U.S. Department of Health and Human Services
Food and Drug Administration
Center for Drug Evaluation Research
Office of Pharmacoepidemiology and Statistical Science
Office of Biostatistics
STATISTICAL REVIEW AND EVALUATION
CLINICAL STUDIES
NDA /Serial Number:
21-661/N000
Drug Name :
RSR13 (efaproxiral) Injection (75 or 100 mg/kg)
Applicant:
Allos Therapeutics Inc.
Indication(s):
Brain metastases
Date(s):
Submission Date: December 4, 2003
PDUFA Date: June 4, 2004
ODAC Meeting Date: May 3, 2004
Review Completion Date:
Review Priority:
Priority
Biometrics Division:
Division of Biometrics I (HFD-710)
Statistical Reviewer:
Rajeshwari Sridhara, Ph.D.
Concurring Reviewer:
Kooros Mahjoob, Ph.D., Acting Director
Medical Division:
Oncology Drug Products (HFD-150)
Clinical Team:
Kevin Ridenhour, M.D. & Ramzi Dagher, M.D.
Project Manager:
Ms. Christy Cottrell
Keywords:
Active control/superiority, log-rank test, post-hoc
analysis, subgroup analyses, multiple endpoints,
multiple comparisons, Cox regression
�Table of Contents
1
Executive Summary ....................................................................................... 1
1.1 Conclusions and Recommendations....................................................... 1
1.2 Brief Overview of Clinical Studies......................................................... 1
1.3 Statistical Issues and Findings................................................................ 1
2 Introduction .................................................................................................... 4
2.1 Overview................................................................................................... 4
2.1.1 Background ......................................................................................... 4
2.1.2 Major Statistical Issues ....................................................................... 5
2.2 Data Sources............................................................................................. 5
3 Statistical Evaluation ..................................................................................... 6
3.1 Evaluation of Efficacy ............................................................................. 6
3.1.1 Study RT009 ....................................................................................... 6
3.1.1.1 Study Design ................................................................................ 6
3.1.1.2 Treatment Administration ............................................................ 8
3.1.1.3 Study Objectives........................................................................... 9
3.1.1.4 Efficacy Endpoints ....................................................................... 9
3.1.1.5 Sample Size Considerations ....................................................... 10
3.1.1.6 Interim Analysis ......................................................................... 11
3.1.1.7 Efficacy Analysis Methods ........................................................ 12
3.1.1.8 Sponsor’s Results and Statistical Reviewer’s Findings/
Comments ................................................................................................... 14
3.1.1.8.1 Baseline Characteristics......................................................... 15
3.1.1.8.2 Primary Efficacy Analyses .................................................... 18
3.1.1.8.3 Exploratory Covariate Adjusted and Subgroup Survival
Analyses 21
3.1.1.8.4 Secondary Efficacy Analyses ................................................ 31
3.2 Evaluation of Safety............................................................................... 33
4 Findings in Special/Subgroup Populations ................................................ 33
4.1 Gender, Race and Age........................................................................... 33
4.2 Other Special/Subgroup Populations................................................... 35
5 Summary and Conclusions .......................................................................... 36
5.1 Statistical Issues and Collective Evidence ........................................... 36
5.2 Conclusions and Recommendations..................................................... 37
APPENDICES ..................................................................................................... 38
Appendix 1: List of Ineligible Patients ......................................................... 38
Appendix 2: List of Patients Who Were Misclassified at Randomization 39
Appendix 3: List of Patients Who Were In-evaluable (Withdrew from
Study Prior to Treatment) .............................................................................. 40
Appendix 4: Survival Analysis Before Addition of Co-primary Hypothesis
........................................................................................................................... 41
Appendix 5: Interim Analysis Results .......................................................... 42
�Appendix 6: Exploratory Covariate Adjusted Survival Analyses in
NSCLC/Breast Primary .................................................................................. 43
Appendix 7: Exploratory Covariate Adjusted Survival Analysis in Breast
Primary ............................................................................................................. 44
ii
�1
1.1
Executive Summary
Conclusions and Recommendations
In this reviewer's opinion the registration study failed to demonstrate improved
survival of RSR13 + whole brain radiation therapy (WBRT) over WBRT alone
for patients with brain metastases. It is not evident that the apparent survival
advantage observed in a single small subgroup of patients with primary breast
cancer based on post-hoc analysis is attributable solely to the treatment effect and
not due to imbalances in known and unknown prognostic factors. Therefore, the
evidence submitted in this application based on results from a single trial, is not
convincing and does not support the sponsor’s claim of efficacy in a subgroup of
patients with breast cancer primary.
1.2
Brief Overview of Clinical Studies
The sponsor has submitted results from one phase III, comparative clinical trial
(registration trial Study RT009) comparing WBRT alone to RSR13 + WBRT, to
demonstrate efficacy of RSR13. The sponsor has also provided supportive
efficacy data from a phase II, single arm study (Study RT008). The main focus of
this review is on results from Study RT009.
Study RT009 was a multicenter international study conducted in patients with
brain metastases. This study was initiated on February 16, 2000 and the study
was completed on September 24, 2002. The data cut-off date for final efficacy
analysis was January 31, 2003.
Study RT009 was a phase III randomized, open-label, comparative study
conducted in 538 patients from 82 international centers, who would be receiving a
standard 2-week (10-day) course of WBRT for brain metastases. Patients were
randomized (1:1) to receive RSR13 no longer than 30 minutes prior to daily
WBRT or WBRT alone. Patients were stratified at randomization to 4 strata: (1)
Radiation Therapy Oncology Group (RTOG) recursive partitioning analysis
(RPA) Class I (including non-small cell lung, breast, and other primary cancers),
(2) RPA Class II non-small cell lung cancer (NSCLC) primary, (3) RPA Class II
breast cancer primary, and (4) RPA Class II primary tumors of various origins
(hereafter referred as other primary).
1.3
Statistical Issues and Findings
This NDA submission is to support administration of RSR13 as an adjunct to
whole brain radiation therapy (WBRT) for patients with brain metastases from
primary breast cancer. In this NDA submission, study RT009 is the only
1
�randomized pivotal study conducted for the efficacy and safety of RSR13. This
open-label study was designed to evaluate the efficacy and safety of combined
therapy with RSR13 + WBRT versus WBRT alone in patients with brain
metastases. This study enrolled a total of 538 patients with 267 patients who
received WBRT alone and 271 patients who received RSR13 + WBRT. The
primary efficacy endpoint of this study was survival.
Statistical Issues:
1. Only one randomized open-label study conducted in patients with brain
metastases, which failed to demonstrate efficacy as per the design of the
study, in the intent-to-treat population (log-rank test, P-value = 0.1688) and in
the co-primary subgroup of patients with NSCLC/Breast cancer primary (logrank test, P-value = 0.1217).
2. When the overall result fails to show efficacy, usually subgroup findings are
not acceptable and subgroup analyses at best can be exploratory or hypothesis
generating analyses (ICH E-3 guidelines, section 11.4.2.8: These analyses are
not intended to "salvage" an otherwise non-supportive study but may suggest
hypotheses worth examining in other studies or be helpful in refining labelling
information, patient selection, dose selection etc.). When one starts to do
multiple subgroups testing, one can easily make a false positive claim based
on such subgroup analysis. We do not know how to interpret the P-values
based on such post-hoc analysis. Furthermore, without replication of the
results in a second well-controlled study, the subgroup analysis can not be
ruled out for a false positive result.
3. The sponsor wishes to claim approval based on a subgroup of patients with
primary breast cancer. This subgroup hypothesis corresponding to breast
cancer primary patients was not stated as a hypothesis of interest to be tested
in the original protocol. Any subgroup hypothesis needs to be stated in the
protocol and accordingly proper allocation of α has to be specified.
Otherwise, such post-hoc subgroup claim will inflate Type I error and it is
difficult to interpret such P-values.
4. Some of the important issues not addressed by the sponsor are: imbalance in
patients who were ineligible (per protocol) between the two treatment groups;
misclassification of patients in the randomized strata; imbalance in the number
of baseline brain lesions in the subgroup of patients with primary breast
cancer.
Findings:
The protocol specified primary analysis was unadjusted log-rank test in the intentto-treat (ITT) population to compare overall survival between the two treatment
2
�arms. This study failed to demonstrate survival benefit as presented in the
following Table A.
