The Open Dentistry Journal, 2010, 4, 201-206
201
Open Access
NOMA: A Preventable “Scourge” of African Children
Kalu U.E. Ogbureke1,2,* and Ezinne I. Ogbureke2
1
Department of Oral Biology, 2Department of Oral Health and Diagnostic Sciences, School of Dentistry,
Medical College of Georgia, Augusta Georgia, U.S.A.
Abstract: Noma is a serious orofacial gangrene originating intraorally in the gingival-oral mucosa complex before
spreading extraorally to produce a visibly destructive ulcer. Although cases of noma are now rarely reported in the developed countries, it is still prevalent among children in third world countries, notably in sub-Sahara Africa, where poverty,
ignorance, malnutrition, and preventable childhood infections are still common. This review summarizes historical, epidemiological, management, and research updates on noma with suggestions for its prevention and ultimate global eradication. The global annual incidence remains high at about 140,000 cases, with a mortality rate exceeding 90% for untreated
diseases. Where the patients survive, noma defects result in unsightly facial disfigurement, intense scarring, trismus, oral
incompetence, and social alienation. Although the etiology has long been held to be infectious, a definitive causal role between microorganisms cited, and noma has been difficult to establish. The management of noma with active disease requires antibiotics followed by reconstructive surgery. Current research efforts are focused towards a comprehensive understanding of the epidemiology, and further elucidation of the microbiology and pathogenesis of noma.
Although a formidable public health challenge, noma can be prevented with a potential for subsequent global eradication.
To achieve both desirable goals, detection of early disease is crucial because these early lesions respond to conventional
antibiotic treatments when instituted side by side with nutritional rehabilitation, and obviates the necessity for extensive
surgical reconstruction often indicated in late stage disease. The eradication of noma in the developed world in the mid
20th century bears out the notion of a similar outcome following effective preventive strategies in Africa. A fundamental
and necessary step towards attaining this goal is for the international community to adopt a perception of noma as an urgent global public health challenge. Research effort toward deciphering the microbiology, molecular events, and pathogenesis of noma also should intensify.
Keywords: Noma, Cancrum Oris, Sub-Sahara Africa, Acute Ulcerative Gingivitis, Preventable Disease, Surgical Management.
BACKGROUND
Noma (cancrum oris) is a debilitating gangrenous disease
of the orofacial region. It occurs in several regions of the
world, including the United States but with notable prevalence in sub-Sahara Africa [1, 2]. Although noma can affect
patients of any age group, infants and children are particularly susceptible [1]. Against a background of poor oral hygiene, long established common denominators to all noma
patients are malnutrition, depressed immunity, and increased
susceptibility to infections with normal oral commensal bacteria [3-7]. However, it is also true that not all patients, even
with the complete set of predisposing conditions, develop
noma. Indeed, because the majority of patients with these
backgrounds never develop noma, it is reasonable to postulate that the biological factors enumerated above may only
complement a stage set by other preexisting genetic and environmental conditions for the pathogenesis of noma.
Noma continues to be a significant cause of death among
child patients in areas where it is currently endemic [3]. In
the absence of timely therapeutic intervention, the mortality
rate is estimated at about 70-90% [8, 9]. When not fatal,
*Address correspondence to this author at the Department of Oral Biology,
School of Dentistry, Medical College of Georgia, 1120 15th Street, Augusta,
Georgia 30912, USA; Tel: 706 721-2526; Fax: 706 721-3392; E-mails:
kogbureke@mail.mcg.edu; kogbureke@netscape.net
1874-2106/10
noma leads to severe destruction of the mid-face structures,
notably the lips, cheek, maxilla, mandible, nose, and orbital
floor [3, 7, 9]. With the disfiguring sequel comes impaired
self-nutrition, speech, and ultimately, social rejection [10].
Antibiotic regimens remain the mainstay of treatment for
active disease. Plastic and reconstructive surgical procedures
are subsequently employed for the repair of the substantial
orofacial hard and soft tissue defects resulting from a completed natural course of the disease [10-12].
Africa not only maintains a disproportionate burden of
noma cases currently, but this avoidable and preventable
condition remains a visible scourge of African children [4,
13]. This review recaptures salient historical aspects of
noma, and summarizes management and research updates on
the etiology and pathogenesis of the disease. Strategies necessary for the prevention and ultimate eradication of noma
are proffered.
