Vol. 11, 1355 – 1357, February 15, 2005
Clinical Cancer Research 1355
The Biology Behind
Nucleotide Excision Repair, Oxidative Damage, DNA Sequence
Polymorphisms, and Cancer Treatment
&& Commentary on Gu et al., p. 1408
Stephanie Q. Hutsell and Aziz Sancar
Department of Biochemistry and Biophysics, University of North
Carolina School of Medicine, Chapel Hill, North Carolina
INTRODUCTION
Can a single polymorphic site help tailor a cancer patient’s
chemotherapy regimen? The study by Zhao et al. (1) presented in
this issue of Clinical Cancer Research suggests that in fact
polymorphic sites in noncoding gene regions may determine how
a patient will react to a given chemotherapy and the likelihood of
cancer recurrence after treatment. The group focused their
investigation on a common polymorphism termed xeroderma
pigmentosum group A ( 4) [XPA ( 4)], whereby the fourth
nucleotide before the ATG start codon is A in about half the
population and G in about the other half (2, 3). The polymorphism
is in the Kozak sequence and thus the A form of the allele may
affect the translation efficiency of XPA resulting in reduced XPA
level and reduced excision repair capacity. Indeed, this group
previously reported that the A allele (XPA A variant in the authors’
terminology) is associated with reduced excision repair capacity
(4). In the current study, the authors report that the XPA G variant
in which both alleles contain G at the fourth position before the
initiation codon is associated with a higher rate of recurrence of
superficial bladder cancer after Bacillus Calmette-Guerin (BCG)
treatment. The authors report that during the follow-up period of
27.6 months from diagnosis, tumor recurred in 44% of patients
with the AA genotype, 62% in those with the AG genotype, and
74% in those with the GG genotype. To explain these findings, the
authors suggest that the XPA G variant exhibits increased DNA
repair capacity by nucleotide excision repair. This allows cancer
cells to bypass the apoptotic response induced by BCG treatment.
Nucleotide excision repair is the only human system that
protects against the carcinogenic effects of sunlight by removing
UV light-induced DNA adducts such as (6 – 4) photoproducts
and cyclobutane thymine dimers (5 – 8). Along with lightinduced lesions, the excision nuclease recognizes and excises a
broad spectrum of bulky lesions such as benzo(a)pyrene,
acetylaminofluorene, cisplatin, and psoralen DNA adducts (5).
The mechanism of excision repair is highly conserved from
E. coli to man and involves a damage recognition step, dual
incisions bracketing the lesion, removal of the damage in the form
of a 12- to 13-nucleotide-long oligomer in E. coli and a 24- to 32-
Received 1/6/05; accepted 1/13/05.
Requests for reprints: Aziz Sancar, Department of Biochemistry and
Biophysics, University of North Carolina School of Medicine, Mary Ellen
Jones Building, Campus Box #7260, Chapel Hill, NC 27599-7260. Phone:
919-962-0115; Fax: 919-966-2852; E-mail: Aziz_Sancar@med.unc.edu.
D2005 American Association for Cancer Research.
nucleotide-long oligomer in humans, repair synthesis to fill the
resulting gap, and finally ligation of the repair patch.
Human nucleotide excision repair has been recently
characterized at the biochemical level in considerable detail.
Six repair factors, XPA, RPA, XPC, TFIIH, XPG, and XPFERCC1, are necessary and sufficient to remove damage from
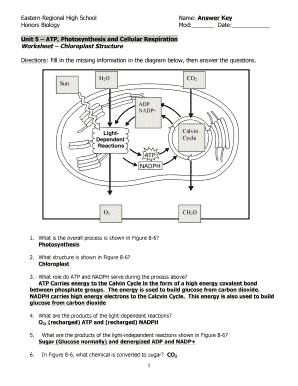
DNA. A current model for human nucleotide excision repair is as
follows: XPA, RPA, and XPC locate the damage site and recruit
the TFIIH transcription/repair factor, which contains six polypeptides including helicases XPB and XPD that unwind the DNA
around the damage site; the XPG and XPF-ERCC1 subunits are
responsible for the 3V and 5V dual incisions, respectively. Repair
synthesis proteins replication factor C, proliferating cell nuclear
antigen, and DNA polymerases y and q fill the gap, and in the
final step, the repair patch is sealed by DNA ligase I (refs. 9, 10;
Fig. 1). Mutations in any of the XP A-to-G coding sequences
result in XP, a disease characterized by extreme light sensitivity
and high incidence of skin cancer. Currently, all known XP cases
contain mutations in the coding regions of one of the XP genes. It
is conceivable that mutations in the noncoding or nontranscribed
regions of the XP genes may cause slight alteration in gene
expression so as not to give rise to an overt XP phenotype, but
of significant magnitude that subtle repair defects may manifest.