Table A: Primary Efficacy Survival Analysis in ITT Population
Treatment
WBRT
RSR13 + WBRT
Number
of Deaths
221/267
220/271
Median Survival
in Months1
(95% C.I.)
4.5 (3.7, 5.4)
5.3 (4.5, 6.2)
Hazard
Ratio 2
(95% C.I.)
0.877
(0.727, 1.057)
P-value 3
0.1688
1
: Kaplan-Meier Estimates; 2: Hazard Ratio of RSR13 + WBRT/ WBRT; 3: unadjusted log-rank
test.
The sponsor amended the protocol during the course of study to include a coprimary hypothesis, to test survival difference between the two treatment arms in
a subgroup of patients with NSCLC or Breast primary cancer. The results of
these comparisons also failed to demonstrate survival benefit as presented in
Table B below.
Table B: Co-Primary Efficacy Survival Analysis in NSCLC/Breast Primary
Cancer Subgroup*
Treatment
WBRT
RSR13 + WBRT
Number
of Deaths
167/206
164/208
Median Survival
in Months1
(95% C.I.)
4.5 (3.8, 5.4)
5.9 (4.7, 7.0)
Hazard
Ratio 2
(95% C.I.)
0.844
(0.680, 1.048)
P-value 3
0.1217
*: Corrected for miss-classification (i.e., non-randomized subgroup); 1: Kaplan-Meier Estimates;
2
: Hazard Ratio of RSR13 + WBRT/ WBRT; 3: unadjusted log-rank test.
The sponsor is seeking approval based on post-hoc analysis in a small subgroup
of 115 patients with Breast cancer primary. The results of these comparisons are
presented in the following Table C.
Table C: Exploratory Survival Analysis in the Subgroup of Patients with
Primary Breast Cancer*
Treatment
WBRT
RSR13 + WBRT
Number
of Deaths
47/55
39/60
Median Survival
in Months1
(95% C.I.)
4.6 (3.8, 6.2)
8.7 (6.0, 11.3)
Hazard
Ratio 2
(95% C.I.)
0.552
(0.359, 0.850)
P-value 3
0.0061
*: Corrected for miss-classification (i.e., non-randomized subgroup);
: Kaplan-Meier Estimates; 2: Hazard Ratio of RSR13 + WBRT/ WBRT;
3
: unadjusted log-rank test and not adjusted for multiple analyses.
1
3
�2
Introduction
2.1
Overview
It has been estimated that in the United States 80,000 to 170,000 patients develop
brain metastases each year. Standard palliative treatment for symptomatic lesions
consists of corticosteroids and whole brain radiation therapy (WBRT). Analysis
of a large database compiled by the Radiation Therapy Oncology Group (RTOG)
indicates that the overall prognosis of patients with brain metastasis is poor with
median survival time of 4-7 months.
2.1.1
Background
RSR13 is a synthetic allosteric modifier of hemoglobin. RSR13 emulates the
function of natural allosteric modifiers such as 2,3-diphosphoglycerate (2,3DPG). RSR13 is a small molecule that reduces hemoglobin-oxygen binding
affinity, described by an increase in p50 (the partial pressure of oxygen [pO2] that
results in 50% hemoglobin saturation), and enhances the diffusion of oxygen from
the blood to the tissues.
Radiation therapy is currently the principal non-surgical therapy to achieve local
control of brain metastases from solid tumors. However, the efficacy of radiation
therapy (RT) is modified by the extent of tumor oxygenation. Hypoxic tumors are
more resistant to cell damage by radiation and tumor hypoxia adversely affects
the clinical prognosis of RT. It has been reported in literature that tumors with a
low median pO 2 have a higher in-field failure rate after RT.
Animal pharmacology studies have shown that RSR13 increases blood p50,
increases pO2 in non-tumor and tumor tissue, and increases oxygen diffusive
transport in non-tumor tissue. The effect of RSR13 on hemoglobin in the red
blood cell to enhance oxygen unloading from hemoglobin, and the diffusion of
that oxygen from the vascular compartment into the hypoxic tumor cells is the
basis for the radioenhancement effect of RSR13. RSR13 does not need to diffuse
into the brain tissue, because oxygen readily diffuses across the blood brain
barrier and the cancer cell membrane to increase tumor oxygenation, thereby
increasing the effectiveness of RT. The goal of adjunctive RSR13 therapy in
cancer patients is to increase tumor O 2 concentration thereby maximizing the
cytotoxicity of the treatment modality (RT and/or chemotherapy).
The sponsor has submitted results from one phase III, randomized, controlled,
open-label clinical trial (registration trial Study RT009) comparing WBRT alone
to RSR13 + WBRT, to demonstrate efficacy of RSR13. The sponsor has also
4
�provided supportive efficacy data from a phase II, single arm study (Study
RT008). The main focus of this review will be on results from Study RT009.
2.1.2
Major Statistical Issues
1. Only one randomized open-label study conducted in patients with brain
metastases, which failed to demonstrate efficacy as per the design of the
study, in the intent-to-treat population (log-rank test, P-value = 0.1688)
and in the co-primary subgroup of patients with NSCLC/Breast cancer
primary (log-rank test, P-value = 0.1217).
2. When the overall result fails to show efficacy, usually subgroup findings
are not acceptable and subgroup analyses at best can be exploratory or
hypothesis generating analyses (ICH E-3 guidelines, section 11.4.2.8:
These analyses are not intended to "salvage" an otherwise non-supportive
study but may suggest hypotheses worth examining in other studies or be
helpful in refining labelling information, patient selection, dose selection
etc.). When one starts to do multiple subgroups testing, one can easily
make a false positive claim based on such subgroup analysis. We do not
know how to interpret the P-values based on such post-hoc analysis.
Furthermore, without replication of the results in a second well-controlled
study, the subgroup analysis can not be ruled out for a false positive result.
3. The sponsor wishes to claim approval based on a subgroup of patients
with primary breast cancer. This subgroup hypothesis corresponding to
breast cancer primary patients was not stated as a hypothesis of interest to
be tested in the original protocol. Any subgroup hypothesis needs to be
stated in the protocol and accordingly proper allocation of α has to be
specified. Otherwise, such post-hoc subgroup claim will inflate Type I
error and it is difficult to interpret such P-values.
4. Some of the important issues not addressed by the sponsor are: imbalance
in patients who were ineligible (per protocol) between the two treatment
groups; misclassification of patients in the randomized strata; imbalance in
the number of baseline brain lesions.
2.2
Data Sources
Data used for review is from the electronic submission received on 12/3/03. The
network path is \\Cdsesub1\n21661\N_000\2003-12-03\crt\datasets. Specifically,
datasets from Study 009 were reviewed (\\Cdsesub1\n21661\N_000\2003-1203\crt\datasets\rt009).
5
�3
Statistical Evaluation
3.1
Evaluation of Efficacy
The sponsor has submitted efficacy results from the following two studies:
a) Study RT008: A phase II non-randomized, open-label single arm study
conducted in 69 patients from 17 centers (16 US, 1 Canada), to evaluate
the safety and efficacy of RSR13 with WBRT in patients with brain
metastases.
b) Study RT009: A phase III randomized, open-label, comparative study
conducted in 538 patients from 82 centers (40 US, 15 Canada, 4 Australia,
4 Hungary, 3 Belgium, 3 France, 3 Germany, 3 Israel, 2 Italy, 2 Scotland,
2 Spain and 1 UK), to evaluate safety and efficacy of RSR13 with WBRT
compared to WBRT alone in patients with brain metastases.
Reviewer’s Comment:
Study RT008 is a non-randomized, single arm, open-label study and as such can
not evaluate efficacy based on overall survival. Therefore, this review will focus
only on the randomized Study RT009 and particularly on the efficacy aspect of
this study. Please refer to the clinical review of this application for the evaluation
of Study RT008.
3.1.1
Study RT009
Study RT009 was a multicenter international study conducted in patients with
brain metastases. This study was initiated on February 16, 2000 and the study
was completed on September 24, 2002. The data cut-off date for final efficacy
analysis was January 31, 2003.