DISCUSSION
Historic and Epidemiological Profile of Noma
The word “noma” is a derivative of the Greek word
“nomein”, which means, “to devour”; an obvious allusion to
the rapidly destructive characteristic of the gangrene [2, 14].
The first clinical description of the disease was said to be in
1595 by Carolus Battus, a Netherlands surgeon [15]. Subse2010 Bentham Open
�202 The Open Dentistry Journal, 2010, Volume 4
quently, A.L. Richter (a Berlin physician) in 1828 drew attention to the presence of noma throughout Europe over
many centuries [16]. In his book, Richter also associated the
disease with malnutrition and childhood infections such as
measles. By the end of the 19th century, noma had virtually
disappeared from Western Europe as a result of improved
nutrition and hygiene among poor people [10, 17]. Although
during the Second World War cases of noma were rife in
Nazi concentration camps where victims died as a result of
malnutrition [18, 19] treatment of active noma became possible with the discovery of penicillin but paradoxically after
the disappearance of the disease from Europe.
Noma still remains the true “face of poverty” in less developed (and therefore impoverished) nations [20]. The 1994
report of the World Health Organization (WHO) characterized noma as a global health priority in response to reports
from humanitarian organization indicating increases in the
incidence of noma in various African countries [2, 21-24].
The report also coincided with an escalating economic crisis
within the continent, combined with the advent of
HIV/AIDS and the AIDS epidemic that followed, and an
increasing number of armed conflicts. These conditions bear
directly on the health and well being of children through
overcrowded living conditions, deteriorating sanitation, and
inadequate nutrition. In accord with its 1994 report, the
WHO established a global campaign against noma as one of
the initiatives emerging from that year’s WHO Day celebration. It also initiated an action program by way of a joint
project with the United States National Institute of Health
(NIH) and the University of Maryland Baltimore, Maryland
[2]. It stands to reason therefore that noma falls within the
rubric of neglected infectious diseases within the domain of
the dentist’s practice.
Although epidemiological facts and figures relating to
noma are at best fragmented and speculative, recent evidence
points to an increasing incidence of noma, particularly in the
poorer regions of Africa [4, 25, 26]. In 1998, the WHO made
available the first estimates on the incidence and prevalence
of noma with a worldwide annual incidence of 140,000
cases, and a prevalence of 770,000 in 1997 [9]. Estimates put
the world number of children under the age of six years with
noma in the order of several hundred thousand per year, including about 100,000 African children per year [3, 27]. The
estimated incidence is between one and seven cases per 1000
population in African countries, and up to 12 cases per 1000
in the most affected communities [8, 13].
Ogbureke and Ogbureke
to livestock, and increased exposure to viral and bacterial
agents [3, 28]. As of 1999, sub-Sahara Africa harboured 38
of the world’s 63 low-income nations, with a per capita annual income of $700, and with 40% of its 500 million people
subsisting on less than $1.00 per day [4, 29]. Thus, interplay
of economic globalization with confounders such as war and
drought constitutes the composite etiologic factor for noma
[30, 31].
The global distribution pattern of noma mirrors the
worldwide distribution of malnutrition, particularly that due
to vitamin A deficiency in children under the age of 5 years
[8, 32]; an observation that recapitulates that at the Nazi concentration camps where noma was rife in the 20th century. In
Nigeria, for example, most cases of noma become evident
during the “dry season”, an annual climatic variation coinciding with the “hungry months” due to food shortage [28,
29, 33, 34]. The hungry months in Nigeria also coincide with
the period of highest incidence of annual measles outbreaks
[28, 29, 35, 36]. Anthropometric, biochemical, and clinical
assessments of rural children in Sokoto Nigeria by Enwonwu
et al. [3] showed widespread severe protein energy malnutrition (PEM) among noma patients when compared to their
healthy but at-risk age-matched ethnic counterparts. The
Sokoto village children studied by Enwonwu et al. [3] also
exhibited marked deficiencies of retinol, ascorbate, zinc, and
the essential amino acids.
