Ensuring Compliance with Digital Signature Lawfulness for Physical Exam Consent in United Kingdom
- Quick to start
- Easy-to-use
- 24/7 support
Simplified document journeys for small teams and individuals




We spread the word about digital transformation
Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.







Your complete how-to guide - digital signature lawfulness for physical exam consent in united kingdom
Digital Signature Lawfulness for Physical Exam Consent in United Kingdom
When it comes to ensuring the lawfulness of digital signatures for physical exam consent in the United Kingdom, it is essential to follow the proper procedures. By utilizing airSlate SignNow, businesses can streamline this process and ensure compliance with regulations.
Steps to Utilize airSlate SignNow for Digital Signatures:
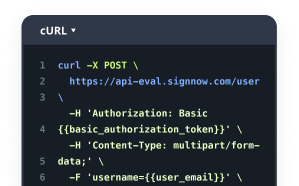
- Launch the airSlate SignNow web page in your browser.
- Sign up for a free trial or log in.
- Upload a document you want to sign or send for signing.
- If you're going to reuse your document later, turn it into a template.
- Open your file and make edits: add fillable fields or insert information.
- Sign your document and add signature fields for the recipients.
- Click Continue to set up and send an eSignature invite.
airSlate SignNow empowers businesses to send and eSign documents with an easy-to-use, cost-effective solution. It offers great ROI with a rich feature set and is tailored for SMBs and Mid-Market. The platform also provides transparent pricing with no hidden support fees and add-on costs, along with superior 24/7 support for all paid plans.
Discover the benefits of airSlate SignNow today and revolutionize your document signing process!
How it works
Rate your experience
What is the digital signature lawfulness for physical exam consent in the United Kingdom
The digital signature lawfulness for physical exam consent in the United Kingdom refers to the legal framework that governs the use of electronic signatures in medical and healthcare settings. This framework ensures that electronic consent forms are valid and enforceable, provided they meet specific criteria set forth by UK law. In essence, digital signatures serve as a secure and efficient means for patients to provide consent for physical examinations, ensuring that their rights and privacy are maintained throughout the process.
How to use the digital signature lawfulness for physical exam consent in the United Kingdom
To utilize the digital signature lawfulness for physical exam consent, healthcare providers can incorporate electronic signature solutions into their workflows. This involves creating a digital consent form that patients can fill out and sign online. Providers should ensure that the platform used complies with legal standards, offering features such as secure storage, audit trails, and user authentication. By doing so, they can streamline the consent process while maintaining compliance with applicable laws.
Steps to complete the digital signature lawfulness for physical exam consent in the United Kingdom
Completing the digital signature lawfulness for physical exam consent involves several key steps:
- Prepare the consent form, ensuring it includes all necessary information about the examination and the patient's rights.
- Upload the form to an electronic signature platform, such as airSlate SignNow, which allows for easy editing and customization.
- Send the form to the patient for review, ensuring they understand the content and implications of their consent.
- Allow the patient to fill out the form and eSign it electronically, using a secure method that verifies their identity.
- Once signed, securely store the completed document for future reference and compliance purposes.
Legal use of the digital signature lawfulness for physical exam consent in the United Kingdom
The legal use of digital signatures for physical exam consent in the United Kingdom is governed by the Electronic Communications Act and the eIDAS Regulation. These laws establish that electronic signatures hold the same legal weight as traditional handwritten signatures, provided they meet specific criteria. This includes ensuring that the signature is uniquely linked to the signer, capable of identifying the signer, and created using means that the signer can maintain under their sole control.
Security & Compliance Guidelines
When implementing digital signatures for physical exam consent, it is crucial to adhere to security and compliance guidelines to protect patient information. This includes:
- Utilizing platforms that offer encryption and secure data storage to safeguard sensitive information.
- Ensuring that the electronic signature solution complies with relevant regulations, such as HIPAA in the United States, to protect patient privacy.
- Implementing authentication measures, such as two-factor authentication, to verify the identity of the signer.
- Maintaining an audit trail that records all actions taken on the document, providing transparency and accountability.