3.1.1.1 Study Design
Study RT009 was a phase III, randomized, open-label, comparative study in
patients who would be receiving a standard 2-week (10-day) course of WBRT for
brain metastases. Patients were randomized (1:1) to receive RSR13 no longer
than 30 minutes prior to daily WBRT or WBRT alone. Patients were stratified at
randomization to 4 strata: (1) Radiation Therapy Oncology Group (RTOG)
recursive partitioning analysis (RPA) Class I (including non-small cell lung,
breast, and other primary cancers), (2) RPA Class II non-small cell lung cancer
(NSCLC) primary, (3) RPA Class II breast cancer primary, and (4) RPA Class II
6
�primary tumors of various origins (hereafter referred as other primary). The
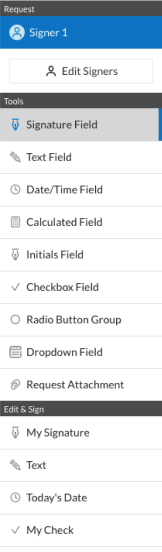
decision tree utilized in the RPA classification is illustrated in Figure 1.
Eligibility criteria included that all patients should have Karnofsky Performance
Status (KPS) = 70, radiographic studies consistent with brain metastases and a
histologically or cytologically confirmed primary malignancy. Patients with
small cell lung cancer, extrapulmonary small cell carcinomas, germ cell tumors or
lymphomas were excluded from entering the study. Patients included in the study
were not to have received prior treatment for brain metastases with WBRT,
sterotactic radiosurgery, chemotherapy, hormonal therapy, immunotherapy, or
biological agents.
All patients were to be assessed for safety from randomization until the initial
follow-up visit at 1 month after completion of the radiation therapy (RT) course.
Standard follow-up visits were required 3 months after the completion of RT
course and every 3 months thereafter until progression, and then followed for
subsequent therapies and survival.
Figure 1: RPA Classification Decision Tree
7
�Reviewer’s Comments:
1. It was clearly stated in the protocol that the randomized stratification was
purely for balance between treatment groups and therefore the number of
patients in each of the four strata would not be predetermined.
2. There were a total of 23 ineligible patients (17 patients in the WBRT alone
arm and 6 patients in the RSR13 + WBRT arm) based on eligibility
criteria at entry, who were entered into the study and treated (Please refer
to Appendix 1 for the list of ineligible patients by treatment arm). There
were greater than 2 times more patients who were ineligible in the control
arm compared to the RSR13 arm. Given the open-label nature of the
study there is concern for bias due to the apparent imbalance in ineligible
patients between the two arms.
3. There were a total of 25 patients who were miss-classified in the strata
assignment at randomization (please refer to Appendix 2 for a complete
list of miss-classified patients). This miss-classification is not an issue
when analyzing the overall intent-to-treat (ITT) population (all patients as
randomized to the two treatment groups) using unadjusted analysis.
However, this miss-classification can lead to biased results when
considering adjusted analysis because the true patient strata will no longer
be as randomized. In particular, there were 6 patients where there were
major miss-classifications: 2 patients who were randomized as RPA II,
breast cancer were later re-classified as RPA II, NSCLC; 1 patient who
was randomized as NSCLC was later re-classified as RPA II, other; and 3
patients who were randomized as RPA II, other were later re-classified as
RPA II, NSCLC.
3.1.1.2 Treatment Administration
Daily administration of RSR13 required placement of a central venous access
device (CVAD). RSR13 treatment arm patients received supplemental oxygen
(4L/min via nasal cannula) beginning 5 minutes prior to initiation of infusion,
during infusion and WBRT, and for at least 15 minutes after completion of daily
WBRT. Patients in the control arm of the study did not receive a placebo.
Starting dose and dosing adjustment thereafter of RSR13 was based on gender,
weight and oxygen saturation measured by standard pulse oximetry (SpO 2).
Starting dose of RSR13 in this study was 75 or 100 mg/kg. The dosing
instructions were amended 2 times during the course of the study. Patients with
SpO2 while breathing room air on any WBRT day < 90% were not treated with
RSR13. Before the second amendment, if SpO2 while breathing room air at
screening (at rest and during exercise) and on WBRT day 1 was = 93% then
RSR13 100mg/kg was administered. If SpO2 while breathing room air at
screening (at rest and during exercise) and on WBRT day 1 was 90-92% then
8
�RSR13 75mg/kg was administered. After the second protocol amendment, if
SpO2 while breathing room air at screening (at rest and during exercise) and on
WBRT day 1 was = 93% then RSR13 was administered based on gender and
weight as follows: (a) Males (i) if weight = 95kg then 100 mg/kg; (ii) if weight >
95kg then 75 mg/kg, and (b) Females (i) if weight = 70kg then 100 mg/kg; (ii) if
weight > 70kg then 75 mg/kg.
Reviewer’s comment:
The dosing regimen was changed during the course of study based on weight and
gender. Therefore it will be difficult to determine the optimum dose that is
efficacious based on the results of this study.
3.1.1.3 Study Objectives
The study objectives were: (1) to determi ne the effect of RSR13 on primary and
secondary efficacy endpoints in patients with brain metastases receiving daily IV
doses of RSR13 administered immediately prior to standard whole brain radiation
therapy compared to patients receiving standard whole brain radiation therapy
alone, and (2) to determine the safety of RSR13 in this patient population.
3.1.1.4 Efficacy Endpoints
Primary Efficacy Endpoint of this study was survival. Secondary Efficacy
Endpoints included time to radiographic and time to clinical tumor progression in
the brain, response rate in the brain, cause of death, and quality of life.
Reviewer’s Comment:
In the original protocol (Jan 10, 2000), efficacy was to be established based on the
primary endpoint of survival in the intent-to-treat total population. Subsequently
in amendment 2 (June 5, 2001) per sponsor after enrollment of a total of 222
patients (172 patients in the NSCLC/breast primary subgroup), the protocol was
amended to include a co-primary analysis in the subgroup of patients with
NSCLC and breast primary cancer. This reviewer’s analysis suggested that by
June 5, 2001 there were a total of 173 patients (134 patients in NSCLC/Breast
primary subgroup) enrolled into the study (Appendix 4). The only reasoning
given by the sponsor to include this subgroup as a co-primary was that the group
9
�of patients with NSCLC/breast primary tumors comprised a large and
homogenous subpopulation of patients. Given the open-label nature of this study
such additions of primary hypotheses are of concern.
3.1.1.5 Sample Size Considerations
In the original protocol (Jan 10, 2000), a sample size requirement of a total of 408
eligible patients was estimated based on the following assumptions: a mix of 20%
RPA class I and 80% RPA class II patients, median survival in WBRT to be 4.57
months, an expected 35% increase in median survival in WBRT with RSR13
(median survival of 6.17 months), 18 months of accrual, a shape parameter of
0.20, and 80% power to detect the difference in survival at two-sided overall
significance level of 0.05. It was estimated that a total of 308 deaths from both
arms would be required to detect the survival difference in the overall ITT
population. It was expected that there might be 5% ineligible patients and
therefore a total of 408 patients were required to be entered on the study.
This sample size calculation was amended in amendment 2 (June 5, 2001) as
follows: The sample size was increased to a total of 501 patients in order to
observe 402 deaths by increasing the power of the study to detect the survival
difference (median survival 4.57 months versus 6.17 months in the overall ITT
population) to 85%, increasing accrual time to 27 months, and changing the shape
parameter to zero (O’Brien and Fleming). In this amendment the sponsor also
added a co-primary analysis in the subgroup of patients with NSCLC/breast
primary tumors. It was stated that in this subgroup a total of 308 deaths will be
required to provide a power of 75% with a two-sided significance level of 0.05.
Furthermore, in this amendment it was stated that the expected number of patients
to be enrolled into the study would be between 501-538 patients, depending on
the percentage of patients with ‘other’ as a primary cancer. If 25% of enrolled
patients had ‘other’ primary, then a total of 501 patients would be enrolled; if
30% of enrolled patients had ‘other’ primary, then a total of 538 patients would be
enrolled.
Reviewer’s Comments:
1. Reason for changing the space parameter was not specified in the
amendment.
2. There was no specific scientific reason given to include a co-primary in
the subgroup of patients with NSCLC/breast primary other than that this
was a large, homogenous subgroup.
3. A total of 538 patients were enrolled in this study. Only 23% of the
patients had ‘other’ primary tumors.
10
�3.1.1.6 Interim Analysis
In the original protocol (Jan 10, 2000) it was stated that, one interim analysis of
the primary study endpoint (overall survival), would be conducted. The interim
analysis was planned to be performed when 50% of expected events (154 deaths)
occurred.
