Workers' Compensation (WC) # Average Weekly Wage
Claimant's Name
Date First TTD Payment
Social Security#
Date of MMI
Date First Payment of PPD
Carrier Claim #
Employer
Insurance Carrier
Third Party Administrator
Medical to Date (total) $
Disfigurement (total) $
Vocational Rehabilitation Services (total) $
Whole Person Impairment
Temporary Total Disability (TTD) (total) $
Temporary Partial Disability (TPD) (total) $
Scheduled Impairment % Part of Body Code
Stipulation $
Scheduled Impairment % Part of Body Code
through
x $
x $
through
x $
x $
through
x $
x $
through
x $
Amount of Interest Paid $
Amount Overpaid $
Claims Representative
Toll-Free Phone#
Address
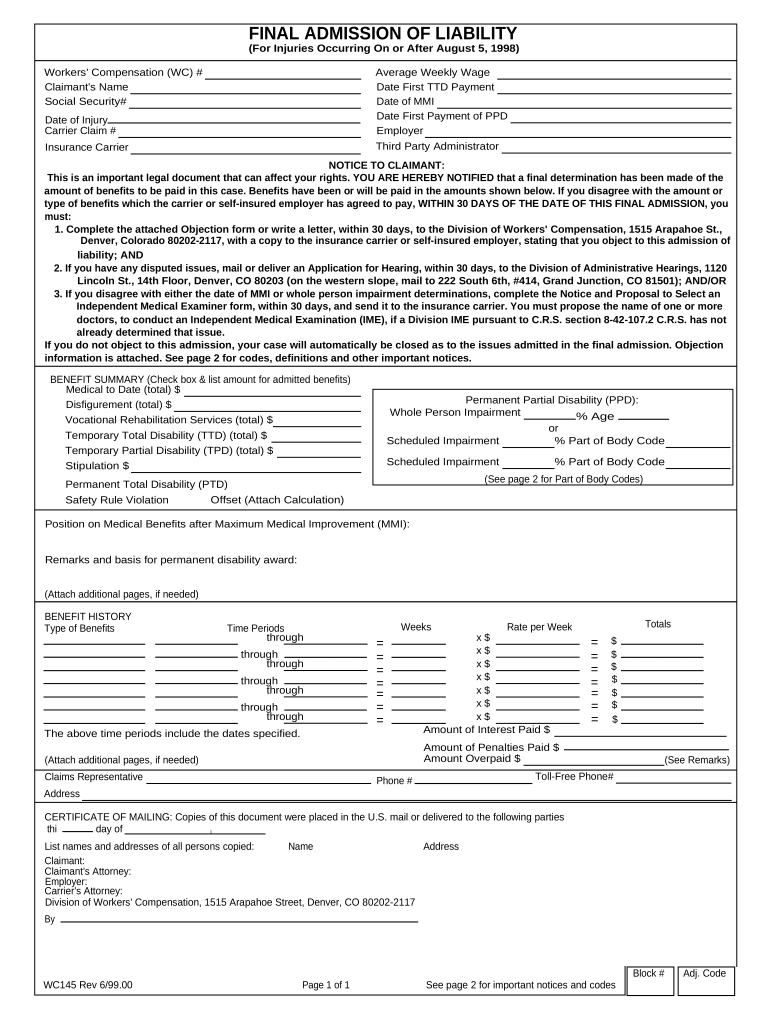
FINAL ADMISSION OF LIABILITY(For Injuries Occurring On or After August 5, 1998)
Date of Injury
NOTICE TO CLAIMANT: This is an important legal document that can affect your rights. YOU ARE HEREBY NOTIFIED that a final determination has been made of the
amount of benefits to be paid in this case. Benefits have been or will be paid in the amounts shown below. If you disagree with the amount ortype of benefits which the carrier or self-insured employer has agreed to pay, WITHIN 30 DAYS OF THE DATE OF THIS FINAL ADMISSION, youmust:1. Complete the attached Objection form or write a letter, within 30 days, to the Division of Workers' Compensation, 1515 Arapahoe St., Denver, Colorado 80202-2117, with a copy to the insurance carrier or self-insured employer, stating that you object to this admission of
liability; AND2. If you have any disputed issues, mail or deliver an Application for Hearing, within 30 days, to the Division of Administrative Hearings, 1120
Lincoln St., 14th Floor, Denver, CO 80203 (on the western slope, mail to 222 South 6th, #414, Grand Junction, CO 81501); AND/OR
3. If you disagree with either the date of MMI or whole person impairment determinations, complete the Notice and Proposal to Select an Independent Medical Examiner form, within 30 days, and send it to the insurance carrier. You must propose the name of one or more
doctors, to conduct an Independent Medical Examination (IME), if a Division IME pursuant to C.R.S. section 8-42-107.2 C.R.S. has notalready determined that issue. If you do not object to this admission, your case will automatically be closed as to the issues admitted in the final admission. Objection
information is attached. See page 2 for codes, definitions and other important notices.