Antecedent Oral and Systemic Conditions. Poor oral hygiene is a significant risk factor and follows as a natural sequel of ignorance and poverty rife in these communities [13,
34]. Poor oral hygiene is an essential predisposing condition
to necrotizing ulcerative gingivitis (NUG) [13, 37]. NUG,
generally considered a key predisposing factor (and not infrequently alluded to as a precursor lesion) to noma, is a socioeconomic disease that was seen almost exclusively among
children in the developing countries following the end of the
Second World War [25, 37, 38]. Clinically, NUG presents as
a recurring gingival infection of complex etiology, characterized by necrosis of the interdental papillae, spontaneous
bleeding, and pain (Fig. 1). Like noma, the pathogenesis of
NUG is poorly understood although causative association
with specific microorganism such as spirochetes, Prevottela
intermedia, cytomegalovirus, Epstein-Barr, herpes simplex
The main obstacle to the procurement of concrete global
epidemiological data on noma is the limited or non-access of
patients to healthcare centers and the attendant inadequacies
of health record-keeping [8]. In addition, family members of
patients as well as health personnel are often incapable of
recognizing the condition. It is also not uncommon for noma
to evolve so rapidly that death ensues before the patients can
avail themselves of assistance from health facilities.
Etiologic and Risk Factors for Noma
Socioeconomic Factors. Poverty remains the single
most important risk indicator for noma [13]. Other related
factors include chronic malnutrition, poor environmental
sanitation, unsafe water supply, close residential proximity
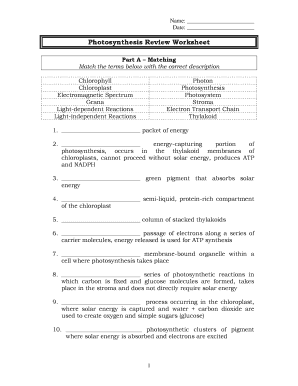
Fig. (1). Acute necrotizing ulcerative gingivitis (ANUG) showing
characteristic punched-out crater-like ulcers. (see also Fig. 2B).
�NOMA: A Preventable “Scourge” of African Children
The Open Dentistry Journal, 2010, Volume 4
203
Fig. (2). Patients with measles (A and B). Measles (B; arrow) usually antedate ANUG. (B; arrow).
viruses, and the measles virus is often cited [13, 25, 39-42].
Often patients may be under stress, immunosuppressed, or
have endocrine dysfunction as additional predisposing conditions [3, 38, 43, 44].
Consistent with earlier reports [3, 45, 46] we have, over
the years, observed that infection with measles (Fig. 2) most
commonly antedates the development of noma in African
children. In this respect other authors have cited interleukin12 (IL-12), an essential cytokine for the generation of cellmediated immunity, as being down-regulated in measles
patients [3]. Records of other antecedent infections include
malaria, tuberculosis, chicken pox, gastroenteritis, and bronchopneumonia [3, 47].
Microbiology of Noma. Although noma is presumed to be
of infectious aetiology, elucidating the precise microbiological culprits remains somewhat of an enigma. The primary
reason for this obscurity is obvious: the epicenter of noma
development, the oral cavity, is inhabited by several hundred
species of normal commensal bacteria [48-51]. A long held
notion is that noma is caused by spirochetes and fusobacteria
[5, 6, 52]. This notion partly stems from an extrapolation of
the microbiological culprits of the presumed noma antecedent, NUG, which also includes spirochetes and fusobacteria, and partly because the levels of these organisms appear
to be elevated in noma. However, a search of the English
literature to date showed no reports of genotypic alterations
from commensal to pathogenic among this group of organism in noma lesions. Furthermore, attempts to recapitulate
the lesions of noma (or NUG) in animal models via inoculation of suspect oral organisms in the absence of predisposing
conditions such as high plasma cortisol and depressed immunity have met with little success [2]. These findings challenge current etiologic concepts and continue to engender
intense research effort in this direction. As a result, new
theories are emerging regarding the pathogenesis of noma
[53].
Another difficulty encountered results from a common
speculation that differences in microbial population might
exist between “early” and “advanced” lesions. Parameters
for “early” and “advanced” noma lesions are yet to be precisely defined. In a broad sense however the early lesion
refers to the reddish/purple-coloured indurations (Fig. 3)
assumed to subsequently extend via ulceration and necrosis
to adjoining hard and soft tissues of the orofacial region in
the absence of timely treatment. On the other hand, the concept of advanced lesions alludes to the highly visible facial
tissue destruction evidenced by the presence of exposed
and/or sequestrated dead bone and soft tissue necrosis (Fig.