In the first amendment of the protocol (Mar 2, 2000) the section on interim
analysis was revised to state that a stochastic analysis would be performed at the
time of interim analysis and reported to Data Safety Monitoring Committee
(DSMC). It was also stated in this amendment that if the significance level of the
log-rank test between treatment arms was less than 0.0077 then the null
hypothesis would be rejected. Additionally, if the stochastic analysis indicated
less than 15% power to observe the alternative hypothesis, then enrollment to the
study may be recommended to be stopped.
In the second amendment of the protocol (June 5, 2001), this section was again
revised. It stated that interim status and safely reports will be prepared for the
independent DSMC every 6 months until planned study enrollment was achieved.
Furthermore, with the revised increase in sample size, the interim analysis for
efficacy was to be conducted when 50% events (201 deaths) had occurred in the
total patient population. The results of interim analysis would be reported to the
DSMC. If the significance level of the log-rank test between treatment arms was
less than 0.0052 then the null hypothesis would be rejected and the DSMC might
recommend stopping enrollment to the study. On the other hand if the analysis
indicated less than 15% power to observe the alternative hypothesis, then also it
may be recommended to stop further accrual.
Reviewer’s Comment:
It appears that one interim efficacy analysis was conducted (March 22, 2002).
Specific results of this interim analysis or DSMC meeting minutes deliberating on
interim efficacy results have not been submitted (Refer to Appendix 5 for FDA
analysis). Because of this interim analysis, the significance level for testing at the
time of final analysis needs to be adjusted to maintain an overall family-wise level
of significance of 0.05.
11
�3.1.1.7 Efficacy Analysis Methods
Primary Efficacy Analysis:
In the original protocol (dated Jan 10, 2000), it was specified that the primary
endpoint, overall survival, measured from the time of randomization into the
study, would be compared between treatment arms by unadjusted log-rank test.
The median survival time would be estimated in both treatment arms. Other
specific point estimates of clinical interest for each treatment were 6-month and 1year survival. It was stated that additional subgroup analyses would be performed
if there were sufficient numbers of patients across subgroups. RPA class, site of
primary cancer, and other important covariates such as primary tumor control,
age, presence of extracranial metastases, baseline KPS, and number of metastatic
lesions, would be included in a multivariate Cox model along with treatment arm
to test the relative importance of these factors for survival.
In the first amendment of the protocol (dated March 2, 2000), it was specified that
the primary final analysis of the study would be undertaken when all patients have
been potentially followed for a minimum of 6 months and the planned number of
deaths (308) had been observed. The primary analysis would be conducted on an
intent-to-treat patient population using log-rank statistic (unadjusted for
covariates) and evaluable subgroup analyses might be performed to provide
supportive evidence of efficacy.
In the second (dated June 5, 2001, sample size increased, co-primary added) and
third (dated October 9, 2001) amendments of the protocol, it was specified that
the primary final analysis would be undertaken when the planned number of
deaths in both the total study population (402) and the NSCLC/breast
subpopulation (308) had been observed. The primary analysis would be
conducted on an intent-to-treat basis and evaluable subgroup analyses might be
performed to provide supportive evidence of efficacy. Furthermore, it was stated
that a modified Bonferroni adjustment for multiple comparisons (co-primary
analyses) would be made. The adjusted significance level for the final analysis
after accounting for one interim analysis was set at 0.048.
The statistical analysis plan (SAP) which was finalized on July 29, 2002, revised
the analysis data set and specified that the analysis data set will consist of eligible
patients only. The SAP specified that: (1) patients without brain metastases,
patients with leptomenigeal metastases, patients with confirmed primaries of
small cell lung cancer, extrapulmonary small cell carcinomas, germ cell tumors
and lymphomas and (2) patients having prior treatment for brain metastases with
WBRT or stereotactic radiosurgery, and patients with prior surgical resection of
brain metastases with no remaining lesions would be ineligible and would be
excluded from analysis. The SAP also stated that the primary analysis of the
12
�overall patient population as well as the NSCLC/breast subpopulation would be
performed using the unadjusted log-rank test.
In the SAP the list of covariates that would be included in the Cox-model was
also revised. It stated that the following covariates would be included: age
(continuous as well as above and below 65 years old), baseline weight (divided by
gender as per the dosing guidelines of amendment 2), number of cranial
metastases (1, 2-3, 4 or more), baseline cranial tumor total area, gender, RPA
class, site of primary cancer, primary tumor control, number of extracranial
metastases (0, 1-2, 3 or more), presence of liver metastases, usage of subsequent
treatment (systemic vs. non-systemic, any vs. none), baseline KPS, diagnosis
timing (definition to follow), prior treatment for cranial metastases (yes/no; prior
treatment may delay time from diagnosis to radiation therapy), worldwide
location (USA vs. Canada vs. others, North America vs. Others), altitude, baseline
hemoglobin, and size of center. Center size was the binary variable designating a
center as large or small. Under the section on covariates, the SAP also stated that
‘While designated prospectively, supporting analyses should be considered
exploratory in nature, and inferences made based on p-values should be done so
with caution. Primary reasons for exploratory analyses are for estimation rather
than hypothesis testing’.
Secondary Efficacy Analyses:
The protocol has specified that the secondary endpoints, time to radiographic
tumor progression in brain and time to clinical tumor progression in the brain,
would be analyzed using cumulative incidence model and that the treatment arms
would be compared using the method of Pepe. It is also stated that analyses
within strata, within other prognostic groups and Cox model analysis would also
be performed.
Secondary endpoint response rate (best maximal response) in the brain would be
determined from MRI or CT scans and the frequency distribution of
CR:PR:SD:PD would be compared for each treatment arm. Between treatment
arms comparison would be made using Cochran-Mantel Haenzel test.
Regarding secondary endpoint cause of death, frequency of neurologic/ nonneurologic/ undistinguishable deaths would be computed for each treatment arm
and compared between treatment arms using Cochran-Mantel Haenzel test.
Secondary endpoint of quality of life would be determined by the Spitzer
Questionnaire and KPS assessment. The frequency distribution would be
computed for each treatment arm by time of follow-up.
13
�Reviewer’s Comments:
1. In the original protocol and in its amendments it was clearly stated that the
primary analysis would be conducted in ITT population. The sample size
and the power considerations were in fact based on ITT population.
2. The co-primary hypothesis testing in the NSCLC/Breast subgroup was
added during the course of study. The protocol did not clearly define this
subgroup, i.e., whether patients from strata 2 and 3 only to be included in
this subgroup or include NSCLC/Breast primary patients in strata 1, and
strata 2 and 3.
3. In using Modified Bonferroni adjustment for co-primary analysis one
could consider 2 methods of adjustment after accounting for one interim
analysis: (1) compare larger of the 2 p-values with 0.048, (a) if the larger
p-value is < 0.048, then reject both hypotheses, or (b) if the larger p-value
is > 0.048, then compare the smaller of the two p-values with 0.024
(Hochberg’s SU modified Bonferroni procedure), or (2) the second
procedure (Holm’s SD modified Bonferroni) is (a) if the smaller of the
two p-values is > 0.024, then both hypotheses are not significant, or (b) if
the smaller of the p-value < 0.024 then the corresponding hypothesis is
significant and then test if the larger of the p-value is < 0.048.
4. In the original protocol and in its amendments as well as in the SAP, it
was clearly stated that the primary analysis would be based on unadjusted
log-rank test.
5. The SAP was finalized after all the patients were entered into the study
(last 3 patients were entered on July 29, 2002). Given the open-label
nature of the study it is of concern that the analysis population was
changed after all patients were entered into the study.
6. Overall there were 23 patients who were ineligible, 17 in the control arm
and 6 in the RSR13 arm. With greater than 2 times more patients who
were ineligible in the control arm, given the study was an open-label
study, there is concern for bias.
7. There was no justification provided for the inclusion of additional several
covariates for the exploratory Cox analysis in the SAP.
8. The covariate ‘diagnosis timing’ was not defined.
9. Because no apriori probability of type I error allocation has been specified,
analyses of secondary efficacy endpoints can only be considered as
exploratory and supportive to primary efficacy analysis.
