Create a Payment Reminder Sample for Product Quality Effortlessly
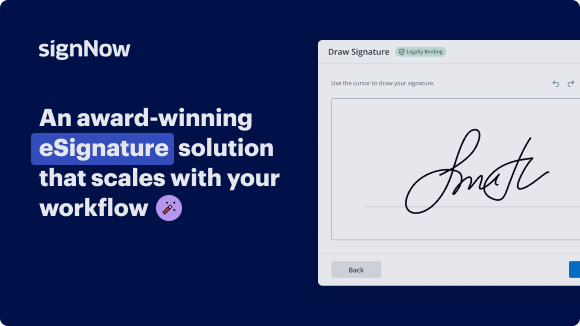
See airSlate SignNow eSignatures in action
Choose a better solution
Move your business forward with the airSlate SignNow eSignature solution
Add your legally binding signature
Integrate via API
Send conditional documents
Share documents via an invite link
Save time with reusable templates
Improve team collaboration
Our user reviews speak for themselves






airSlate SignNow solutions for better efficiency
Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.

Payment reminder sample for Product quality
When managing product quality, timely communication can signNowly enhance relationships with partners and customers. One effective approach to ensure accountability is by sending payment reminders. Utilizing tools like airSlate SignNow allows businesses to seamlessly send eSignature invites for their documents. Follow the guide below to maximize your payment reminders utilizing airSlate SignNow's efficient features.
Payment reminder sample for Product quality
- Open your web browser and navigate to the airSlate SignNow homepage.
- Register for a complimentary trial or log into your existing account.
- Select the document that requires signing or needs to be sent for e-signatures and upload it.
- If you plan to use this document multiple times, save it as a reusable template.
- Access your document to make necessary modifications: add fillable sections or input required information.
- Insert your signature and designate fields for the recipients' signatures.
- Proceed by clicking Continue to arrange and send out your eSignature invitation.
By incorporating airSlate SignNow in your workflow, you empower your organization with a budget-friendly solution that greatly enhances document management efficiency.
With user-friendly features, transparent pricing, and robust customer support available 24/7 for all paid plans, consider leveraging airSlate SignNow for your payment reminder needs today!
How it works
Get legally-binding signatures now!
FAQs
-
What is a payment reminder sample for product quality?
A payment reminder sample for product quality is a template designed to remind clients about their outstanding payments while emphasizing the quality of the product they received. By integrating this sample into your business communications, you can maintain a professional relationship while ensuring timely payments for services rendered. -
How can airSlate SignNow help me create a payment reminder sample for product quality?
airSlate SignNow offers customizable templates that allow businesses to create a payment reminder sample for product quality easily. The platform's user-friendly interface ensures that you can tailor reminders to fit your brand's communication style and highlight product quality effectively. -
What features does airSlate SignNow offer for managing payment reminders?
With airSlate SignNow, you can automate payment reminders, track document statuses, and send personalized messages. These features ensure that your payment reminder sample for product quality signNowes your clients promptly, enhancing your cash flow management and client relationships. -
Can I integrate airSlate SignNow with my existing CRM for payment reminders?
Yes, airSlate SignNow supports integrations with various CRM systems, allowing you to manage your payment reminder sample for product quality seamlessly. This integration ensures that all client interactions are consistent and that reminders are sent automatically based on your CRM's data. -
Are there any costs associated with using airSlate SignNow for payment reminders?
airSlate SignNow offers competitive pricing plans that cater to different business needs. Whether you're a small business or a large enterprise, you can find a plan that fits your budget while still providing a robust solution for sending a payment reminder sample for product quality. -
How does a payment reminder sample for product quality improve customer relations?
Sending a payment reminder sample for product quality shows that you value your clients and their experience with your product. By framing reminders positively and professionally, you not only prompt timely payments but also enhance customer satisfaction and loyalty. -
What advantages does using an electronic signature for payment reminders have?
Using electronic signatures with airSlate SignNow for payment reminders streamlines the approval process, making it quicker and more efficient. This not only saves time but also provides a secure and legally binding way to confirm transactions related to your payment reminder sample for product quality.