FATIGUE
Text Button I
ACCREDITATION COUNCIL FOR GRADUATE MEDICAL EDUCATION (ACGME)
Accreditation Council for Graduate Medical Education (ACGME)
The ACGME’s Approach to Limit Resident Duty Hours 12 Months After Implementation:
A Summary of Achievements
Rationale for the Duty Hour Limits
Changes in health care delivery, and concerns that restricted sleep has a negative effect on performance
resulted in a need to limit resident duty hours. As the accrediting body for more than 7,900 residency
programs, the Accreditation Council for Graduate Medical Education is the entity charged with setting
and enforcing duty hour limits. In July 2003, ACGME instituted a comprehensive approach that includes:
(1) standards for resident hours and institutional oversight; (2) promoting compliance; and (3) increasing
knowledge on the effect of the standards and on innovative ways to conduct education and patient care
under limited resident hours. ACGME considers duty hour limits an important element of its
comprehensive approach to promote high-quality education and safe patient care.
The Standards
ACGME’s common duty hour standards acknowledge scientific evidence that long hours and sleep loss
have a negative effect on resident performance, learning and well-being. The duty hour standards include:
• An 80-hour weekly limit, averaged over four weeks;
• An adequate rest period, which should consist of 10 hours of rest between duty periods;
• A 24-hour limit on continuous duty, and up to six added hours for continuity of care and education;
• One day in seven free from patient care and educational obligations, averaged over four weeks;
• In-house call no more than once every three nights, averaged over four weeks;
• The option for programs in some specialties to request an increase of up to 8 hours in the weekly
hours, if this benefits resident education, with approval by their sponsoring institution and the
Residency Review Committee (RRC) in the given specialty.
ACGME chose 80-hours as the upper limit to safeguard against the negative effects of chronic sleep loss,
and selected a limit of 24 hours plus up to six hours to address the effects of acute sleep loss, and to allow
for adequate time for patient hand-off and didactic learning.1
1
Accreditation Council for Graduate Medical Education, Report of the Work Group on Resident Duty Hours and
the Learning Environment, June 11, 2002; (http://www.acgme.org, accessed July 16, 2004).
�FATIGUE
Text Button I
ACCREDITATION COUNCIL FOR GRADUATE MEDICAL EDUCATION (ACGME) (CONT’D)
Achievements in the first 12 Months
In the first 12 months after the July 2003 implementation, ACGME, the RRCs and the residency
education community rose to the challenge of applying the duty hour standards to 7,973 accredited
specialty and subspecialty programs. Programs and sponsoring institutions made changes in the clinical
training of residents, their patient care activities and the mechanisms for duty hour monitoring and
oversight. Many programs used schedule changes, night float and other rotation changes to bring duty
hours below the common limits. Others replaced resident services with care by nurse practitioners,
physician assistants or hospitalists. A few programs completely re-engineered their patient care and
education system to function well under reduced hours. Virtually all programs increased the clinical
responsibilities of faculty physicians. Highlights from the first year under the new standards include:
• ACGME collected data on duty hour compliance from the program directors of all accredited programs,
with more than 98% of ACGME-accredited programs responding by the March 2004 deadline. Senior
officials at each sponsoring institution verified this information.
• ACGME instituted systems to track compliance, including the number of programs cited for duty
hour violations, complaints related to resident hours, and programs applying for duty hour exceptions.
• During accreditation reviews conducted between July 2003 and June 2004, ACGME site visitors
interviewed program directors, faculty, residents and sponsoring institution representatives and
conducted primary reviews of documents that detail resident duty hours, including rotation schedules,
call rosters and some institutional duty hour surveys to verify compliance with the standards.
• Of the 2,235 programs reviewed during Academic Year 2003-04, 208 were applications for new
programs. Of 2,027 existing programs that received full reviews, 101 programs (5.0%) received one
or more citations related to non-compliance with the duty hour standards. The majority of citations
related to compliance with the 80-hour weekly limit (52 citations), followed by the requirement for
one day in seven free of program duties and the 24 + up to 6-hour limit on continuous duty (29 and 27
citations, respectively). RRCs requested that 42 programs provide them with dedicated reports that
detail their efforts to bring duty hours into compliance or general progress reports that included
information on duty hours. Detailed information on duty hour citations, including duty hour citations
and time to next RRC review by specialty, is shown at Exhibit 1.