3.1.1.8 Sponsor’s Results and Statistical Reviewer’s Findings/ Comments
In the RT009 study, a total of 538 patients were randomized to receive WBRT
alone (267 patients) or RSR13 followed by WBRT (271 patients).
14
�3.1.1.8.1 Baseline Characteristics
Table 1 lists the number of patients entered in each of the randomized strata. The
baseline Characteristics of the overall population and NSCLC/Breast subgroup
are presented in Tables 3 & 4.
Reviewer’s Comments:
1. There were 25 patients who were miss-classified at randomization
according to the sponsor / CRF. Therefore the corrected numbers in each
of the strata are presented in Table 2.
2. It should be noted that the patients as listed in each strata in Table 2 are no
longer as randomized.
3. This miss-classification may not affect analysis based on ITT population.
However analyses based on subgroups could potentially lead to biased
results.
4. The sponsor has reported that 9 patients (4 in the control (WBRT) arm and
5 in the RSR13 arm) withdrew from the study prior to WBRT day 1
(Appendix 3).
5. In the overall patient population the baseline characteristics appear to be
balanced between the two treatment arms.
6. It should be noted that the NSCLC/Breast subgroup as presented in Table
3 is no longer as randomized, because: (1) NSCLC and breast cancer
patients from the Strata 1, RPA class I, are included in this subgroup, and
(2) patients who were miss-classified in the incorrect stratum at
randomization are re-classified into corrected primary tumors based on the
reported diagnosis in CRF.
Table 1: Number of Patients as Randomized in Each Stratum by Treatment
Arm
Strata
RPA Class I
RPA Class II, NSCLC
RPA Class II, Breast
RPA Class II, Other
WBRT
28 (10.5%)
132 (49.4%)
51 (19.1%)
56 (21.0%)
RSR13 + WBRT
29 (10.7%)
132 (48.7%)
52 (19.2%)
58 (21.4%)
Total
57 (10.6%)
264 (49.1%)
103 (19.1%)
114 (21.2%)
Table 2: Number of Patients as Observed in Each Stratum by Treatment
Arm
Strata
RPA Class I
RPA Class II, NSCLC
RPA Class II, Breast
RPA Class II, Other
WBRT
24 (9.0%)
136 (50.9%)
50 (18.7%)
57 (21.3%)
RSR13 + WBRT
22 (8.1%)
133 (49.1%)
56 (20.7%)
60 (22.1%)
Total
46 (8.6%)
269 (50.0%)
106 (19.7%)
117 (21.7%)
15
�Table 3: Baseline Characteristics in ITT Population
Characteristic
Gender: Female
Male
Race: Caucasian
Non-Caucasian
Age Group: < 65 years
= 65 years
Age in yrs: Mean (S.D.)
Median (Range)
Weight in Kg: Mean (S.D.)
Median (Range)
KPS Group: < 90
= 90
KPS: Mean (S.D.)
Bidirectional product (mm2) for
baseline lesions: Mean (S.D.)
Median (Range)
Resting SpO2: Mean (S.D.)
Primary Controlled : No
Yes
Extracranial metastases: 0
1
2
=3
Number of Brain Lesions: 1
2
=3
Liver Metastases: No
Yes
Lung Metastases: No
Yes
Synchronous Disease: No
Yes
Prior Brain Mets Treatment: No
Yes
Hemoglobin (g/dL): Mean (S.D.)
Creatinine (mg/dL): Mean (S.D.)
Albumin (g/dL): Mean (S.D.)
ALT (IU/L): Mean (S.D.)
Primary Site: NSCLC
Breast
Other
WBRT
150 (56.2%)
117 (43.8%)
239 (89.5%)
28 (10.5%)
197 (73.8%)
70 (26.2%)
57.0 (11.0)
57 (23 – 81)
72.5 (17.1)
70.5 (33 – 140.9)
124 (46.4%)
143 (53.6%)
85.2 (9.7)
WBRT + RSR13
153 (56.5%)
118 (43.5%)
242 (89.3%)
29 (10.7%)
196 (72.3%)
75 (27.7%)
57.1 (11.1)
57 (30 -87)
71.3 (15.0)
71.0 (39.8 – 122)
113 (41.7%)
158 (58.3%)
85.1 (9.7)
760.8 (694.8)
587.5 (4, 4200)
96.8 (1.7)
200 (74.9%)
67 (25.1%)
96 (36.0%)
69 (25.8%)
55 (20.6%)
47 (17.6%)
53 (20.2%)
81 (30.9%)
128 (48.9%)
225 (84.3%)
42 (15.7%)
183 (68.5%)
84 (31.5%)
184 (68.9%)
83 (31.1%)
238 (89.1%)
29 (10.9%)
13.5 (1.5)
0.79 (0.23)
3.70 (0.45)
40.9 (34.2)
151 (56.5%)
55 (20.6%)
61 (22.9%)
753.6 (735)
518 (16, 5080)
96.7 (1.8)
199 (73.4%)
72 (26.6%)
84 (31.0%)
72 (26.6%)
56 (20.7%)
59 (21.7%)
45 (16.9%)
82 (30.7%)
140 (52.4%)
217 (80.1%)
54 (19.9%)
179 (66.1%)
92 (33.9%)
183 (67.5%)
88 (32.5%)
250 (92.3%)
21 (7.7%)
13.3 (1.5)
0.76 (0.21)
3.65 (0.47
40.5 (49.4)
148 (54.6%)
60 (22.1%)
63 (23.3%)
16
�Table 4: Baseline Characteristics in NSCLC/Breast* Subgroup
Characteristic
WBRT
WBRT + RSR13
Gender: Female
130 (63.1%)
128 (61.5%)
Male
76 (36.9%)
80 (38.5%)
Race: Caucasian
184 (89.3%)
184 (88.5%)
Non-Caucasian
22 (10.7%)
24 (11.5%)
Age Group: < 65 years
150 (72.8%)
150 (72.1%)
= 65 years
56 (27.2%)
58 (27.9%)
Age in yrs: Mean (S.D.)
57.1 (11.2)
56.9 (11.0)
Median (Range)
57 (26 – 81)
57 (31 – 80)
Weight in Kg: Mean (S.D.)
70.7 (15.9)
71.1 (15.0)
Median (Range)
68.8 (33 – 124.1)
69.6 (41.1 – 122)
KPS Group: < 90
89 (43.2%)
87 (41.8%)
= 90
117 (56.8%)
121 (58.2%)
KPS: Mean (S.D.)
85.7 (9.5)
85.1 (9.6)
2
Bidirectional product (mm ) for
baseline lesions: Mean (S.D.)
755.6 (668.2)
767.8 (767.8)
Median (Range)
573.5 (17 – 3806)
459 (16 – 5080)
Resting SpO2: Mean (S.D.)
96.9 (1.7)
96.8 (1.8)
Primary Controlled : No
156 (75.7%)
159 (76.4%)
Yes
50 (24.3%)
49 (23.6%)
Extracranial metastases: 0
76 (36.9%)
75 (36.0%)
1
51 (24.8%)
54 (26.0%))
2
42 (20.4%)
42 (20.2%)
=3
37 (18.0%)
37 (17.8%)
Number of Brain Lesions: 1
43 (21.1%)
37 (18.0%)
2
60 (29.4%)
66 (32.2%)
=3
101 (49.5%)
102 (49.8%)
Liver Metastases: No
176 (85.4%)
176 (84.6%)
Yes
30 (14.6%)
32 (15.4%)
Lung Metastases: No
148 (71.8%)
155 (74.5%)
Yes
58 (28.2%)
53 (25.5%)
Synchronous Disease: No
140 (68.0%)
133 (63.9%)
Yes
66 (32.0%)
75 (36.1%)
Prior Brain Mets Treatment: No
189 (91.8%)
197 (94.7%)
Yes
17 (8.2%)
11 (5.3%)
Hemoglobin (g/dL): Mean (S.D.)
13.4 (1.5)
13.4 (1.4)
Creatinine (mg/dL): Mean (S.D.)
0.77 (0.22)
0.75 (0.20)
Albumin (g/dL): Mean (S.D.)
3.7 (0.4)
3.6 (0.5)
ALT (IU/L): Mean (S.D.)
39.2 (33.0)
41.9 (54.4)
*: Revised group per reclassification (corrected) and including RPA Class I
patients.
