Collaborate on Hospital Receipt Format for Quality Assurance with Ease Using airSlate SignNow
See how it works!Click here to sign a sample doc
See airSlate SignNow eSignatures in action
be ready to get more
Choose a better solution
Move your business forward with the airSlate SignNow eSignature solution
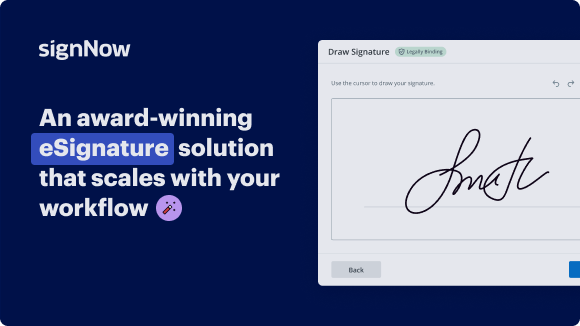
Add your legally binding signature
Create your signature in seconds on any desktop computer or mobile device, even while offline. Type, draw, or upload an image of your signature.
Integrate via API
Deliver a seamless eSignature experience from any website, CRM, or custom app — anywhere and anytime.
Send conditional documents
Organize multiple documents in groups and automatically route them for recipients in a role-based order.
Share documents via an invite link
Collect signatures faster by sharing your documents with multiple recipients via a link — no need to add recipient email addresses.
Save time with reusable templates
Create unlimited templates of your most-used documents. Make your templates easy to complete by adding customizable fillable fields.
Improve team collaboration
Create teams within airSlate SignNow to securely collaborate on documents and templates. Send the approved version to every signer.
Our user reviews speak for themselves






Collect signatures
24x
faster
Reduce costs by
$30
per document
Save up to
40h
per employee / month
airSlate SignNow solutions for better efficiency
Keep contracts protected
Enhance your document security and keep contracts safe from unauthorized access with dual-factor authentication options. Ask your recipients to prove their identity before opening a contract to hospital receipt format for quality assurance.
Stay mobile while eSigning
Install the airSlate SignNow app on your iOS or Android device and close deals from anywhere, 24/7. Work with forms and contracts even offline and hospital receipt format for quality assurance later when your internet connection is restored.
Integrate eSignatures into your business apps
Incorporate airSlate SignNow into your business applications to quickly hospital receipt format for quality assurance without switching between windows and tabs. Benefit from airSlate SignNow integrations to save time and effort while eSigning forms in just a few clicks.
Generate fillable forms with smart fields
Update any document with fillable fields, make them required or optional, or add conditions for them to appear. Make sure signers complete your form correctly by assigning roles to fields.
Close deals and get paid promptly
Collect documents from clients and partners in minutes instead of weeks. Ask your signers to hospital receipt format for quality assurance and include a charge request field to your sample to automatically collect payments during the contract signing.
be ready to get more
Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.

Discover how to simplify your process on the hospital receipt format for Quality Assurance with airSlate SignNow.
Looking for a way to streamline your invoicing process? Look no further, and adhere to these simple guidelines to easily work together on the hospital receipt format for Quality Assurance or ask for signatures on it with our intuitive platform:
- Сreate an account starting a free trial and log in with your email credentials.
- Upload a document up to 10MB you need to sign electronically from your PC or the web storage.
- Continue by opening your uploaded invoice in the editor.
- Execute all the necessary actions with the document using the tools from the toolbar.
- Select Save and Close to keep all the changes made.
- Send or share your document for signing with all the needed recipients.
Looks like the hospital receipt format for Quality Assurance process has just turned more straightforward! With airSlate SignNow’s intuitive platform, you can easily upload and send invoices for electronic signatures. No more producing a hard copy, signing by hand, and scanning. Start our platform’s free trial and it enhances the whole process for you.
How it works
Access the cloud from any device and upload a file
Edit & eSign it remotely
Forward the executed form to your recipient
be ready to get more
Get legally-binding signatures now!
FAQs
-
What is the hospital receipt format for quality assurance?
The hospital receipt format for quality assurance refers to a standardized document layout used by healthcare facilities to ensure accurate billing and record-keeping. This format helps maintain consistency in data presentation, aiding in quality assessments and audits. By utilizing this format, hospitals can enhance their financial accuracy and improve service quality. -
How can airSlate SignNow help with creating a hospital receipt format for quality assurance?
airSlate SignNow provides customizable templates that enable hospitals to generate a hospital receipt format for quality assurance quickly and efficiently. Users can easily input their specific information, ensuring that receipts meet compliance standards. This streamlines the billing process and minimizes errors associated with manual entry. -
Are there any costs associated with using airSlate SignNow for hospital receipt formats?
Yes, airSlate SignNow offers various pricing plans depending on the features and level of access required. These plans include options suitable for small clinics to large hospitals, ensuring that organizations can find an affordable solution for generating hospital receipt formats for quality assurance. A free trial is also available for new users to explore the platform's features. -
What features does airSlate SignNow offer for hospital receipt format creation?
airSlate SignNow includes a range of features for creating a hospital receipt format for quality assurance, such as customizable templates, electronic signatures, and document storage. Additionally, the platform supports easy sharing and collaboration on documents, improving workflow efficiency. These features help healthcare providers maintain accurate billing practices. -
Can airSlate SignNow integrate with other healthcare management systems?
Yes, airSlate SignNow can seamlessly integrate with various healthcare management systems, enhancing the efficacy of generating a hospital receipt format for quality assurance. Integration allows for automatic data synchronization, reducing the need for manual entry and minimizing errors. This results in a more streamlined billing process and better overall service delivery. -
What are the benefits of using an electronic hospital receipt format for quality assurance?
Using an electronic hospital receipt format for quality assurance offers numerous benefits, including increased accuracy, reduced paper usage, and faster processing times. Electronic receipts are easy to store and retrieve, aiding in efficient audits and reducing the risk of misplacing documents. This convenience ultimately leads to improved service quality and patient satisfaction. -
How does airSlate SignNow ensure compliance with healthcare regulations when generating hospital receipts?
airSlate SignNow ensures compliance with healthcare regulations by offering secure templates that adhere to industry standards for data protection and privacy. The platform uses encryption for data security and provides audit trails for document alterations. This focus on compliance is essential for hospitals when generating a hospital receipt format for quality assurance.
What active users are saying — hospital receipt format for quality assurance
Get more for hospital receipt format for quality assurance
- Free auto repair invoice template word for non-profit organizations
- Interior Design Invoice Template for Businesses
- Interior design invoice template for corporations
- Interior Design Invoice Template for Enterprises
- Interior design invoice template for small businesses
- Interior Design Invoice Template for Teams
- Interior design invoice template for organizations
- Interior Design Invoice Template for NPOs
Find out other hospital receipt format for quality assurance
- Sign Residential lease electronically
- Sign Residential lease agreement online
- Sign Residential lease agreement form electronically
- Sign Residential lease application online
- Sign Residential lease contract electronically
- Sign Residential lease form online
- Sign Room lease agreement electronically
- Sign Simple confidentiality agreement online
- Sign Simple lease agreement electronically
- Sign Simple rental agreement form online
- Sign Standard confidentiality agreement electronically
- Sign Standard lease form online
- Sign Standard rental agreement electronically
- Sign Standard residential lease agreement online
- Sign Tenant lease agreement electronically
- Sign Commercial real estate contract electronically
- Sign Contract online
- Sign Contract for work electronically
- Sign Contract leasing online
- Sign Contract of employment electronically