• ACGME interviewed between 11,000 and 13,000 residents during scheduled accreditation site visits,
and via an electronic resident survey collected data on duty hour compliance from 25,176 residents in
1,489 programs. Among the respondents, 834 residents (3.3% of the responding residents) in 370
programs (24.8% of responding programs) reported working more than 80 hours per week during the
previous 4 weeks. That a small group of residents work beyond the duty hour limits likely relates to
factors associated with individual residents’ learning and practice performance, rather than program
level non-compliance with the standards. At the same time, the survey found a few programs where
the majority of residents worked significantly beyond the duty hour limits. ACGME is following up
with programs where the resident survey data suggests a potential program-level compliance problem.
• ACGME received 53 complaints related to non-compliance related to resident hours. Eleven were
dismissed as unfounded. For the remainder ACGME instituted appropriate follow-up activities,
including its procedure for “Rapid Response to Alleged Egregious Accreditation Violations or
Catastrophic Institutional Events” for the most serious complaints. Details are shown at Exhibit 2.
�FATIGUE
Text Button I
ACCREDITATION COUNCIL FOR GRADUATE MEDICAL EDUCATION (ACGME) (CONT’D)
•
•
•
•
•
•
The RRCs approved 75 requests by individual programs to extend the weekly limit to 88 hours, and
denied another 14 requests. Exhibit 3 shows requests by specialty. ACGME denied a request by the
surgical RRCs to increase the weekly limit for the surgical chief resident year to 88 hours, due a lack
of data thus far showing a negative effect of the limits, and ability of programs to request an increase
in their weekly limit for chief residents to 88-hours, with the approval of their institution and RRC.
Eleven RRCs have standards that are more restrictive than the common duty hour limits or do not
permit programs to apply for the increase in the weekly duty hour limit, as shown at Exhibit 4.
ACGME communicated its approach to limit resident duty hours and its compliance efforts to the
academic community and the public through published articles, interviews and information presented
on the ACGME Web site and in the quarterly ACGME Bulletin.
In August 2003, ACGME communicated with approximately 100,000 residents in accredited
programs through the officials at their sponsoring institution, informing them about the duty hour
standards and compliance monitoring activities, including residents’ rights to raise concerns about
violations of the standards with their institutions and, ultimately, ACGME.
ACGME is sensitive to the issue that reporting alleged non-compliance with the standards may place
such “whistleblowers” at risk for retaliation or retribution, and its confidential complaint management
process and institutional requirements seek to safeguard these individuals. In addition, ACGME has
emphasized to program directors and institutional leaders the need to protect “confidential reporters,”
beginning with an article in the fall 2003 ACGME Bulletin.
ACGME kept the academic community informed about compliance activities and “innovative ideas”
for meeting the standards thorough articles in the ACGME Bulletin, question and answer sections on
the ACGME Web site and presentations to the academic community. Successful approaches for
reducing hours that preserve a balance between education and service could be adopted or adapted by
other programs and institutions. A sampling of innovative ideas is presented at Exhibit 5.
Potential Future Refinements to the Standards
ACGME has solicited feedback on the elements of the standards that may reduce educational quality or
have other unintended effects, with the goal of assessing the need for future refinements. It is aware that
public attention is focused on the issue of resident hours and the mechanisms to ensure compliance and
believes that a period of at least 12 to 18 months without changes to the standards is needed to give
programs time to adapt education and patient care activities to the limits and to collect data on their effect.
ACGME may make future refinements in areas where key indices suggest the standards may be
problematic from an educational or patient care perspective. Revisions to the standards would be made
only in response to convincing data that they are necessary and would benefit education and/or patient
care, and after a process of soliciting broad input and support for any changes from the education
community and the general public.