17
�3.1.1.8.2 Primary Efficacy Analyses
Primary efficacy analysis per original protocol, comparing overall survival
between WBRT and RSR13 + WBRT, in the ITT population using unadjusted
log-rank test is presented in Table 5 (same as reported by the sponsor). There
were a total of 441/538 patients who had events (deaths) at the time of the final
analysis. The Kaplan-Meier curves for the ITT population are illustrated in
Figure 2. The efficacy analysis in the subgroup of NSCLC/Breast primary
patients is presented in Table 6 (same as reported by the sponsor). The KaplanMeier curves for the NSCLC/Breast subgroup is presented in Figure 3. There
were 331/414 deaths in this subgroup at the time of the final analysis.
Table 5: Primary Efficacy Survival Analysis in ITT Population
Treatment
WBRT
RSR13 + WBRT
1
3
Number
of Deaths
221/267
220/271
Median Survival
in Months1
(95% C.I.)
4.5 (3.7, 5.4)
5.3 (4.5, 6.2)
Hazard
Ratio 2
(95% C.I.)
0.877
(0.727, 1.057)
P-value 3
0.1688
: Kaplan-Meier Estimates; 2: Hazard Ratio of RSR13 + WBRT/ WBRT;
: unadjusted log-rank test.
Figure 2: Kaplan-Meier Survival Curves in the ITT Population
18
�Table 6: Co-Primary Efficacy Survival Analysis in NSCLC/Breast Primary
Cancer Subgroup*
P-value 3
Hazard
Median Survival
2
1
Ratio
in Months
(95% C.I.)
(95% C.I.)
WBRT
167/206
4.5 (3.8, 5.4)
0.844
0.1217
(0.680, 1.048)
RSR13 + WBRT
164/208
5.9 (4.7, 7.0)
*: Corrected for miss-classification (i.e., non-randomized subgroup);
1
: Kaplan-Meier Estimates; 2: Hazard Ratio of RSR13 + WBRT/ WBRT;
3
: unadjusted log-rank test.
Treatment
Number
of Deaths
Figure 3: Kaplan-Meier Survival Curves in the Subgroup of Patients with
NSCLC/Breast Primary
Reviewer’s Comments:
1. RSR13 + WBRT treatment failed to demonstrate superior survival
over WBRT alone in the randomized ITT population (Table 5 and
Figure 2 above). The final analysis was conducted after observing the
required number of deaths (required 402 deaths, observed 441 deaths)
19
�specified in the protocol. The median survival in the WBRT arm was
slightly less than what was expected in the protocol design.
2. RSR13 + WBRT treatment failed to demonstrate superior survival
over WBRT alone in the subgroup of patients with NSCLC/Breast
primary (Co-primary analysis, Table 6 and Figure 3 above). The final
analysis was conducted after observing the required number of deaths
(required 308 deaths, observed 331 deaths) specified in the protocol.
3. There appears to be an imbalance between the treatment arms in the
number of patients who were not eligible (17 in the WBRT alone arm and
6 in the RSR13 + WBRT arm). The results of exploratory analyses in
eligible patients only or per-protocol patients in the overall population and
in the NSCLC/Breast primary subgroup of patients are presented
respectively, in the following Tables 7 and 8. These results also fail to
demonstrate superior survival of RSR13 + WBRT treatment over WBRT
alone.
4. There were 30/441 early deaths within 1 month from the start of the study.
Of the 30 deaths 16 were in the WBRT alone arm (2 Breast, 11 NSCLC
and 3 Other primaries), and 14 were in the RSR13 + WBRT arm (4
Breast, 3 NSCLC and 7 Other primaries). It appears that there were more
early deaths in the control arm compared to RSR13 arm in the NSCLC
and breast primary subgroups. Given these numerical differences and
open-label nature of the study it is uncertain if bias was introduced in
patient selection and allocation.
Table 7: Exploratory Survival Analysis in the Per-Protocol Overall
Population
Treatment
Number
Median Survival
Hazard
P-value 3
of Deaths
in Months1
Ratio 2
(95% C.I.)
(95% C.I.)
WBRT
206/250
4.4 (3.7, 5.3)
0.871
0.1549
(0.719,
1.054)
RSR13 + WBRT
215/265
5.4 (4.6, 6.3)
1
: Kaplan-Meier Estimates; 2: Hazard Ratio of RSR13 + WBRT/ WBRT;
3
: unadjusted log-rank test and not adjusted for multiple analyses.
Table 8: Exploratory Survival Analysis in the Per-Protocol NSCLC/Breast
Primary Cancer Subgroup*
Treatment
Number
Median Survival
Hazard
P-value 3
of Deaths
in Months1
Ratio 2
(95% C.I.)
(95% C.I.)
WBRT
157/194
4.4 (3.7, 5.2)
0.815
0.0693
(0.654,
1.017)
RSR13 + WBRT
159/203
6.0 (4.7, 7.1)
*: Corrected for miss-classification (i.e., non-randomized subgroup);
1
: Kaplan-Meier Estimates; 2: Hazard Ratio of RSR13 + WBRT/ WBRT;
3
: unadjusted log-rank test and not adjusted for multiple analyses.
20
�3.1.1.8.3 Exploratory Covariate Adjusted and Subgroup Survival Analyses
The sponsor had specified exploratory covariate adjusted survival analyses using
Cox model. The sponsor had also specified exploratory survival analyses in each
of the randomized strata. In this section the results of these exploratory analyses
are presented.
In the original protocol and its amendments, 7 covariates were mentioned as
likely to be included in the Cox model (Refer to section 3.1.1.7, and Table 9
below). After completion of accrual this analysis was revised in the SAP to
include 18 covariates (Refer to section 3.1.1.7, and Table 9 below) in various
combinations of continuous and categorical variables resulting in 48 Cox models
(submitted by sponsor including 17/18 covariates, all models included the same
17 covariates, not presented here). Results of Cox regression analysis including
the 7 covariates specified in the protocol are presented in Table 11 (FDA
analysis). One of the models including the 18 covariates in the per-protocol
population as specified in the SAP is presented in Table 12 (FDA analysis).
Table 9: Covariates Intended to be Included in the Cox Model
Protocol Covariates
RPA Class
Site of Primary Cancer
Primary Tumor Control
Age
Presence of Extracranial Metastases
Baseline KPS
Number of Metastatic Lesions
SAP Covariates
RPA Class
Site of Primary Cancer
Primary Tumor Control
Age
Baseline KPS
Number of Cranial Metastases
Number of Extracranial Metastases
Baseline Cranial Tumor Total Area
Baseline Weight (divided by gender as per
the dosing guidelines)
Gender
Presence of Liver Metastases
Usage of Subsequent Treatment*
Diagnosis Timing
Prior Treatment to Cranial Metastases
Worldwide Location
Altitude
Baseline Hemoglobin
Size of Center
* Not included in sponsor’s adjusted Cox models
21
�Table 10: Cox’s Proportional Hazard Model Adjusting for Covariates in the
ITT Population (Protocol Planned Model)
Covariates
Hazard Ratio
95% C.I.
Treatment (RSR13 + WBRT/WBRT)
0.814
0.674, 0.984
RPA Class (1 vs. 2)
0.742
0.471, 1.168
Site of Primary Cancer: Breast (Yes vs. No)
0.568
0.423, 0.764
NSCLC (Yes vs. No)
0.861
0.682, 1.085
Primary Tumor Control (Yes vs. No)
1.310
1.006, 1.707
Age
1.014
1.005, 1.023
Presence of Extracranial Metastases (No vs. Yes)
1.138
0.800, 1.618
Baseline KPS
0.968
0.958 – 0.978
Number of Metastatic Lesions 2
1.287
1.111 – 1.490
1: P-values not adjusted for multiplicity; 2: Since all patients were supposed to
have brain metastases, for the purpose of this analysis ‘number of extracranial
metastases’ was used as the covariate in place of ‘number of metastatic lesions’.
P-value 1
0.0335
0.1973
0.0002
0.2050
0.0453
0.0022
0.4732
< 0.0001
0.0008
Table 11: Cox’s Proportional Hazard Model Adjusting for Covariates in the
Overall Eligible Patient Population (SAP Planned Model)*
Covariates
Hazard Ratio
95% C.I.