BENEFIT SUMMARY (Check box & list amount for admitted benefits)
Permanent Partial Disability (PPD):
% Age or
Permanent Total Disability (PTD)
Safety Rule Violation
(See page 2 for Part of Body Codes)
Offset (Attach Calculation)
Position on Medical Benefits after Maximum Medical Improvement (MMI):
Remarks and basis for permanent disability award:
(Attach additional pages, if needed)
BENEFIT HISTORYType of Benefits Time Periods Weeks Rate per Week Totals
through
= = $
=
through = $
= = $
=
through
= = $
= $
=
= $
= = $
The above time periods include the dates specified.
Amount of Penalties Paid $ (Attach additional pages, if needed) (See Remarks)
Phone #
CERTIFICATE OF MAILING: Copies of this document were placed in the U.S. mail or delivered to the following partiesthis day of
I
List names and addresses of all persons copied: Name Address
Claimant:Claimant's Attorney:Employer:Carrier's Attorney:Division of Workers' Compensation, 1515 Arapahoe Street, Denver, CO 80202-2117
By:
Block # Adj. Code WC145 Rev 6/99.00 Page 1 of 1 See page 2 for important notices and codes
NOTICE TO CLAIMANT:
YOU ARE HEREBY NOTIFIED that if a child support obligation is owed, compensation benefits may be attached, and
payment of the child support obligation may be withheld and forwarded to the obligee pursuant to C.R.S. section 8-
42- 124 and C.R.S. section 26-13-122(4). YOU ARE FURTHER NOTIFIED that you must provide written notice of any
award for social security, pension, disability or other source of income that might reduce your compensation
benefits. This notice must be sent to the insurance carrier or self-insured employer within 20 days after learning of
the payment or award. Failure to report may result in suspension of your benefits pursuant to C.R.S. section 8-42-
113.5.
BENEFITS:
Compensation benefits are paid by insurance carriers for compensable injuries. Temporary disability benefits are paid every
two weeks.
Medical Benefits - Current medical benefits for medical, hospital and surgical supplies, prescriptions, crutches, apparatus and
vocational rehabilitation.
Maximum Medical Improvement (MMI) - The date when any medically determinable physical or mental condition as a result of
injury has become stable and when no further treatment is reasonably expected to improve the condition.
Facial or Bodily Disfigurement - Serious, permanent disfigurement about the head, face or parts of the body normally exposed
to public view. Benefits are not to exceed $2000.
Temporary Total Disability (TTD) - Total disability of more than 3 working days. If disability lasts for more than 14 calendar
days, compensation shall be paid from the day the claimant left work. Compensation is payable at the rate of 66',''f 1/4% of the
average weekly wage in effect at the time of the injury not to exceed the statutory maximum. A loss of fringe benefits
specifically enumerated in the statute should be included in the calculation of the average weekly wage.
Temporary Partial Disability (TPD) - Temporary partial disability of more than three working days. Compensation is payable at
the rate of 66 11V 1/4% of the difference between the employee's average weekly wage at the time of injury and the employee's
average weekly wage during the continuance of the temporary partial disability not to exceed the statutory maximum.
Permanent Partial Disability (PPD) - For dates of injury on or after July 1, 1991, an award for PPD is based on permanent
impairment as defined by the authorized treating physician and is limited to the part of the body that is affected.
Whole Person Impairment - Loss of function affecting body parts, including mental, not listed under the schedule below.
Scheduled Impairment - Loss of function affecting the toes, feet, legs, fingers, hands, arms, eyes, vision and deafness. Codes
for scheduled impairment ratings used by insurance carriers are listed below:
Part of body codes for scheduled ratings:
01 Arm@ Shoulder
03 Hand@ Wrist
04 Thumb @Metacarpal
05 Thumb @ Proximal
06 Thumb @ Distal
07 Index @ Metacarpal
08 Index@ Proximal
09 Index@ Second
10 Index @ Distal
11 Middle @ Metacarpal
12 Middle @ Proximal
13 Middle@ Second
14 Middle @ Distal
15 Ring @ Metacarpal
16 Ring @ Proximal
17 Ring @ Second
18 Ring@ Distal
19 Little @ Metacarpal
20 Little @ Proximal
21 Little@ Second
22 Little @ Distal
23 Leg @ Hip25 Leg. @ Foot, Heel, Ankle
26 Great Toe @ Metatarsal
27 Great Toe@ Proximal
28 Great Toe @ Distal
29 Other Toe @ Metatarsal
30 Other Toe@ Proximal
31 Other Toe @ Distal
32 Eye Enucleation
33 Blindness One Eye
34 Deafness Both Ears
35 Deafness One Ear
36 Total Hearing 2nd Ear
If you have any questions or need forms, contact the Division of Workers' Compensation, Customer Service Unit at
303.318.8700 or toll-free at 888.390.7936.