�FATIGUE
Text Button I
ACCREDITATION COUNCIL FOR GRADUATE MEDICAL EDUCATION (ACGME) (CONT’D)
�FATIGUE
Text Button I
ACCREDITATION COUNCIL FOR GRADUATE MEDICAL EDUCATION (ACGME) (CONT’D)
�FATIGUE
Text Button I
ACCREDITATION COUNCIL FOR GRADUATE MEDICAL EDUCATION (ACGME) (CONT’D)
�FATIGUE
Text Button I
ACCREDITATION COUNCIL FOR GRADUATE MEDICAL EDUCATION (ACGME) (CONT’D)
�Text Button I
ACCREDITATION COUNCIL FOR GRADUATE MEDICAL EDUCATION (ACGME) (CONT’D)
Neurology: Reducing Neurology Resident Hours at UT Medical Branch, Galveston
In early 2003, this neurology program revised its resident scheduling patterns to conform to the ACGME
duty hour limits. The program’s nine residents all take night call with no differences between senior and
junior residents. Rotating residents do not participate in call. At the heart of the system is that each
resident is scheduled for a two-week long “night float” rotation three times per year. The other residents
are on a regular rotation with more limited call. No resident works more than 80 hours per week or 24
hours of continuous duty. The primary benefit is that residents no longer complain of being “post-call”
and do not fall asleep in conferences. Residents and faculty consider the plan a success.
Surgery: Models for Surgical Resident Education at Northwestern University, Chicago
A think tank at the McGaw Medical Center of Northwestern University developed four resident rotation
models the surgery residency program currently uses. The goal was to develop models programs can
adopt to comply with the standards while maintaining or enhancing resident education. In the Stretch
Model, residents take call every fourth night (or less) and leave the next morning. This is the easiest
approach to get to an 80-hour week, but it has no real educational advantages other than reducing duty
hours, presumably giving residents more time to read. The Night Float Model consists of a traditional
resident team system, except that a percentage of the program's residents are designated to a “night-float”
shift, usually for a month at a time. Each resident rotates on night float two to three months per year. The
day team has one hour of overlap with the night- float team to allow for a robust "sign-out." Teams
working during the day would take no in-house night call. The "night float" team works a night shift six
days per week, although larger programs may be able to accommodate a five nights per week schedule.
The Apprentice Model involves one resident working exclusively with one or two faculty members over
several months. Residents work side-by-side with their mentors in the operating room and outpatient
setting and take home call when their mentor is on call, and participate only in the care of their mentors'
patients. Faculty members are selected carefully based on dedication to education and an appropriate
practice profile. This model lends itself well to subspecialty areas like colorectal or breast surgery, but
also can be used for general surgery rotations. Apprentices take no in-house call, and are on duty less than
80 hours, even if they have to come in at night once or twice a week. In the Mastery (Case-Based) Model,
cases are assigned to residents solely based on their learning needs. Knowledge and skills associated with
diagnoses and operations are measured by personal progress, not by time. Proficiency is verified through
formal assessment, and residents are allowed to advance to other areas and are not required to scrub on
operations they have mastered unless they want to refresh their knowledge. Residents are responsible for
making arrangements to review the cases with the appropriate attending. They round on their own
patients in the morning and go to the clinic or operating room depending on their assignments for that
week. They are not required to take night call, but could take call from home. Learning expectations are
made clear at the start and are mastery-based, but broken down by year of training for planning purposes.
Surgery: From more than 110 to less than 80 hours at St. Luke’s Hospital, Bethlehem
After analyzing the responsibilities and tasks of its residents and the service requirements of their various
clinical rotations, the leadership of this surgery program instituted a modified night float system. From
Sunday through Thursday one resident is on a night-float rotation from 6 pm to 8 am and to 11 am for
Friday morning conferences. Two different residents are on call Friday night, Saturday day and night, and
Sunday during the day. The night-float resident changes weekly. Chief residents take call from home and
come to the hospital when needed.
�FATIGUE
Text Button I
ACCREDITATION COUNCIL FOR GRADUATE MEDICAL EDUCATION (ACGME) (CONT’D)
The modified night float system has advantages in a small surgery program: (1) residents miss few
clinical opportunities; (2) residents are able to attend surgical clinics and attending faculty office hours;
(3) residents can participate in time-protected conferences during the morning; (4) residents have more
time for rest and personal learning; (5) the night float resident is still involved in operative procedures in
that he/she participates in late elective surgical cases and is involved in emergency surgical cases at night.