Treatment (RSR13 + WBRT/WBRT)
0.777
0.640, 0.942
RPA Class (1 vs. 2)
0.763
0.479, 1.215
Site of Primary Cancer: Breast (Yes vs. No)
0.602
0.430, 0.842
NSCLC (Yes vs. No)
0.826
0.640, 1.065
Primary Tumor Control (Yes vs. No)
1.238
0.927, 1.652
Age Group ( < 65 vs. = 65 yrs)
1.486
1.178, 1.875
Baseline KPS Group (= 90 vs. < 90)
1.564
1.283, 1.907
Number of Cranial Metastases
1.148
1.000, 1.320
Number of Extracranial Metastases
1.237
1.102, 1.389
Baseline Cranial Tumor Total Area ( 1000)
Baseline Weight Group (Low vs. High)
0.971
0.765, 1.232
Gender (Female vs. Male)
1.407
1.120, 1.767
Presence of Liver Metastases (No vs. Yes)
1.249
0.941, 1.658
Usage of Subsequent Treatment (No vs. Yes)
0.910
0.695, 1.192
Diagnosis Timing (metachronous vs. synchronous)
1.122
0.870, 1.448
Prior Treatment to Cranial Metastases (No vs. Yes)
0.450
0.302, 0.671
Worldwide Location: USA (No vs. Yes)
0.921
0.665, 1.275
Canada (No vs. Yes)
0.919
0.639, 1.322
Altitude (Low vs. High)
1.096
0.805, 1.491
Baseline Hemoglobin Group (= 12 vs. < 12 g/dL)
1.336
1.027, 1.738
Size of Center (Not a big site vs. Big site)
0.965
0.762, 1.222
*: Results based on a total of 528 patients; 1 : P-values not adjusted for multiplicity;
22
P-value1
0.0103
0.2547
0.0031
0.1409
0.1481
0.0008
< 0.0001
0.0508
0.0003
0.3418
0.8096
0.0033
0.1232
0.4937
0.3737
< 0.0001
0.6199
0.6505
0.5604
0.0308
0.7679
�Reviewer’s Comments:
1. Some of the covariates included in the model are likely to be highly
correlated. For example, RPA Classification takes into account whether
primary was controlled or not, age and whether there was metastasis in
brain only or not.
2. The models specified by the sponsor both in the protocol and in SAP are
ambiguous and questionable. In the protocol specified model, the
meaning of the covariate, number of metastatic lesions, is unclear. One
could interpret it as total number of metastases (cranial + extracranial
metastases), or number of brain lesions. Furthermore both the number of
cranial lesions, extracranial metastases, and baseline tumor area appear
like continuous variables, but in fact are categorized as zero, 1, 2 or 3.
Regarding baseline cranial tumor area, the variable included in the model
was the variable submitted by the sponsor as ‘GBDPTOT’ and the
explanation given for this variable is that it is bi-dimensional product for
baseline lesions. It is assumed in the above analysis that these are
measurements for cranial lesions only. The covariate, diagnosis timing,
was not defined in the protocol. The sponsor had used this as a categorical
variable: synchronous diagnosis or not. One could interpret it as the actual
time in days to the diagnosis of brain metastasis.
3. Scientific basis or literature citation in choosing these covariates (either in
the protocol or SAP) for the model was not provided by the sponsor. Some
of the important covariates, such as, response to steroid treatment,
systemic tumor activity, LDH, interval between primary tumor and
development of brain metastases, reported in literature as significant
prognostic factors for survival, were not included in these analyses and
data needed for such evaluation were not collected.
4. Furthermore, when appropriately adjusted for multiplicity, treatment
differences are unlikely to be significant. P-values from these exploratory
covariate analyses can not be taken at face value.
5. Results from Cox regression analyses including only the randomized strata
are presented in Tables 12-14. The treatment effect was not significant in
any of these models. Please refer to Appendix 6 for exploratory Cox
regression analyses in NSCLC/Breast Primary subgroup.
6. The sponsor did not include the covariate ‘usage of subsequent therapy’
(as specified in the final SAP) in their Cox models
23
�Table 12: Cox’s Proportional Hazard Model Adjusting for Strata (As
Randomized) in the ITT Population
Covariates
Hazard Ratio
95% C.I.
Treatment (RT + RSR vs. RT)
0.871
0.722 – 1.050
Stratum 2** = RPA Class 2, Primary Lung
1.638
1.175 – 2.284
Stratum 3** = RPA Class 2, Primary Breast
1.388
0.954 – 2.022
Stratum 4** = RPA Class 2, Primary Other
2.142
1.488 – 3.083
* P-values not adjusted for multiplicity; ** Strata as randomized (25 patients were
miss-classified)
P-value*
0.1484
0.0036
0.0870
< 0.0001
Table 13: Cox’s Proportional Hazard Model Adjusting for Re-classified
Strata in the ITT Population
Covariates
Hazard Ratio
95% C.I.
Treatment (RT + RSR vs. RT)
0.879
0.729 – 1.061
Stratum 2** = RPA Class 2, Primary Lung
1.436
1.003 – 2.056
Stratum 3** = RPA Class 2, Primary Breast
1.158
0.777 – 1.726
Stratum 4** = RPA Class 2, Primary Other
1.933
1.313 – 2.846
* P-values not adjusted for multiplicity; ** Strata as observed or intended (25
patients were re-classified)
P-value*
0.1799
0.0479
0.4714
0.0008
Table 14: Cox’s Proportional Hazard Model Adjusting for Primary Site
(Including RPA Class I and Primary Site as Observed) in the ITT Population
Covariates
Treatment (RT + RSR vs. RT)
Primary Lung
Primary Breast
* P-values not adjusted for multiplicity
Hazard Ratio
0.893
0.774
0.618
95% C.I.
0.740, 1.077
0.617, 0.969
0.466, 0.821
7. Exploratory survival analyses results in each of the primary site subgroups
(NSCLC, Breast, and Other) are presented in Tables 15-17 (results same
as reported by the sponsor) and Kaplan-Meier Curves are illustrated in
Figures 4-6.
24
P-value*
0.2362
0.0258
0.0009
�Table 15: Exploratory Survival Analysis in the Subgroup of Patients with
Primary NSCLC
P-value 3
Hazard
Median Survival
2
1
Ratio
in Months
(95% C.I.)
(95% C.I.)
WBRT
120/151
4.4 (3.5, 5.7)
0.991
0.9426
(0.771, 1.273)
RSR13 + WBRT
125/148
4.9 (4.1, 6.2)
1
: Kaplan-Meier Estimates; 2: Hazard Ratio of RSR13 + WBRT/ WBRT;
3
: unadjusted log-rank test and not adjusted for multiple analyses.
Treatment
Number
of Deaths
Figure 4: Kaplan-Meier Curves in the Subgroup of Patients with Primary
NSCLC
25
�Table 16: Exploratory Survival Analysis in the Subgroup of Patients with
Primary Breast Cancer
P-value 3
Hazard
Median Survival
2
1
Ratio
in Months
(95% C.I.)
(95% C.I.)
WBRT
47/55
4.6 (3.8, 6.2)
0.552
0.0061
(0.359, 0.850)
RSR13 + WBRT
39/60
8.7 (6.0, 11.3)
1
: Kaplan-Meier Estimates; 2: Hazard Ratio of RSR13 + WBRT/ WBRT;
3
: unadjusted log-rank test and not adjusted for multiple analyses.
Treatment
Number
of Deaths
Figure 5: Kaplan-Meier Curves in the Subgroup of Patients with Primary
Breast Cancer
26
�Table 17: Exploratory Survival Analysis in the Subgroup of Patients with
Primary ‘Other’ Cancer
P-value 3
Hazard
Median Survival
2
1
Ratio
in Months
(95% C.I.)
(95% C.I.)
WBRT
54/61
3.7 (2.5, 6.0)
1.029
0.8812
(0.708, 1.496)
RSR13 + WBRT
56/63
4.0 (2.9, 5.6)
1
: Kaplan-Meier Estimates; 2: Hazard Ratio of RSR13 + WBRT/ WBRT;
3
: unadjusted log-rank test and not adjusted for multiple analyses.
Treatment
Number
of Deaths
Figure 5: Kaplan-Meier Curves in the Subgroup of Patients with Primary
‘Other’ Cancer
8. Any subgroup analysis results are relevant only if overall study (ITT) is
positive.
