Digital Signature Licitness for Physical Exam Consent in United Kingdom
- Quick to start
- Easy-to-use
- 24/7 support
Simplified document journeys for small teams and individuals




We spread the word about digital transformation
Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.







What is the digital signature licitness for physical exam consent in the United Kingdom
The digital signature licitness for physical exam consent in the United Kingdom refers to the legal validity and acceptance of electronic signatures in the context of consent forms for physical examinations. In the UK, electronic signatures are recognized under the Electronic Communications Act 2000 and the eIDAS Regulation, which establishes that electronic signatures hold the same legal standing as handwritten signatures, provided they meet certain criteria. This means that healthcare providers can use digital signatures to obtain consent for physical exams, streamlining the process while ensuring compliance with legal standards.
How to use the digital signature licitness for physical exam consent in the United Kingdom
To effectively utilize the digital signature licitness for physical exam consent, healthcare providers should integrate electronic signature solutions into their workflow. This involves creating a digital consent form that can be filled out online. Once the form is prepared, providers can send it electronically to patients for their signature. Patients can complete the form from any device, sign it using an eSignature, and submit it back securely. This process not only enhances efficiency but also maintains compliance with legal requirements.
Steps to complete the digital signature licitness for physical exam consent in the United Kingdom
Completing the digital signature licitness for physical exam consent involves several straightforward steps:
- Create a digital consent form using an electronic signature platform.
- Send the form to the patient via email or a secure link.
- The patient fills out the required information directly on the form.
- Once completed, the patient applies their digital signature.
- The signed document is automatically returned to the provider for record-keeping.
This process ensures that both parties have access to a legally binding document without the need for physical paperwork.
Legal use of the digital signature licitness for physical exam consent in the United Kingdom
The legal use of digital signatures for physical exam consent in the United Kingdom is supported by legislation that recognizes electronic signatures as valid. To ensure compliance, the digital signature must be uniquely linked to the signatory, capable of identifying the signatory, and created using secure methods that protect the integrity of the signed document. Healthcare providers must also ensure that they retain records of consent forms in a secure manner to comply with data protection regulations.
Security & Compliance Guidelines
When using digital signatures for physical exam consent, it is essential to adhere to security and compliance guidelines to protect patient information. Key practices include:
- Utilizing encryption to secure data during transmission and storage.
- Implementing multi-factor authentication for signatories.
- Regularly updating software and security protocols to mitigate risks.
- Ensuring compliance with relevant regulations, such as GDPR, for data protection.
By following these guidelines, healthcare providers can ensure that the digital signature process remains secure and compliant with legal standards.
Sending & Signing Methods (Web / Mobile / App)
Digital signatures for physical exam consent can be executed through various methods, enhancing accessibility for both patients and providers. Users can send and sign documents via:
- Web browsers, allowing for easy access from any device with internet connectivity.
- Mobile applications, which facilitate signing on-the-go for patients.
- Desktop applications, providing a robust platform for managing documents securely.
These methods ensure that the signing process is convenient and efficient, catering to the preferences of users.
-
Best ROI. Our customers achieve an average 7x ROI within the first six months.
-
Scales with your use cases. From SMBs to mid-market, airSlate SignNow delivers results for businesses of all sizes.
-
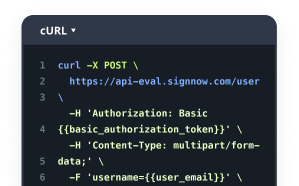
Intuitive UI and API. Sign and send documents from your apps in minutes.
FAQs
-
What is the digital signature licitness for physical exam consent in the United Kingdom?
The digital signature licitness for physical exam consent in the United Kingdom refers to the legal validity of electronic signatures used for consent forms. In the UK, electronic signatures are recognized under the Electronic Communications Act 2000 and the eIDAS Regulation, making them a legitimate option for obtaining consent in medical settings.
-
How does airSlate SignNow ensure compliance with digital signature licitness for physical exam consent in the United Kingdom?
airSlate SignNow complies with the legal standards set forth by UK law regarding digital signatures. Our platform employs advanced encryption and authentication methods to ensure that all signed documents meet the requirements for digital signature licitness for physical exam consent in the United Kingdom.
-
What features does airSlate SignNow offer for managing physical exam consent forms?
airSlate SignNow provides a range of features for managing physical exam consent forms, including customizable templates, secure storage, and real-time tracking of document status. These features enhance the efficiency of obtaining digital signature licitness for physical exam consent in the United Kingdom.
-
Is airSlate SignNow cost-effective for obtaining digital signatures?
Yes, airSlate SignNow offers a cost-effective solution for obtaining digital signatures. Our pricing plans are designed to accommodate businesses of all sizes, ensuring that you can achieve digital signature licitness for physical exam consent in the United Kingdom without breaking the bank.
-
Can airSlate SignNow integrate with other software for managing consent forms?
Absolutely! airSlate SignNow integrates seamlessly with various software applications, allowing you to streamline your workflow. This integration capability supports the digital signature licitness for physical exam consent in the United Kingdom by ensuring that all your documents are easily accessible and manageable.
-
What are the benefits of using airSlate SignNow for physical exam consent?
Using airSlate SignNow for physical exam consent offers numerous benefits, including increased efficiency, reduced paperwork, and enhanced security. By ensuring digital signature licitness for physical exam consent in the United Kingdom, you can focus more on patient care and less on administrative tasks.
-
How secure is the digital signature process with airSlate SignNow?
The digital signature process with airSlate SignNow is highly secure, utilizing encryption and secure access protocols to protect your documents. This level of security is essential for maintaining digital signature licitness for physical exam consent in the United Kingdom, ensuring that sensitive information remains confidential.