Making the modified night float system a success requires a commitment by the faculty, nursing and
administration to make the residency primarily an educational experience. It also requires understanding
on the part of residents and faculty that the ACGME duty hour standards improve the educational
experience of residents. Finally, a robust sign-out of patients at the beginning and end of the night-float
period is a key element of a successful night-float model.
�
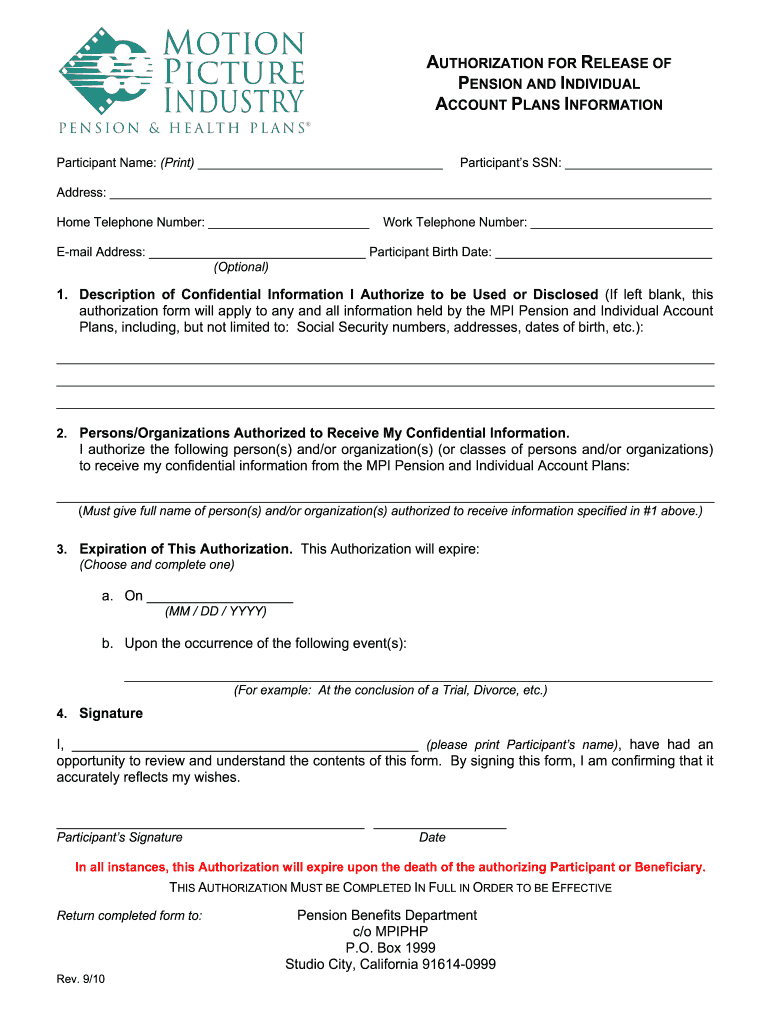
Practical tips for preparing your ‘Mpiphp Authorization For Release Of Health Information’ online
Are you fed up with the inconvenience of handling paperwork? Look no further than airSlate SignNow, the leading electronic signature platform for individuals and small to medium-sized businesses. Bid farewell to the lengthy process of printing and scanning documents. With airSlate SignNow, you can effortlessly finish and sign documents online. Utilize the robust features included in this user-friendly and cost-effective platform to transform your document management strategy. Whether you need to sign forms or gather signatures, airSlate SignNow makes it simple, requiring only a few clicks.
Follow these comprehensive steps:
- Access your account or sign up for a free trial with our service.
- Click +Create to upload a file from your device, cloud storage, or our form library.
- Open your ‘Mpiphp Authorization For Release Of Health Information’ in the editor.
- Click Me (Fill Out Now) to finalize the document on your end.
- Add and allocate fillable fields for others if needed.
- Proceed with the Send Invite settings to request eSignatures from others.
- Download, print your version, or convert it into a reusable template.
Don’t fret if you need to collaborate with others on your Mpiphp Authorization For Release Of Health Information or send it for notarization—our solution provides everything necessary to accomplish such tasks. Register with airSlate SignNow today and take your document management to the next level!