Examples of using the digital signature lawfulness for physical exam consent in the United Kingdom
Examples of using digital signatures for physical exam consent include:
- Patients signing consent forms for routine physical examinations before their appointments, allowing for quicker processing at the healthcare facility.
- Telehealth providers obtaining consent for remote examinations or consultations, ensuring that patients can participate from the comfort of their homes.
- Healthcare organizations using digital signatures to streamline their administrative processes, reducing paperwork and improving efficiency.
-
Best ROI. Our customers achieve an average 7x ROI within the first six months.
-
Scales with your use cases. From SMBs to mid-market, airSlate SignNow delivers results for businesses of all sizes.
-
Intuitive UI and API. Sign and send documents from your apps in minutes.
FAQs
-
What is the digital signature lawfulness for physical exam consent in the United Kingdom?
In the United Kingdom, the digital signature lawfulness for physical exam consent is recognized under the Electronic Communications Act 2000 and the eIDAS Regulation. This means that digital signatures can be legally binding for consent forms, including those for physical exams, provided they meet certain criteria. Using a reliable eSignature solution like airSlate SignNow ensures compliance with these laws.
-
How does airSlate SignNow ensure compliance with digital signature lawfulness for physical exam consent in the UK?
airSlate SignNow adheres to the legal standards set forth by UK law regarding digital signatures. Our platform employs advanced encryption and authentication methods to ensure that all signed documents are secure and legally valid. This guarantees that your physical exam consent forms are compliant with the digital signature lawfulness for physical exam consent in the United Kingdom.
-
What features does airSlate SignNow offer for managing physical exam consent documents?
airSlate SignNow provides a range of features tailored for managing physical exam consent documents, including customizable templates, automated workflows, and real-time tracking of document status. These features streamline the signing process and enhance the overall efficiency of obtaining consent. This ensures that you can easily comply with the digital signature lawfulness for physical exam consent in the United Kingdom.
-
Is airSlate SignNow cost-effective for small businesses needing digital signatures?
Yes, airSlate SignNow offers competitive pricing plans that cater to small businesses looking for cost-effective digital signature solutions. Our pricing structure is designed to provide maximum value without compromising on features or compliance. This makes it an ideal choice for businesses needing to adhere to the digital signature lawfulness for physical exam consent in the United Kingdom.
-
Can airSlate SignNow integrate with other software for managing consent forms?
Absolutely! airSlate SignNow seamlessly integrates with various software applications, including CRM systems and document management tools. This integration capability allows businesses to streamline their workflows and ensure that all consent forms, including those for physical exams, comply with the digital signature lawfulness for physical exam consent in the United Kingdom.
-
What are the benefits of using airSlate SignNow for physical exam consent?
Using airSlate SignNow for physical exam consent offers numerous benefits, including enhanced security, improved efficiency, and reduced paper usage. Our platform simplifies the signing process, making it easier for patients to provide consent digitally. This aligns with the digital signature lawfulness for physical exam consent in the United Kingdom, ensuring that your processes are both modern and compliant.
-
How secure is airSlate SignNow for handling sensitive consent documents?
airSlate SignNow prioritizes security by employing industry-standard encryption and secure storage for all documents. Our platform is designed to protect sensitive information, ensuring that consent documents remain confidential and tamper-proof. This commitment to security supports the digital signature lawfulness for physical exam consent in the United Kingdom.
Related searches to digital signature lawfulness for physical exam consent in united kingdom
Join over 28 million airSlate SignNow users
Get more for digital signature lawfulness for physical exam consent in united kingdom
- Unlock the potential of eSignature legitimacy for ...
- ESignature Legitimacy for Affidavit of Service in ...
- ESignature Legitimacy for Affidavit of Service in ...
- Unlock eSignature Legitimacy for Affidavit of Service ...
- Unlocking eSignature Legitimacy for Affidavit of ...
- Unlock eSignature Legitimacy for Affidavit of Service ...
- Enhance eSignature Legitimacy for Affidavit of Service ...
- Unlock eSignature Legitimacy for Affidavit of Service ...