Fig. (3). Necrotic (Arrow ) erythematous ulcer still confined to the
alveolus and gingiva. This may represent the so-called “early
noma” lesion.
4) seen at later stages of the disease, or with rapidly progressing disease.
Nevertheless, recent reports suggest that noma is caused
by a mixed infection of oral and extraoral opportunistic
pathogens [3, 5, 6, 54] while incorporating the proposal that
some noma cases may be the result of zoonotic infection
with Fusobacterium necroforum. Using culture-independent
molecular methods, Paster et al. [54] reported the detection
of 67 bacterial species or phylotypes in advanced noma lesion of four Nigerian patients. Of these, phylotytpes that
were unique to noma infections included those in the genera
Eubacterium, Flavobacterium, Kocuria, Microbacterium,
Porphyromonas, Streptococcus (salivarius), Sphingomonas,
and Treponema. Twenty five species had not yet been grown
in vitro, 19 phylotypes, including Propionibacterium acne,
Staphylococcus species, and the opportunistic pathogens
Stenotrophomonas maltophilia and Ochrobacterum antrophi
were found in samples from one of the four patients. The
authors suggested that the presence in advanced noma lesions of organisms not normally associated with the oral
cavity may be due to contamination from the extraoral environment [54]. It however remains to be seen whether the
microbial constituent of “early” lesions differs remarkably
from that of advanced lesions.
Current Management Approaches
The consequences of noma relate to functional and esthetic problems. The acute and fulminating early stages of
the disease indicate need for antibiotic treatment, while the
chronic and disfiguring late stage requires surgical intervention: plastic and reconstructive surgeries designed to suit
individual cases.
Medical Management: During the acute stage, treatment
strategies aim to improve the overall health status of patients.
This includes nutritional, correction of ionic and acid-base
imbalances, administration of vitamins, and the administration of broad spectrum antibiotics to control infection [2]. In
our cumulative experiences spanning over two decades at
both the Maxillofacial Unit of the Ahmadu-Bello University
Hospital, Kaduna (KUEO) and the Noma Children Hospital
�204 The Open Dentistry Journal, 2010, Volume 4
Ogbureke and Ogbureke
indication to improve nutritional intake), and the debridement of the lesion to avoid secondary infection [2]. Routine
presurgical clinical investigations, including full blood count
and differentials, chest, skull and, when feasible, full mouth
radiological examinations must be carried out and documented. Skull radiographs that usually include temporomandibular joint (TMJ) views reveal the extent of bony ankylosis
and trismus present in a particular patient [11, 56-58]. Various profiles of presurgical photographs are also documented,
and subsequently used side-by-side with postsurgical photographs and other clinical parameters to assess treatment outcome.
Fig. (4). Advanced noma lesions. A. Rapidly destructive and fulminating disease requiring lengthy antibiotic treatment prior to surgery. B. Arrested advanced disease requiring short course of antibiotics before surgical reconstruction (arrow indicates sequestrum
formation (4A is adapted from Noma Project, Courtesy of Noma
Children Hospital, Sokoto, Nigeria).
Sokoto, Nigeria, antibiotics of the penicillin group with established potency in bone infections in combination with
metronidazole were found to be consistently useful in arresting the fulminating acute phase of noma. Overall, the “goldstandard” remains that antibiotics administered at the acute
phase must be sufficiently broad to cover the spectrum of
aerobic and anaerobic organisms inhabiting the periodontium
and oropharynx [2]. Improved oral hygiene instructions and
strategy also must accompany early phase treatment.
Surgical Reconstruction: In the African settings where
noma is overwhelmingly prevalent, there is also a shortage
of qualified surgical teams to treat the number of patients
requiring reconstruction [2, 25]. In some of these centers,
such as the Noma Children’s Hospital in Sokoto, Nigeria, the
local teams of surgeons and nurses are periodically supplemented by a volunteer team of expert representatives of humanitarian projects based in the developed countries [55].
