Transform your healthcare sales cycle management with airSlate SignNow
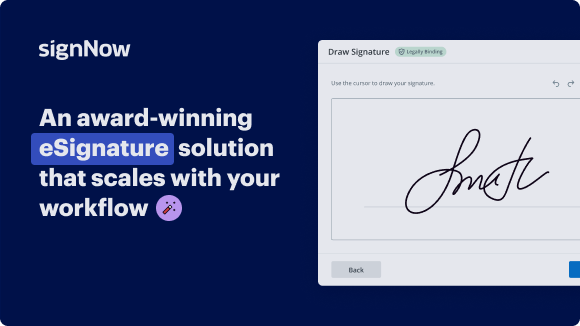
See airSlate SignNow eSignatures in action
Our user reviews speak for themselves






Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.

Sales Cycle Management for Healthcare
Sales cycle management for Healthcare with airSlate SignNow
Take advantage of airSlate SignNow's user-friendly interface and powerful features to revolutionize your sales cycle management for healthcare. Say goodbye to manual paperwork and hello to a more efficient way of handling documents.
Sign up for a free trial of airSlate SignNow today and experience the benefits firsthand!
airSlate SignNow features that users love
Get legally-binding signatures now!
FAQs online signature
-
What is the sales cycle of insurance?
The insurance sales cycle refers to the number of days it takes for an application to go from the initial submission to policy issuance. During this time, a series of steps and processes are conducted before a policy is issued. Currently, the average insurance sales cycle is between 60 and 90 days.
-
What is the average sales cycle in healthcare?
Sales Cycles The average B2B sales cycle lasts 102 days. In the healthcare industry, this cycle can be more than twice as long, lasting more than two quarters. Sales cycles for bigger ticket items may take even longer. Again, you can't expect to change healthcare sales cycles overnight.
-
What are the 7 stages of the sales cycle?
The 7 steps of a sales cycle are: prospecting, making contact, qualifying your prospects, nurturing your prospect, presenting your offer, overcoming objections, and finally closing the sale.
-
What is the cycle of sales management?
Let's break down the seven main stages of the sales cycle: prospecting, making contact, qualifying your lead, nurturing your lead, presenting your offer, overcoming objections, and closing the sale.
-
What is the sales cycle of a health plan?
A typical sales cycle in health insurance involves several stages: prospecting for insurance leads, initial contact, assessing client needs, presenting insurance policies, handling objections, closing the sale, and follow-up for cross-selling or upselling opportunities.
-
What is the sales process cycle?
A sales cycle goes from leads to prospects to customers, and along the way, we earn the right to keep talking, listening, and selling. We have to take it one step at a time and do those steps in the right order. It's why we don't dive into our product details before we've found out the problem they're trying to solve.
-
What are the 5 steps of the sales cycle?
How the 5-step sales process simplifies sales Approach the client. Discover client needs. Provide a solution. Close the sale. Complete the sale and follow up.
-
What is revenue cycle management in healthcare?
Revenue cycle management (RCM) is a financial process used by healthcare providers to bill, track, and collect incoming payments. RCM encompasses patient registration, insurance verification, claims submissions, patient billing, and collections.
Trusted e-signature solution — what our customers are saying
How to create outlook signature
So, there are a lot of KPIs that you want to track with your revenue cycle process and we'll go through some of the highlights. Charge lag - how many days does it take you to submit a claim? 1-5 days is really considered the industry standard. People we talk to, the places I've been --- 1-5 days is acceptable. Anything that's 6-10 days, maybe that's the average and over that you're really getting into the risk zone. Days in A/R. This is also known at some companies as DSO. This is a different metric. This is the number of days from the date of service to the payment date. How many days from that encounter are you waiting to get your paycheck? 35 days is the goal. You can be really aggressive with anything from 30-34. Anything 45 or higher is more of a risk and you really need to dig in and see if it's taking you longer to get your charges out the door (charge lag) or is a payer just by process taking a while. Clean claims rate. So you want your clean claims to be a really big metric. 95% or above is a great goal. You want to put your resources on the front end to make sure you have every check and balance as you can that a clean claim is going to the payer for reimbursement. You don't want to have to work this stuff on the back end. You want to put your work on the front end. A/R. Let's talk about A/R. We age it in 30-day buckets. Anything over 90 days aged from the date of service, you want that to be less than 10%. So, 10% 90 days and over, there are some things out there that take time to work, maybe you're waiting on an addendum with medical records, but you want to keep that A/R at 90 days or below. Rejection rate and denial rate - those are just two ways a claim can get hung up and start hanging out on your A/R for an extended period of time. So, you want you rejection rate to be less than 10%, meaning that you attempted to submit a claim but you didn't get it there to the payer. So you want to make sure again you're going back to that clean claims rate and measuring to make sure you have checks and balances on the front end. This may be with your type of software, this may be people looking at the process to make sure you're not missing anything. Cash collection. So, 90-plus percent. Across the industry, anything from 85% to 96% are the common numbers we hear. 90-plus percent, I would have a goal of 95%. That to me is aggressive but it makes sure you're getting that cash back in the door, especially with those in-network payers where you have a contract and you know what you should be paid. Bad debt. This can be measured a lot of ways. The metric gauges the amount of non-contractual charges, things that are a write-off. You really want to limit this. You don't want to work for free. You want this to be less than 5% if at all possible.
Show more