Even though nucleotide excision repair is generally thought
of as a repair system for bulky adducts, it has been shown that
it works with moderate efficiency on nonbulky DNA lesions,
such as DNA bases altered by oxidative damage that are usually
processed by base excision repair (11, 12). Because of this
property, the nucleotide excision repair system plays a backup
role for the base excision repair pathway in the removal of such
DNA adducts. Reactive oxygen species are by-products of
oxidative metabolism and are also produced in great quantities
during inflammatory reactions. They induce numerous DNA
lesions including thymine glycols, 8-oxoguanine, and cyclodeoxyadenosine. Nucleotide excision repair is capable of
removing all of these DNA lesions induced by reactive oxygen
species (13, 14).
In the study by Zhao et al. (1), the authors propose
a mechanism that involves the nucleotide excision repair pathway
and its response to oxidative damage, to explain why the XPA G
variant is less responsive to BCG treatment. The suggestion is
that BCG therapy provokes an inflammatory cellular response,
which subsequently results in the production of oxygen radicals
and extensive oxidative damage to DNA followed by apoptosis.
The XPA G variant was reported to have increased DNA repair
capacity (4). This increase in DNA repair capacity may be
responsible for removing a greater percentage of oxidative
damage from DNA, preventing the apoptotic pathway, and
permitting tumor cell survival, rendering BCG ineffective for
patients homozygous for the XPA G variant.
Downloaded from clincancerres.aacrjournals.org on July 11, 2018. © 2005 American Association for Cancer
Research.
�1356 Nucleotide Excision Repair Gene
Fig. 1 Model for nucleotide excision repair.
Damage is recognized by RPA, XPA, and XPC in
a cooperative way. TFIIH is recruited to form preincision complex 1 (PIC1). XPG displaces XPC
from PIC1 to form PIC2. Finally, XPF-ERCC1 is
recruited to form PIC3 in which XPG makes the 3V
incision 6 F 3 nucleotides 3V from the damage site
and XPF-ERCC1 makes the 5V incision 20 F 5
nucleotides 5V to the damaged bases releasing the
damage in the form of a 27-nucleotide-long
oligomer. Repair synthesis proteins replication
factor C, proliferating cell nuclear antigen, and
DNA polymerases y and q fill the gap. Repair patch
is sealed by DNA ligase.
This is a reasonable speculation. However, there are certain
caveats to this interpretation. The report that the XPA G variant
allele shows increased DNA repair capacity requires verification
by more than just the reporter gene assays reported previously (4).
Currently, there is no evidence that the level of XPA protein is
increased constitutively or in response to damage in XPA G variant
patients. Furthermore, there is no evidence by independent repair
assays that there is increased excision repair activity in cells with
the XPA G variant. In addition, although it has been shown that
human nucleotide excision repair excises 8-oxoguanine, thymine
glycol, and perhaps other oxidative stress base lesions from DNA
as efficiently as the light-induced cyclobutane thymine dimer
(13), 8-oxoguanine and other oxidative stress lesions are repaired
very efficiently by 8-oxoguanine DNA glycosylase and other
glycosylases (15). Therefore, the magnitude of contribution of
nucleotide excision repair in the removal of oxidative damage to
nucleotide bases remains to be determined. As a final caveat,
previous studies (4, 16) have shown that the XPA G variant allele
has a protective effect against the onset of lung cancer. Those
reports predict that individuals with XPA G variant would have
lower incidence of bladder cancer as well. Zhao et al. (1) did not
study an unaffected sample of the population to determine if the
XPA G variant allele shows a similar protective effect against
superficial bladder cancer. If it does, this study reveals an
interesting issue in the genetic consideration in carcinogenesis and
cancer treatment: a mutation makes the carriers more resistant to
cancer, but once they develop cancer, the same mutation may
make them less responsive to treatment by agents that directly or
indirectly damage DNA.
This is an interesting study, and in conclusion, the
connection between the XPA G variant polymorphism and lack
of response to BCG treatment could have significant clinical
Downloaded from clincancerres.aacrjournals.org on July 11, 2018. © 2005 American Association for Cancer
Research.
�Clinical Cancer Research 1357
applications. However, whether or not this polymorphism
is relevant to nucleotide excision repair activity needs further
investigation.
REFERENCES
1. Gu J, Dinney CP, Zhu Y, et al. Nucleotide excision repair gene
polymorphisms and recurrence after treatment for superficial bladder
cancer. Clin Cancer Res. 2004;11:1408-16.
