INITIAL INFORMATION LETTER TO INSURED/CLAIMANT/PROVIDERS
Sent on Concentra Integrated Services Letter Head
Dear Insured and/or /Eligible Injured Person/Medical Provider:
Please read this letter carefully because it provides specific information concerning how a medical
claim under Personal Injury Protection coverage will be handled, including specific requirements
which you must follow in order to ensure payment for medically necessary treatment, tests,
durable medical equipment and prescription drugs that a named insured or eligible injured person
may incur as a result of an auto accident.
Decision Point Review
The New Jersey Department of Banking and Insurance has published standard courses of
treatment, Care Paths, for soft tissue injuries of the neck and back, collectively referred to as
Identified Injuries. The Care Paths provide that treatment be evaluated at certain intervals called
Decision Points. At decision points, either you or the treating health care provider must provide
us with information about further treatment that is intended to be provided (this is referred to as
Decision Point Review). Such information includes reasonable prior notice and the appropriate
clinically supported findings that are being relied upon to support that the anticipated treatment or
test is medically necessary. The Decision Point Review requirements do not apply to treatment or
diagnostic tests administered during emergency care or during the first 10 days after the accident
causing the injury. The Care Paths and accompanying rules, are available on the Internet on the
Department's website at http://www.nj.gov/dobi/aicrapg.htm (Scroll down to PIP Reforms) or by
calling CONCENTRA INTEGRATED SERVICES, INC at 888-451-7952 for MetLife Auto &
Home and MetLife’s website at www.MetLife.com.
In addition, the administration of certain diagnostic tests is subject to Decision Point Review
regardless of the diagnosis. The following tests are subject to decision point review:
•
•
•
•
•
•
•
•
•
•
•
Needle electromyography (needle EMG)
Somatosensory evoked potential (SSEP), visual evoked potential (VEP), brain audio
evoked potential (BAEP), brain evoked potential (BEP), nerve condition
velocity(NCV), and H-reflex study
Electroencephalogram (EEG)
Videofluoroscopy
Magnetic resonance imaging (MRI)
Computer assisted tomographic studies (CT, CAT scan)
Dynatron/cyber station/cybex
Sonograms/ultrasound
Thermography / Thermograms
Brain Mapping
Any other diagnostic test that is subject to the requirements of the Decision Point
Review Plan by New Jersey law or regulation.
1
�These diagnostic tests must be administered in accordance with New Jersey Department of
Banking and Insurance regulations which set forth the requirements for the use of diagnostic tests
in evaluation injuries sustained in an auto accident.
We will notify you or your treating health care provider of our decision to authorize or deny
reimbursement of the treatment or test as promptly as possible, but no later than three business
days after a request has been made. A request for treatment, testing, durable medical equipment
or prescription drugs is to be submitted together with legible, conspicuously presented, clinically
supported findings that the proposed treatment, testing, durable medical equipment or prescription
drugs is in accordance with the standards of medical necessity established under MetLife Auto &
Home policy and New Jersey law. Any denial of reimbursement for further medical treatment or
tests will be based on the determination of a physician or dentist. If we fail to take any action or
fail to respond within three business days after receiving the required notification and supporting
medical documentation at a decision point, then the treating health care provider is permitted to
continue the course of treatment until we provide the required notice. Please note that the
decision point review requirements do not apply to treatment or diagnostic tests administered
during emergency care.
If requests for decision point reviews are not submitted or clinically supported findings that
support the request are not supplied, payment of your bills will be subject to a penalty co-payment
of 50 percent even if the services are determined to be medically necessary. This co-payment is in
addition to any deductible or co-payment required under the Personal Injury Protection coverage.
Mandatory Precertification
New Jersey regulation provides that insurers may require precertification of certain treatments or
diagnostic tests for other types of injuries or tests not included in the Care Paths. Precertification
means providing us with notification of intended medical procedures, treatments, diagnostic tests,
prescription supplies, durable medical equipment or other potentially covered medical expenses.