WC145 Rev 6/99.00 Page 2 of 2
Name of Claimant:
Social Security #-
Workers' Compensation (WC) #-
Date of Injury:
Insurance Carrier Claim #-
Date of Final Admission:
OBJECTION TO FINAL ADMISSION OF LIABILITY
(For Injuries Occurring On or After August 5, 1998)
If you disagree with the Final Admission, you must mail or deliver an objection WITHIN 30 CALENDAR DAYS of
the date of the Final Admission to the Division of Workers' Compensation and send a copy to the insurance
carrier or self-insured employer. Also within 30 days, if you disagree with the determination of Maximum Medical
Improvement (MMI), and/or Whole Person Permanent Impairment*, you must propose one or more names of an
Independent Medical Examiner, if a Division Independent Medical Examination (IME) has not already determined
that issue, by completing the form on the back; AND you must request a hearing on any disputed issues.
Otherwise, your claim will be closed as to the issues admitted in the Final Admission of Liability.Please print and complete Sections I and II of this form. Complete the back of this form, if applicable. If you have any
questions, or need an Application for Hearing form and/or Application for Independent Medical Examination (IME) form,
you may contact the Customer Service Unit at 303.318.8700 or toll-free at 888.390.7936.
SECTION I
- OBJECTION TO FINAL ADMISSION
I contest this admission. Check the boxes that apply:
I am proposing the name(s) of an Independent Medical Examiner and requesting an Independent Medical Examination
(IME). I have not previously undergone a Division IME that resolved a dispute over maximum medical improvement
(MMI), or a whole person permanent impairment determination*. I am completing the Notice and Proposal to Select an
Independent Medical Examiner on page 4 of this form. Additional instructions are on page 4. I understand that I will be
responsible for the cost of the IME, and I must complete an Application for Independent Medical Examination
(IME) form.
*Note: If you believe that a scheduled rating should be a whole person rating, you may request an IME. If you
disagree with a scheduled rating, you may proceed directly to hearing without an IME. (See definition of scheduled
impairment rating and codes on page 2.)
I will mail or deliver an Application for Hearing form on disputed issues to the Division of Administrative Hearings within
30 calendar days of the date of the Final Admission. Disputes about MMI and/or whole person impairment ratings are not
ready for hearing until an IME has been completed.
SECTION 11
- CERTIFICATE OF MAILING
Copies of this document were placed in the U.S. mail or delivered to the following parties
this day of
List names and addresses of all persons
copied:
Name Address
Claimant:
Claimant's Attorney:
Employer:
Insurance Carrier:
Carrier's Attorney:
Division of Workers' Compensation, 1515 Arapahoe Street, Denver, CO 80202-2117
By
:
(Signature of claimant or claimant's representative)
WC145 Rev 6/99 00 Paae 3 of 3
MMI Permanent Impairment MMI and Permanent Impairment
WC #
Carrier Claim # Social Security #
Claimant Name
Date of Injury
I disagree with the determination by Dr.
dated
Signature of Requester
Phone#
Copies of this document were placed in the U.S. mail or delivered to the following parties this
day of
By:
COLORADO DEPARTMENT OF LABOR AND EMPLOYMENT
DIVISION OF WORKERS' COMPENSATION
NOTICE AND PROPOSAL TO SELECT AN INDEPENDENT MEDICAL EXAMINER
Complete Sections I and 11. Please read the information at the bottom of this form.
SECTION I Notice and Proposal of Independent Medical Examiner I
and I request a Division IME on the following issue: (check one)
I propose any one of the following physicians to conduct the IME: (The physician must be Level II accredited. Information on
accredited physicians and the Application for IME form may be obtained by calling the Customer Service Unit listed below.)
I understand that I need to talk to the other party to discuss this request. Once the negotiation process is completed, I must submit the
Application for IME form to the Division and all parties.
SECTION II Certificate of Mailing
I
List the names and address of all persons copied: Name Addres
s Claimant:
Claimant's Attorney:
Carrier:
Carrier's Attorney:
Division of Workers' Compensation, 1515 Arapahoe Street, Tower 2, Suite 640, Denver, CO 80202-2117
Signature
INFORMATIONAL SUMMARY
The following is a brief outline of the Division Independent Medical Examination (IME) process. This general information may not include allcircumstances and is not meant as legal advice. If you have any questions, contact the Customer Service Unit listed below.