2. Richards FM, Goudie DR, Cooper WN, et al. Mapping the multiple
self-healing squamous epithelioma (MSSE) gene and investigation of
xeroderma pigmentosum group A (XPA) and PATCHED (PTCH) as
candidate genes. Hum Genet 1997;101:317 – 22.
3. Butkiewicz D, Rusin M, Harris CC, Chorazy M. Identification of four
single nucleotide polymorphisms in DNA repair genes: XPA and XPB
(ERCC3) in Polish population. Hum Mutat 2000;15:577 – 8.
4. Wu X, Zhao H, Wei Q, et al. XPA polymorphism associated with
reduced lung cancer risk and a modulating effect on nucleotide excision
repair capacity. Carcinogenesis 2003;24:505 – 9.
5. Sancar A. DNA excision repair. Annu Rev Biochem 1996;65:43 – 81.
6. Sancar A, Lindsey-Boltz LA, Unsal-Kacmaz K, Linn S. Molecular
mechanisms of mammalian DNA repair and the DNA damage
checkpoints. Annu Rev Biochem 2004;73:39 – 85.
7. Wood R. Nucleotide excision repair in mammalian cells. J Biol Chem
1997;272:23465 – 8.
8. Sancar A, Reardon JT. Nucleotide excision repair in E. coli and man.
Adv Protein Chem 2004:69:43 – 71.
9. Mu D, Hsu DS, Sancar A. Reaction mechanism of human DNA repair
excision nuclease. J Biol Chem 1996;5:8285 – 94.
10. Reardon JT, Sancar A. Recognition and repair of the cyclobutane
thymine dimer, a major cause of skin cancers, by the human excision
nuclease. Genes Dev 2003;17:2539 – 51.
11. Branum ME, Reardon JT, Sancar A. DNA repair excision nuclease
attacks undamaged DNA. A potential source of spontaneous mutations.
J Biol Chem 2001;6:25421 – 6.
12. Huang JC, Hsu DS Kazantsev A, Sancar A. Substrate spectrum of
human excinuclease: repair of abasic sites, methylated bases, mismatches,
and bulky adducts. Proc Natl Acad Sci U S A 1994;91:12213 – 7.
13. Reardon JT, Bessho T, Kung HC, et al. In vitro repair of oxidative
DNA damage by human nucleotide excision repair system: possible
explanation for neurodegeneration in xeroderma pigmentosum patients.
Proc Natl Acad Sci U S A 1997;19:9463 – 8.
14. Kuraoka I, Bender C, Romieu A, et al. Removal of oxygen freeradical-induced 5V,8-purine cyclodeoxynucleosides from DNA by the
nucleotide excision-repair pathway in human cells. Proc Natl Acad Sci
U S A 2000;11:3832 – 7.
15. Fromme JC, Verdine GL. Base excision repair. Adv Protein Chem
2004;69:1 – 41.
16. Butkiewicz D, Popanda O, Risch A, et al. Association between the
risk for lung adenocarcinoma and a ( 4) G-to-A polymorphism in the
XPA gene. Cancer Epidemiol Biomarkers Prev 2004;13:2242 – 6.
Downloaded from clincancerres.aacrjournals.org on July 11, 2018. © 2005 American Association for Cancer
Research.
�Nucleotide Excision Repair, Oxidative Damage, DNA
Sequence Polymorphisms, and Cancer Treatment
Stephanie Q. Hutsell and Aziz Sancar
Clin Cancer Res 2005;11:1355-1357.
Updated version
Cited articles
Citing articles
E-mail alerts
Reprints and
Subscriptions
Permissions
Access the most recent version of this article at:
http://clincancerres.aacrjournals.org/content/11/4/1355
This article cites 12 articles, 4 of which you can access for free at:
http://clincancerres.aacrjournals.org/content/11/4/1355.full#ref-list-1
This article has been cited by 1 HighWire-hosted articles. Access the articles at:
http://clincancerres.aacrjournals.org/content/11/4/1355.full#related-urls
Sign up to receive free email-alerts related to this article or journal.
To order reprints of this article or to subscribe to the journal, contact the AACR Publications
Department at pubs@aacr.org.
To request permission to re-use all or part of this article, use this link
http://clincancerres.aacrjournals.org/content/11/4/1355.
Click on "Request Permissions" which will take you to the Copyright Clearance Center's
(CCC)
Rightslink site.
Downloaded from clincancerres.aacrjournals.org on July 11, 2018. © 2005 American Association for Cancer
Research.