9. Hypotheses testing in these subgroups, and a allocation for testing these
subgroup hypotheses were not prespecified. Therefore, the P-values
obtained in these subgroup analyses are not interpretable without a
prespecified significance level.
27
�10. There were no significant differences in the treatment effect in the
subgroups of patients with primary NSCLC or Other Cancer.
11. The apparent treatment difference observed in the subgroup of patients
with primary breast cancer can only be considered as hypothesis
generating. The efficacy claim in this non-randomized, non-prespecified
subgroup is based on post-hoc, data driven hypothesis testing in a very
small subgroup (115 patients in total) of patients from a single study.
12. Well-controlled studies are required to approve a drug (21 CFR
314.126(a): Reports of adequate and well-controlled investigations
provide the primary basis for determining whether there is "substantial
evidence" to support the claims of effectiveness for new drugs). Large,
well conducted, controlled, randomized study is required particularly
when considering single study for consideration of approval.
13. The Guidance for Industry: Providing clinical evidence of effectiveness
from human drug and biological products (May 1998) clearly states that:
‘When considering whether to rely on a single multicenter trial, it is
critical that the possibility of an incorrect outcome be considered and that
all the available data be examined for their potential to either support or
undercut reliance on a single multicenter trial’.
14. Furthermore, of the 115 patients with breast primary, 8 patients (6 in
WBRT arm and 2 in the RSR13 +WBRT arm) were not eligible patients
(did not meet the inclusion criteria), 7 patients (3 in WBRT arm and 4 in
RSR13 + WBRT arm) were misclassified, 1 patient in the control arm was
withdrawn from the study prior to receiving any treatment, 6 patients (2 in
WBRT arm, 4 in RSR13+WBRT arm) were dead within one month, and
15 patients (8 in WBRT arm, 7 in RSR13 + WBRT arm) were dead within
2 months from the start of the study. Among the patients who were
terminated early in the RSR13 arm, 1 patient received only one dose, 5
patients received 2 doses only, and 2 patients received 5 doses only.
15. There appears to be imbalance in some of the baseline patient
characteristics favoring the RSR13 + WBRT arm compared to WBRT
alone arm in the subgroup of patients with breast primary. These baseline
characteristics include, weight, performance status = 90, tumor burden, 3
or more extracranial metastases, 3 or more brain lesions, presence of lung
metastases and prior brain metastases treatment (Table 18 below, bolded
characteristics). Please refer to the clinical review of this application for
other imbalances such as, differences in oxygen administration between
the two treatment arms in the subgroup of patients with breast cancer
primary.
16. Furthermore, in the breast primary subgroup majority were younger (< 65
years old) women with metachronous diagnosis compared to the other
subgroups.
17. Without replication of the results in a second well-controlled study, the
subgroup analysis can not be ruled out for a false positive result.
28
�18. ICH E– 3, Section 11.4.2.8, clearly specifies guidelines for conducting
subgroup analyses, namely, ‘These analyses are not intended to
"salvage" an otherwise non-supportive study but may suggest
hypotheses worth examining in other studies or be helpful in refining
labelling information, patient selection, dose selection etc.’ Therefore,
(a) Examining a subgroup of patients with primary breast cancer when the
overall study is not-supportive, is not acceptable; (b) Because the
randomized strata have been modified, the subgroup under consideration
is not a randomized subgroup; (c) Apparent imbalances between the
treatment groups with respect to some of the baseline characteristics may
potentially be driving the difference in survival.
19. Although no drug has been approved for breast cancer patients with brain
metastasis, in general the approval of drugs in advanced breast cancer are
based on relatively large studies.
29
�Table 18: Baseline Characteristics in Breast* Subgroup
Characteristic
Gender: Female
Male
Race: Caucasian
Non-Caucasian
Age Group: < 65 years
= 65 years
Age in yrs: Mean (S.D.)
Median (Range)
Weight in Kg: Mean (S.D.)
Median (Range)
KPS Group: < 90
= 90
KPS: Mean (S.D.)
Bidirectional product (mm2) for
baseline lesions: Mean (S.D.)
Median (Range)
Resting SpO2 : Mean (S.D.)
Primary Controlled : No
Yes
Extracrania l metastases: 0
1
2
=3
Number of Brain Lesions: 1
2
=3
Liver Metastases: No
Yes
Lung Metastases: No
Yes
Synchronous Disease: No
Yes
Prior Brain Mets Treatment: No
Yes
Hemoglobin (g/dL): Mean (S.D.)
Creatinine (mg/dL): Mean (S.D.)
Albumin (g/dL): Mean (S.D.)
ALT (IU/L): Mean (S.D.)
WBRT
54 (98.2%)
1 (1.8%)
48 (87.3%)
7 (12.7%)
45 (81.8%)
10 (18.2%)
53.9 (11.2)
53 (30-78)
68.2 (17.5)
64 (42-124.1)
24 (43.6%)
31 (56.4%)
85.3 (9.2)
WBRT + RSR13
60 (100.0%)
0 (0.0%)
50 (83.3%)
10 (16.7%)
48 (80.0%)
12 (20.0%)
52.0 (11.6)
51 (31-80)
73.2 (14.7)
72.9 (46.5-122)
24 (40.0%)
36 (60.0%)
85.5 (9.6)
882.1 (695.1)
699 (17-3588)
97.5 (1.8)
37 (67.3%)
18 (32.7%)
8 (14.6%)
8 (14.6%)
17 (30.9%)
22 (40.0%)
5 (9.3%)
9 (16.7%)
40 (74.1%)
36 (65.5%)
19 (34.5%)
23 (41.8%)
32 (58.2%)
53 (96.4%)
2 (3.6%)
51 (92.7%)
4 (7.3%)
13.0 (1.6)
0.78 (0.28)
3.9 (0.5)
36.4 (29.5)
761.9 (705.8)
578.5 (16-2936)
96.9 (1.7)
41 (68.3%)
19 (31.7%)
7 (11.7%)
14 (23.3%)
20 (33.3%)
19 (31.7%)
13 (21.7%)
13 (21.7%)
34 (56.7%)
39 (65.0%)
21 (35.0%)
31 (51.7%)
29 (48.3%)
58 (96.7%)
2 (3.3%)
58 (96.7%)
2 (3.3%)
12.7 (1.2)
0.67 (0.12)
3.7 (0.42)
40.4 (44.9)
*: Revised group per reclassification (corrected) and including RPA Class I patients.
30
�3.1.1.8.4 Secondary Efficacy Analyses
Results submitted by the sponsor on the evaluation of secondary efficacy
endpoints will be briefly summarized in this section. The protocol specified
secondary endpoints were time to radiographic and time to clinical tumor
progression in the brain, response rate in the brain, cause of death, and quality of
life.
Time to Radiographic Tumor Progression in the Brain
Time to radiographic tumor progression, as determined by Central Radiology
Review, was estimated for all patients using cumulative incidence analysis and
Kaplan-Meier methods, and tested between treatment arms using Gray’s test.
Death in this analysis was recorded as a competing risk when it occurred prior to
diagnosis of radiographic progression.
Per sponsor’s report, there was no statistically significant difference in the
cumulative incidence of radiographic progression between the WBRT alone and
RSR13 + WBRT arms (?2 = 0.458, p-value = 0.4986). The sponsor has also
reported that there was no statistically significant difference in the cumulative
incidence of radiographic progression between the WBRT alone and RSR13 +
WBRT arms in the subset of patients with NSCLC primary (p-value = 0.8142), or
Breast primary (p-value = 0.8023) or Other primary (p-value = 0.3597).
Time to Clinical Progression in the Brain
Time to clinical tumor progression, was estimated for all patients using
cumulative incidence analysis and Kaplan-Meier methods, and tested between
treatment arms using Gray’s test. Death in this analysis was recorded as a
competing risk when it occurred prior to diagnosis of clinical progression.
Per sponsor’s report, there was no statistically significant difference in the
cumulative incidence of clinical progression between the WBRT alone and
RSR13 + WBRT arms (?2 = 0.595, p-value = 0.4407). The sponsor has also
reported that there was no statistically significant difference in the cumulative
incidence of clinical progression between the WBRT alone and RSR13 + WBRT
arms in the subset of patients with NSCLC primary (p-value = 0.8142), or Breast
primary (p-value = 0.8023) or Other primary (p-value = 0.3597).
Response Rate in the Brain
Best response was determined from MRI o