Creating the Ultimate Doctor Receipt Format for Product Quality
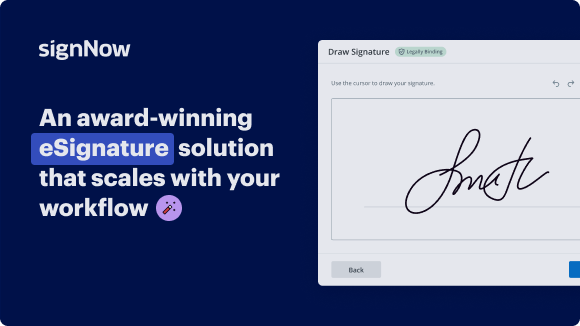
See airSlate SignNow eSignatures in action
Choose a better solution
Move your business forward with the airSlate SignNow eSignature solution
Add your legally binding signature
Integrate via API
Send conditional documents
Share documents via an invite link
Save time with reusable templates
Improve team collaboration
Our user reviews speak for themselves






airSlate SignNow solutions for better efficiency
Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.

Doctor receipt format for product quality
Creating a doctor receipt format for product quality is essential for maintaining accurate records and facilitating seamless transactions. Implementing a structured approach ensures that healthcare providers can efficiently document their services and products offered to patients, enhancing accountability and transparency in the medical field. One effective tool to accomplish this is airSlate SignNow, which provides a user-friendly platform for managing documents and signatures.
Steps to create a doctor receipt format for product quality using airSlate SignNow
- Navigate to the airSlate SignNow website in your preferred browser.
- Create a new account with a free trial or log in to your existing account.
- Select the document you wish to prepare for signing or upload a new one.
- If needed, transform your document into a reusable template for future use.
- Open the uploaded document to make necessary modifications, including adding fillable sections.
- Insert signature areas for both you and the recipients before finalizing the document.
- Proceed to set up an eSignature invitation by clicking Continue.
airSlate SignNow allows businesses to streamline the process of sending and signing documents with an efficient and budget-friendly solution. The platform offers an impressive return on investment (ROI) with a comprehensive range of tools tailored for small to mid-sized businesses. Furthermore, its straightforward pricing model ensures there are no unexpected support charges or supplementary costs.
In summary, using airSlate SignNow for your doctor receipt format enhances both productivity and professionalism. Start your free trial today to experience the benefits firsthand!
How it works
Get legally-binding signatures now!
FAQs
-
What is a doctor receipt format for product quality?
A doctor receipt format for product quality is a structured document that verifies the provision of medical services or products. It typically includes details such as the patient's name, services rendered, and the doctor's signature. Using a standardized format ensures clarity and can facilitate easier eSigning through platforms like airSlate SignNow. -
How does airSlate SignNow support the creation of a doctor receipt format for product quality?
airSlate SignNow offers robust features that allow users to easily create a doctor receipt format for product quality. With customizable templates and an intuitive drag-and-drop interface, businesses can quickly generate receipts that meet their specific needs. The platform also simplifies the eSigning process, making it efficient to obtain necessary approvals. -
What pricing options does airSlate SignNow offer for using their eSigning features?
airSlate SignNow provides various pricing tiers to accommodate different business requirements. Each plan includes features like document templates and secure eSigning that are essential for managing a doctor receipt format for product quality. You can choose a plan that best fits your organization's volume of transactions and document management needs. -
Can I integrate airSlate SignNow with other software for enhanced functionality?
Yes, airSlate SignNow seamlessly integrates with a variety of software tools, allowing you to enhance the functionality of your doctor receipt format for product quality. Popular integrations include CRM systems, project management tools, and cloud storage services. This enables a smoother workflow and more efficient management of documents. -
What are the benefits of using airSlate SignNow for documenting doctor receipts?
Using airSlate SignNow for documenting doctor receipts offers numerous benefits including increased accuracy, speed, and security. The platform allows for quick customization of the doctor receipt format for product quality, reducing the chances of errors. Furthermore, eSigning ensures that all documents are legally binding and time-stamped, providing a reliable record. -
Is it easy to customize the doctor receipt format for product quality in airSlate SignNow?
Absolutely! airSlate SignNow provides a user-friendly interface that makes it easy to customize your doctor receipt format for product quality. You can add your branding, adjust layouts, and include field requirements without needing any technical skills. This flexibility helps ensure that your receipts meet regulatory standards and your business branding. -
How secure is the data when using airSlate SignNow for doctor receipts?
Security is a top priority for airSlate SignNow, especially when handling sensitive documents like doctor receipts. The platform uses advanced encryption protocols to protect your data and ensure confidentiality. Additionally, access controls and audit trails provide further assurance that your doctor receipt format for product quality remains secure at all times.
What active users are saying — doctor receipt format for product quality
Get more for doctor receipt format for product quality
- Get Your Free Receipt Template PDF for Logistics
- Free receipt template pdf for Operations
- Get Your Free Receipt Template PDF for Planning
- Free receipt template pdf for Purchasing
- Get Your Free Receipt Template PDF for Quality Assurance
- Free receipt template pdf for Engineering
- Free Receipt Template PDF for Export
- Free receipt template pdf for Shipping
Find out other doctor receipt format for product quality
- Ensuring digital signature licitness for Toll ...
- Understanding Electronic Signature Legality for ...
- Ensuring Electronic Signature Lawfulness for Contract ...
- Understanding the Lawfulness of Electronic Signatures ...
- Unlocking the Power of Electronic Signature Legitimacy ...
- Enhance Freelance Contract Legitimacy with Electronic ...
- Electronic Signature Legitimateness for Contracts in ...
- Ensuring Electronic Signature Legitimateness for ...
- Enhance Electronic Signature Legitimateness for Home ...
- Maximize Electronic Signature Legitimateness for Stock ...
- Electronic Signature Legitimateness for Manufacturing ...
- The Legitimacy of Electronic Signatures for Personal ...
- Electronic Signature Licitness for Property Inspection ...
- Online Signature Legality for Forms in India Boost Your ...
- Unlock the Power of Online Signature Legality for ...
- Online Signature Legality for Contracts in United ...
- Unlocking the Power of Online Signature Legality for ...
- Unlock the Power of Legally Binding Online Signatures ...
- Unlock Online Signature Lawfulness for Contracts in ...
- Unlock the power of electronic signature in PDF with ...