The timing of surgical intervention in the management of
noma is critical. All forms of invasive surgery in the vicinity
of an acute phase lesion are discouraged because of the potential for such intervention to accelerate the destructive evolution of the disease. However, as soon as the acute phase is
visibly contained, usually evidenced by clear fibrotic demarcation at the normal tissue-lesion interface (see Fig. 4) the
design of surgical reconstruction should commence. Simultaneously, pre-surgical oral physiotherapy to relieve the
trismus resulting from the fibrous strictures and ankylosis
thereby enhancing intraoral access during surgery should
also commence. In Nigerian centers, for example, graduated
acrylic mouth screws are designed and fabricated, and these
are employed to relieve trismus and enhance mouth opening.
Physiotherapy continues postsurgical until acceptable or
normal mouth opening is achieved.
Over the years, the surgical corrections of noma deformities have proved to be daunting because each new case appears to present a unique composite of reconstructive challenges. There is therefore no standard surgical approach
common to all noma cases. Nevertheless, certain ground
rules for surgical treatment of noma appears to exist, and
include the postponement of treatment of lesions less than
one-year-old (except where the sequelae created an urgent
Surgery, which is invariably under general anesthesia,
sometimes presents peculiar anesthetic technique challenges
and risks. For example, because most noma patients with
significant loss of orofacial tissues and scarring develop limited mouth opening, intubation for general anesthesia is
sometimes challenging. Before the advent of fibreoptic technology [59], intubation for anesthesia of noma patients preparatory for surgery presented significant risks and challenges, often compounded by the shortage of experienced
nursing staff at centers located in the noma “hot spots” in
Africa. It was therefore not uncommon for patients who electively present for the repair of their defects for social reasons, to die from anaesthetic complications during or after
surgery.
Generally, the surgical designs involve the raising and
transposition of local and distant soft tissue flaps, depending
on the extent of tissue loss (see Fig. 4). In cases of considerable loss of facial or jaw bone, bone grafting may be considered in the sequence of reconstructive design. While a discussion of the technical details for each of the reconstructive
designs advocated by various practitioners, together with
their philosophies, is beyond the scope of this review, references to these details are cited in the text. Nevertheless, the
three fundamental principles underlying every good surgical
reconstruction design for noma repair are summarized. First,
due to the substantial tissue loss characteristics of most noma
defects, designs must account for adequate vascular supply
capable of sustaining flap viability [54, 60]. Therefore, both
locoregional and pedicled flaps must maintain adequate distance from pathological tissues. Second, designs must aim
for optimal length pedicles capable of anastomoses with local vessels in the area of repair [54, 59]. Third, an inner lining of the flap is required to prevent re-scarring and consequent functional impairment [61]. The deltopectoral, pedicled latissimus dorsi, pedicled radial forearm, and various
designs of forehead flaps are routinely employed to close
noma defects and provide outer lining [55]. Split-thickness
skin grafts are commonly used to provide inner linings.
The deltopectoral flap has been used as both outer and
inner linings with satisfactory results, and remains the most
versatile flap for the reconstruction of facial defects [57, 62,
63]. The advantage of the deltopectoral flap lies in the relative simplicity of its design, minimal blood loss during surgery, and the viability of the flap after surgery [62, 63]. The
various forehead flap designs are also simple. However, a
main criticism of the forehead flaps is that they often result
in unsightly appearance of the donor site.
�NOMA: A Preventable “Scourge” of African Children
The various myocutaneous flaps mentioned above are intricate and should be employed only by practitioners with the
appropriate experience and where adequate postoperative
care is available because of the associated longer morbidity.
Nath and Jovic [62, 63] advocate that myocutaneous flaps be
sparingly used, if at all, in children. However, it would appear that for some considerably large and sophisticated defects myocutaneous flaps would remain the only viable reconstructive option. The Abbe-Estlander, nasolabial, and
temporoauricular (Washio type) are local flaps that produce
excellent results in small to moderate defects involving the
upper lip, paranasal, and nasal areas [61]. Closure of oronasal fistulas can be achieved with the aid of tongue flaps [11].
Overall, because of the complexity of most noma defects,
single surgical procedures are not always feasible, and most
cases require revision surgeries to correct residual undesired
functional and esthetic outcome of initial treatment.
The Open Dentistry Journal, 2010, Volume 4
ACKNOWLEDGMENT
KUEO’s participation in the noma research project in
conjunction with the Forsyth Institute, Boston was supported
by the Division of Intramural Research, National Institute of
Dental and Craniofacial Research, National Institute of Dental and Craniofacial Research, National Institutes of Health,
Department of Health and Human Services, Bethesda, MD,
U.S.A.
