality of schizophrenia.
British Journal of Psychiatry, 177,
212-217.
Discussion
CORMAC, I., FERRITER, M. & MARTIN,
D. (2004) Improving the physical health
of long-stay psychiatric in-patients.
Advances in PsychiatricTreatment, 10,
107-115.
Owing to the cross-sectional design of the study, it was
not possible to determine the aetiology or development
of the physical health problems. No invasive procedures
were undertaken, such as measurement of cholesterol
levels, as this might have deterred patients from participation in the study. We could not measure levels of
physical activity. Blood pressure measurements should be
taken at least three times before a diagnosis of hypertension is made. However, we were only able to make
one measurement for each patient. The patients’ recall of
past health problems might have been biased by their
current mental and physical health status (selective recall
bias).
HARRIS, E. C. & BARRACLOUGH, B.
(1998) Excess mortality of mental
disorder. British Journal of Psychiatry,
137,11-53.
LEAN, M. E. J., HAN,T. S. & MORRISON,
C. E. (1995) Waist circumference as a
measure for indicating need for
weight measurement. BMJ, 311,
158-161.
PETERSON, S., RAYNOR, M. & PRESS,V.
(2000) Coronary Heart Disease
Statistics. London: British Heart
Foundation.
TAYLOR, D., McCONNELL, H.,
McCONNELL, D., et al (2001)
Prescribing Guidelines (6th edn), p.105.
London: Martin Dunitz.
WORLDHEALTHORGANIZATION (1992)
The ICD-Classification of Mental and
Behavioural Disorders. Clinical
Descriptions and Diagnostic Guidelines.
Geneva:WHO.
*Irene Cormac Consultant Forensic Psychiatrist with Special Interest in Physical
Healthcare, Rampton Hospital, Nottinghamshire Healthcare NHS Trust, Retford
DN22 0PD (tel: 01777 248321; fax: 01777 247737; e-mail: irene.cormac@
nottshc.nhs.uk), Michael Ferriter Research Fellow, Rampton Hospital,
Ram Benning Locum Consultant Forensic Psychiatrist, Derby City General
Hospital, Carol Saul Research Fellow, Section of Mental Health, University of
Sheffield
20