Precertification does not apply to treatment or diagnostic tests administered during emergency
care or during the first ten days after the accident causing the injury.
The following are procedures, treatments, diagnostic tests, prescription supplies, durable medical
equipment or other potentially covered medical expenses for which precertification is required:
•
•
•
•
•
•
•
Non-emergency inpatient and outpatient hospital care;
Non-emergency surgical procedures;
Extended care rehabilitation facilities;
Outpatient care for soft-tissue/disc injuries of the person’s neck, back and related
structures not included within the diagnoses covered by the Care Paths;
Physical, Occupational, speech, cognitive or other restorative therapy or other therapeutic
or body-part manipulation including manipulation under anesthesia except that provided
for identified injuries in accordance with decision point review;
Outpatient psychological / psychiatric services and testing including biofeedback;
All pain management services except as provided for identified injuries in accordance with
2
�•
•
•
•
•
•
•
•
•
decision point review;
Home health care;
Non-emergency dental restoration;
Temporomandibular disorder; any oral facial syndrome; Infusion therapy;
Bone scans;
Vax-D
Transportation Services costing more than $50.00;
Brain Mapping other than provided under Decision Point Review;
Durable Medical Equipment including orthotics and prosthestics costing more than $50.00;
Prescriptions costing more than $50.00;
Our approval of requests for precertification will be based exclusively on medical necessity, as
determined by using standards of good practice and standard professional treatment protocols,
including, but not limited to, Care Paths recognized by the Commissioner of Banking and
Insurance. Our final determination of the medical necessity of any disputed issues shall be made
by a physician or dentist as appropriate for the injury and treatment contemplated.
If requests for precertification are not submitted or clinically supported findings that support the
request are not supplied, payment of your bills will be subject to a penalty co-payment of 50
percent even if the services are determined to be medically necessary. This co-payment is in
addition to any deductible or co-payment required under the Personal Injury Protection coverage.
Voluntary Precertification
Health care providers are encouraged to participate in a voluntary precertification process by
providing CONCENTRA INTEGRATED SERVICES, INC with a comprehensive treatment
plan for both identified and other injuries.
CONCENTRA INTEGRATED SERVICES, INC will utilize nationally accepted criteria and the
Care Paths to work with the health care provider to certify a mutually agreeable course of
treatment to include itemized services and a defined treatment period.
In consideration for the health care provider's participation in the voluntary certification process,
the bills that are submitted, when consistent with the precertified services, will be paid so long as
they are in accordance with the PIP medical fee schedule set forth in N.J.A.C. 11:3-29.6. In
addition, having an approved treatment plan means that as long as treatment is consistent with the
plan, additional notification to CONCENTRA INTEGRATED SERVICES, INC at decision points
is not required.
Voluntary Networks
MetLife Auto & Home’s vendor, CONCENTRA INTEGRATED SERVICES, INC, has
established networks of pre-approved vendors which can be recommended designated providers
for diagnostic tests;; MRI, CT, CAT Scan, Somatosensory evoked potential (SSEP), visual evoked
potential (VEP), brain audio evoked potential (BAEP), brain evoked potential (BEP), nerve
3
�condition velocity (NCV), and H-reflex study, Electroencephalogram (EEG), needle
electromyography (needle EMG) and durable medical equipment and prescriptions costing more
than $50.00. An exception from the network requirement applies for any of the electro diagnostic
tests performed in 11:3-4.5b1-3 when done in conjunction with a needle EMG performed by the
treating provider. The designated providers are approved through a Workers Compensation
Managed Care Organization
You are encouraged, but not required, to obtain the noted service from one of the preapproved vendors. If you use a pre-approved vendor from one of these networks for medically
necessary goods or services, you will be fully reimbursed for those goods and services consistent
with the terms of your auto insurance policy. If you choose to use a vendor that is not part of
these pre-approved networks, we will provide reimbursement for medically necessary goods or
services but only up to seventy percent of the lesser of the following: (1) the charge or fee
provided for in N.J.A.C. 11:3-29, or (2) the vendor’s usual, customary and reasonable charge or
fee. The Networks can be accessed either through a referral from the Nurse Case Manager or by
contacting
The Atlantic Imaging Group - Diagnostic testing 888-340-5850
Progressive Medical – Durable Medical Equipment and Prescriptions 800-777-3574
Concentra has PPO Networks available that include providers in all specialties, hospitals,
outpatient facilities, and urgent care centers throughout the entire State. The Nurse Case Manager
can provide a current PPO network list. The use of these networks is strictly voluntary and the
choice of health care provider is always made by the injured party. The PPO networks are
provided as a service to those persons who do not have a preferred health care provider by giving
them recommendations of providers that they may select from. Networks include CHN Solutions
and Focus NJ Chiropractic.