REFERENCES
[1]
[2]
[3]
Research Update
Prior to designating noma as one of the five global priorities for study by a joint initiative between NIH/NIDCR and
WHO/ORH in the early 1990s, studies were carried out with
less coordination amongst groups in the forefront of noma
research. Following the characterization of noma as a major
health problem requiring integrated international resources
and expertise, the Federation Dentaire International (FDI)
and the WHO Joint Working Group in 1992 launched the
International Action Network Against Noma in 1994 [4].
This on-going initiative prompted studies that are now more
coordinated with the ultimate goal of preventing and eradicating noma. It is hoped that this goal will be attained
through studies elucidating more clearly the epidemiology of
noma and its etiopathogenesis. In this regard, of course, the
main battle-ground remains the developing countries of subSahara Africa.
A combined team of researchers from the Dental School
of the University of Maryland, Forsyth Institute Boston, the
Nigerian Institute of Medical Research Lagos, and the University of Lagos, School of Dentistry has been investigating
the microbiological etiology of noma, as well as the immune
and nutritional statutes of noma patients in Sokoto, Nigeria
over the past decade.
205
[4]
[5]
[6]
[7]
[8]
[9]
[10]
[11]
[12]
[13]
[14]
[15]
SUMMARY
[16]
Although a formidable public health challenge, noma is
both preventable and amenable to eradication. Detection of
early lesions is crucial to an overall preventative goal because these early lesions respond to conventional antibiotic
treatments when instituted side by side with nutritional rehabilitation, thereby obviating the late stage and potentially
lethal gangrenes. The concept of “think globally act locally”
[31] is clearly germane to the goal of eradicating noma in
Africa and, by implication, globally. A fundamental and
necessary step towards attaining this goal is for the international community to adopt a perception of noma as an urgent
global public health challenge. This challenge must then be
confronted by international agencies and research-sponsoring
organization by addressing the various local logistical obstacles, increasing financial support for on-going research activities, and training local research scientists and mentors for
noma centers in Africa.
[17]
[18]
[19]
[20]
[21]
[22]
[23]
[24]
[25]
Enwonwu CO, Falkler WA, Idigbe EO. Oro-facial gangrene
(noma/cancrum oris): pathogenetic mechanisms. Crit Rev Oral Biol
Med 2000; 11:159-71.
Baratti-Mayer D, Pittet B, Montandon D, et al., Geneva study
group on noma. noma: an "infectious" disease of unknown aetiology. Lancet Infect Dis 2003; 3: 419-31.
Enwonwu CO, Falkler WA Jr, Idigbe EO, Afolabi BM, Ibrahim M,
Onwujekwe D. Pathogenesis of cancrum oris (noma): confounding
interactions of malnutrition with infection. Am J Trop Med Hyg
1999; 60: 223-32.
Idigbe EO, Enwonwu CO, Falkler WA, Ibrahim MM, Onwujekwe
D, Afolabi BM. Living conditions of children at risk for noma: Nigerian experience. Oral Dis 1999; 5: 156-62.
Falkler WA Jr, Enwonwu CO, Idigbe EO. Microbiological understandings and mysteries of noma (cancrum oris). Oral Dis 1999; 5:
150-55.
Falkler WA, Enwonwu CO, Ewell AJ, Idigbe EO. Isolation of
fusobacteria from the oral cavities of malnourished nigerian children living in agricultural and herding villages. Oral Dis 2000 6:
103-5.
Obiechina AE, Arotiba JT, Fasola AO. Cancrum oris (noma): level
of education and occupation of parents of affected children in Nigeria. Odontostomat Trop 2000; 23:11-14.
Barmes DE, Enwonwu CO, Leclercq MH, Bourgeois D, Falkler
WA. The need for action against oro-facial gangrene (noma). Trop
Med Int Health 1997; 2: 1111-4.
Bourgeois DM, Leclercq MH. The world health organization initiative on noma. Oral Dis 1999; 5: 172-4.
Marck KW, de Bruijn HP. Surgical treatment of noma. Oral Dis
1999; 5: 167-71.
Adekeye EO, Ord RA. Cancrum Oris: principles of management of
reconstructive surgery. J Maxillofacial Surg 1983; 1: 160-70.
Adolph HP, Yugueros P, Woods JE. Noma: a review. Ann Plast
Surg 1996; 37: 657-68.