1. The party requesting the IME (requester) must complete the Notice and Proposal for Independent Medical Examiner form. The requester must send this Notice to the other party. If you are the claimant, the other party is the insurance carrier. If you are the Insurance Carrier, the otherparty is the claimant or claimant's representative, if applicable. 2. The parties have 30 calendar days to negotiate the selection of the Independent Medical Examiner (physician who will conduct the IME). The
requester needs to obtain an Application for Independent Medical Examination (IME), Form WC77, during this time.
3. If the parties agree on the Independent Medical Examiner, the requester must schedule the examination promptly with the physician. The
requester must also complete the Application for IME form and submit this to the Division of Workers' Compensation, the physician, and theother party. 4. If the parties do not agree on the Independent Medical Examiner, or there is no response to the Notice and Proposal, the insurance carriermust complete the Notice of Failed IME Negotiation, Form WC165. A copy must be sent to the Division and the claimant. The partyrequesting the IME shall have 30 days from the date of the failure to agree or respond to submit Application for Independent MedicalExamination (IME), Form WC77. The Division will select a qualified physician to perform the IME. The parties will be notified by phone of thephysician's name within 10 calendar days after receipt of the application for an IME.
5.6.
The carrier must submit medical records to the physician and other party at least 14 calendar days before the examination.
The claimant must notify the carrier if a language interpreter is needed at least 14 calendar days before the examination. The requester isresponsible for paying the interpreter. 7. The requester must make the payment to the IME physician at least 10 calendar days before the examination. 8. The physician is required to mail the IME report to the parties and the Division within 20 calendar days of the examination. 9. If the requester wishes to cancel the IME process, contact the IME Section of the Division immediately.
If you have any questions or need an Application for Independent Medical Examination (IME), Form WC77, or any other forms, contactthe Division of Workers' Compensation Customer Service Unit at 303.318.8700 or toll free at 888..390.7936.
WC145 Rev 11/00
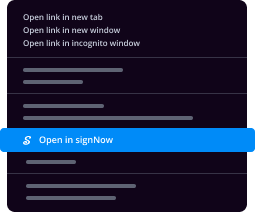
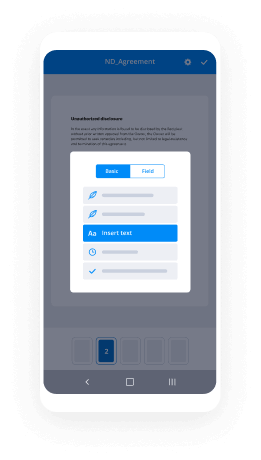
Essential tips for completing your ‘Final Workers Compensation 497300814’ online
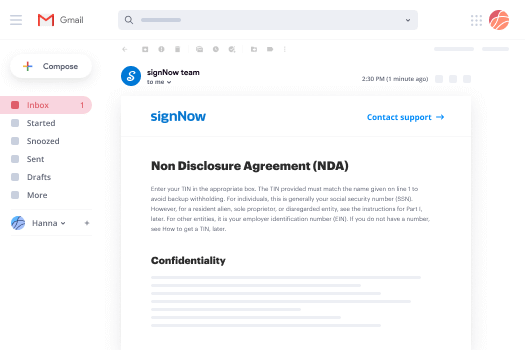
Are you fed up with the inconvenience of managing paperwork? Look no further than airSlate SignNow, the premier electronic signature tool for individuals and small to medium-sized businesses. Bid farewell to the tedious process of printing and scanning documents. With airSlate SignNow, you can effortlessly fill out and sign documents online. Utilize the powerful features integrated into this intuitive and cost-effective platform to transform your document management strategy. Whether you need to approve forms or gather electronic signatures, airSlate SignNow simplifies the process, needing only a few clicks.
Follow this comprehensive guide:
- Log in to your account or initiate a free trial with our service.
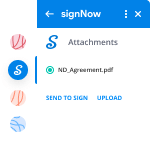
- Click +Create to upload a file from your device, cloud storage, or our form library.
- Access your ‘Final Workers Compensation 497300814’ in the editor.
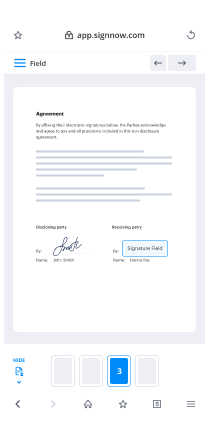
- Click Me (Fill Out Now) to set up the form on your end.
- Insert and assign fillable fields for others (if necessary).
- Proceed with the Send Invite options to request eSignatures from others.
- Save, print your version, or convert it into a reusable template.
Don’t fret if you need to work with your colleagues on your Final Workers Compensation 497300814 or send it for notarization—our platform provides you with everything you need to achieve those tasks. Create an account with airSlate SignNow today and elevate your document management to new levels!