Internal Appeals Process
If a Decision Point Review request or a request to precertify any medical treatment, tests, durable
medical equipment or prescriptions drugs is denied, you are entitled to seek an appeal of such
decision. To access the Internal Appeals Process you must notify CIS within 30 days of the
denial. A peer to peer Standard Appeal third level review will be conducted within 5-7 business
days. An Expedited Appeal can be conducted within 1-3 business days. The Nurse Case Manager
determines the applicable appeal process based on medical need. Appeals should be submitted to
CONCENTRA INTEGRATED SERVICES, INC, P.O. Box 5038, Woodbridge, NJ 07095 or
faxed to (732) 734-2587. An appeal can also be communicated to the Nurse Case Manager via
telephone. Either party can appeal to an Alternate Dispute Resolution Organization as provided
for in N.J.A.C. 11:3-5 if the issue can not be resolved through the Internal Appeals Process.
Assignment of Benefits
Assignment of your rights to receive benefits for medically necessary treatment, testing, durable
medical equipment or prescription drugs or other services are prohibited except to a licensed
health care provider who agrees to fully comply with our Decision Point Review Plan. If the
provider accepts direct payment of benefits, the provider must hold harmless the insured and/or
4
�eligible injured person for any deduction or declination in benefits caused by the provider’s failure
to comply with the terms of the policy and the treating provider agrees to submit disputes to
Alternate Dispute Resolution Organization as provided for in N.J.A.C. 11:3-5. The assignment is
limited by statute and regulation to a licensed health care provider who complies with the
restrictive language contained within the MetLife Auto & Home’s insurance policy.
Medical Examinations
At our request, we may require a medical examination (IME) to determine medical necessity of
further treatment or testing. The appointment will be made within 7 calendar days of receipt of
the
notice that an IME is required unless the injured person agrees to extend the time period. The
IME
will be completed by a provider in the same discipline as the treating provider and upon request
the injured person must provide medical records and other pertinent information to the provider
conducting the IME. The IME will be conducted at a location reasonably convenient to the
insured and/or eligible injured party. Within three business days following the examination the
injured party and provider will be notified as to whether they will be reimbursed for further
treatment. The injured party or his designee may request a copy of any written report prepared in
conjunction with any physical examination we request. If there are two or more unexcused
failures to attend the scheduled exam, notification will be immediately sent to the Named Insured
and/or Eligible Injured Person, Attorney if noted and all health care providers providing treatment
for the diagnosis (and related diagnosis) contained in the attending physician's treatment plan
form. The notification will place the parties on notice that all future treatment, diagnostic testing,
durable medical equipment or prescription drugs required for the diagnosis (and related diagnosis)
contained in the attending physician's treatment plan form will not be reimbursable as a
consequence for failure to comply with the plan. Treatment may proceed while the IME is being
scheduled and until the results become available.