Enwonwu CO. Noma: a neglected scourge of children in subSahara Africa. WHO Bull 1995; 73: 541-5.
Marck KW. Cancrum oris and noma: some etymological and historical remarks. Br J Plast Surg 2003; 56: 524-7.
Battus C. Handboeck der chirurgijen. Dordrecht: Abraham ende
Isaak Canin 1595.
Ritcher AL. Der Wasserkrebs der Kinder. Berlin: TFC Enslin,
1828.
Fieger A, Marck KW, Busch R, Schmidt A. An estimation of the
incidence of noma in north-west Nigeria. Trop Med Int Health
2003; 8: 402-7.
Dawson J. Cancrum oris. Br Dent J 1945; 79: 151-7.
Adelsberger L. Medical observations in auschwitz concentration
camp. Lancet 1946; 1: 317-9.
Marck KW. A history of noma, the "Face of Poverty. Plast Reconstr Surg 2003; 111: 1702-7.
World Health Organization. A disease such as noma should not
exist. noma contact. WHO publications October 1997; pp. 1-2.
World Health Organization. Noma: a vicious and deadly disease.
Noma Contact WHO 1997; p.2.
World Health Organization. Delphi expert consultation. is noma
today a public health problem? WHO/MMC/NOMA/98.1. WHO;
Geneva, Switzerland 1998.
World Health Organization. World health report, WHO, Geneva,
Switzerland 1998.
Sheiham A. An epidemiological survey of acute ulcerative gingivitis in Nigerians. Arch Oral Biol 1966; 11: 937-42.
�206 The Open Dentistry Journal, 2010, Volume 4
[26]
[27]
[28]
[29]
[30]
[31]
[32]
[33]
[34]
[35]
[36]
[37]
[38]
[39]
[40]
[41]
[42]
[43]
[44]
[45]
Ogbureke and Ogbureke
Bourgeois DM, Diallo B, Frieh C, Leclercq MH. Epidemiology of
the incidence of oro-facial noma: a study of cases in Dakar, Senegal, 1981-1993. Am J Trop Med Hyg 1999; 61: 909-13.
World Health Organization Homepage. Noma, the face of poverty.
WHO 2003; Available from: www.who.int/noma/noma_facepoverty.htm
Tempest MN. Cancrum oris. Br J Surg 1966; 53: 1071-4.
Enwonwu CO, Falkler Jr WA, Idigbe EO, Savage KO. Noma (cancrum oris): questions and answers. Oral Dis 1999; 5: 144-9.
Ndaiye FC, Bourgeois D, Leclercq MH, et al. Noma: public health
problem in senegal and epidemiological surveillance. Oral Dis
1999; 5: 163-6.
Hobdell MH. Economic globalization and oral health. Oral Dis
2001; 7: 137-43.
DeOnis M, Monteiro C, Akre J, et al. The worldwide magnitude of
protein-energy malnutrition: an overview from the WHO global database on child growth. WHO Bull 1993; 71: 703-12
Jelliffe DB. Infective gangrene of the mouth (cancrum oris). Pediatrics 1952; 9: 544-50.
Enwonwu CO. Epidemiological and biochemical studies of necrotizing ulcerative gingivitis and noma (cancrum oris) in Nigerian
children. Arch Oral Biol 1972; 17: 1357-71.
Morely D. Severe measles in the tropics I. Br Med J 1969; 1: 297300.
Morely D. Severe measles in the tropics II. Br Med J 1969; 1: 3635.
Osuji OO. Necrotizing ulcerative gingivitis and cancrum oris
(noma) in Ibadan, Nigeria. J Periodontol 1990; 61: 769-72.
Taiwo JO. Oral hygiene status and necrotizing ulcerative gingivitis
in Nigerian children. J Periodontol 1993; 64: 1071-4.
Listgarten MA, Socransky SS. Ultrastructural characteristics of a
spirochete in the lesion of acute necrotizing ulcerative gingivostomatitis (vincent's infection). Arch Oral Biol 1964; 16:95-6.
Sabiston CB Jr. A review and proposal for the etiology of acute
necrotizing gingivitis. J Clin Periodontol 1986; 13: 727-34.
Contreras A, Falkler WA Jr, Enwonwu CO, et al. Human
herpesviridae in acute necrotizing ulcerative gingivitis in children
in Nigeria. Oral Microbiol Immunol 1997; 12: 259-65.
Emslie RD. Cancrum oris. Dent Pract Dent Rec 1963; 13: 481-95.
Melnick SL, Roseman JM, Engel D, Cogen RB. Epidemiology of
acute necrotizing ulcerative gingivitis. Epidemiol Rev 1988; 10:
191-211.
Melnick SL, Alvarez JO, Navia JM, Cogen RB, Roseman JM. A
case-control study of plasma ascorbate and acute necrotizing ulcerative gingivitis. J Dent Res 1988; 67: 855-60.
Phillips RS, Enwonwu CO, Okolo S, Hassan A. Metabolic effects
of acute measles in chronically malnourished Nigerian children. J
Nutr Biochem 2004; 15: 281-8.
Received: November 23, 2009
[46]
[47]
[48]
[49]
[50]
[51]
[52]
[53]
[54]
[55]
[56]
[57]
[58]
[59]
[60]
[61]
[62]
[63]
Revised: July 10, 2010
Hussey G. Measles. In: Semba RD, Bloem MW, Eds. nutrition and
health in developing countries. Totowa, NJ: Humana Press 2001; p.
163-76.
Enwonwu CO, Phillips RS, Ferrell CD. Temporal relationship
between the occurrence of fresh noma and the timing of linear
growth retardation in Nigerian children. Trop Med Int Health 2005;
10: 65-73.
Dewhirst FE, Tamer MA, Ericson RE, et al. The diversity of periodontal spirochetes by 16S rRNA analysis. Oral Microbiol Immunol
2000; 15: 196-202.
Paster BJ, Boches SK, Galvin JL, et al. Bacterial diversity in human subgingival plaque. J Bacteriol 2001; 183: 3770-83.
Kazor CE, Mitchell PM, Lee AM, et al. Diversity of bacterial
populations on the tongue dorsa of patients with halitosis and
healthy patients. J Clin Microbiol 2003; 41: 558-63.
Uohara GI, Knapp MJ. Oral fusospirochetosis and associated lesions. Oral Surg Oral Med Oral Pathol 1967; 24: 113-23.
Horning GM. Necotizing gingivostomatitis: NUG to noma. Compend Contin Educ Dent 1996; 17: 951-4.
Enwonwu CO. Noma--the ulcer of extreme poverty. N Engl J Med
2006; 354: 221-4.
Paster BJ, Falkler WA Jr, Enwonwu CO, et al. Prevalent bacterial
species and novel phylotypes in advanced noma lesions. J Clin Microbiol 2002; 40: 2187-91.
Giessler GA, Schmidt AB. Noma: experiences with a microvascular approach under west African conditions. Plast Reconstr Surg
2003; 112: 947-54.
Adekeye EO. Ankylosis of the mandible: analysis of 76 cases. J
Oral Maxillofac Surg 1983; 41: 442-9.
Adams-Ray WE, James JH. Cancrum oris: functional and cosmetic
reconstruction in patients with ankylosis of the jaws. Br J Plast
Surg 1992; 45: 193-8.
Oluwasanmi JO, Lagundoye SB, Akinyemi OO. Ankylosis of the
mandible from cancrum oris. Plast Reconstr Surg 1976; 57: 342-50.
Tassonyi E, Lehmann C, Gunning K, Coquoz E, Montandon D.
Fiberoptically guided intubation in children with gangrenous stomatitis (noma). Anesthesiology 1990; 73: 348-9.
Kuhnel TS, Dammer R, Dunzl B, Beule AG, Strutz J. New split
scar cheek flap in reconstruction of noma sequelae. Br J Plast Surg
2003; 56: 528-33.
Nath S, Jovic G. Total loss of upper and lower lips: challenges in
reconstruction. Br J Oral Maxillofac Surg 1998; 36: 460-1.
Nath S, Jovic G. Cancrum oris: management, incidence, and implications of human immunodeficiency virus in Zambia. Plast Reconstr Surg 1998; 102: 350-7.
Montandon D, Lehmann C, Chami N. The surgical treatment of
noma. Plast Reconstr Surg 1991; 87: 76-86.
Accepted: July 19, 2010
© Ogbureke and Ogbureke; Licensee Bentham Open.
This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License
(http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the
work is properly cited.