Sincerely,
Nurse Case Managers Name
Nurse Case Managers Telephone number with extention
5
�
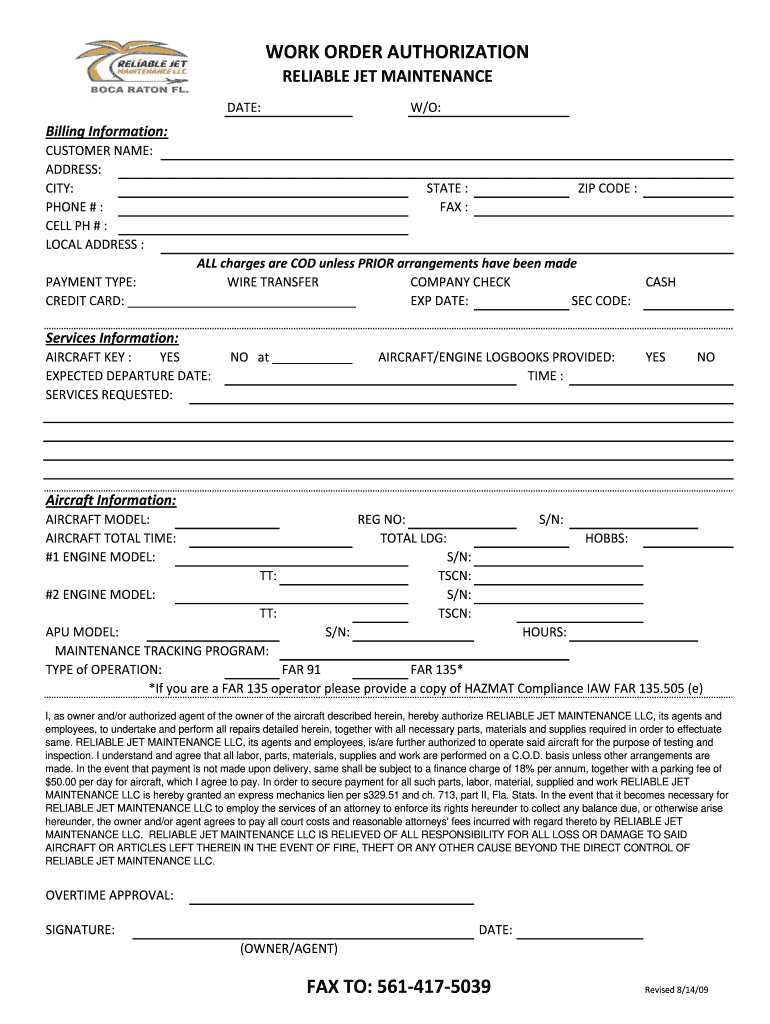
Practical advice on preparing your ‘Authorization Work Order Form’ online
Are you exhausted by the burden of handling paperwork? Look no further than airSlate SignNow, the premier electronic signature tool for individuals and small to medium-sized businesses. Bid farewell to the lengthy process of printing and scanning documents. With airSlate SignNow, you can seamlessly complete and sign paperwork online. Take advantage of the robust features integrated into this user-friendly and cost-effective platform and transform your method of document management. Whether you need to authorize forms or collect signatures, airSlate SignNow manages it all effortlessly, requiring just a few clicks.
Follow this comprehensive guide:
- Log into your account or sign up for a complimentary trial with our service.
- Click +Create to upload a file from your device, cloud, or our form library.
- Open your ‘Authorization Work Order Form’ in the editor.
- Click Me (Fill Out Now) to finalize the document on your end.
- Include and assign fillable fields for others (if necessary).
- Continue with the Send Invite settings to request eSignatures from others.
- Save, print your version, or transform it into a reusable template.
Don’t be concerned if you need to collaborate with your colleagues on your Authorization Work Order Form or send it for notarization—our solution offers everything necessary to achieve such objectives. Create an account with airSlate SignNow today and take your document management to new heights!