Discover the Perfect Weekly Billing Format for Supervision
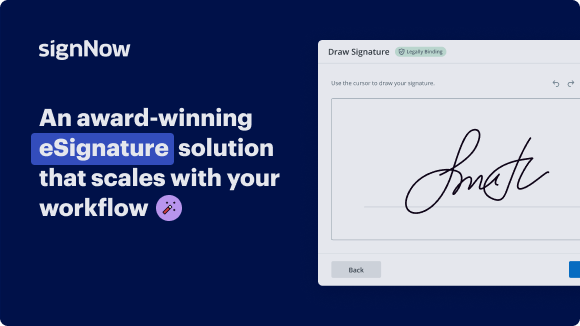
See airSlate SignNow eSignatures in action
Choose a better solution
Move your business forward with the airSlate SignNow eSignature solution
Add your legally binding signature
Integrate via API
Send conditional documents
Share documents via an invite link
Save time with reusable templates
Improve team collaboration
Our user reviews speak for themselves






airSlate SignNow solutions for better efficiency
Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.

Weekly billing format for supervision
The weekly billing format for supervision is essential for businesses seeking streamlined operations and improved accountability. When utilizing tools like airSlate SignNow, organizations can enhance their document processes while keeping costs transparent and manageable. This guide will walk you through the easy steps to utilize airSlate SignNow’s features effectively, ensuring you can take full advantage of its benefits for weekly billing processes.
Weekly billing format for supervision
- Visit the airSlate SignNow website in your preferred browser.
- Create a free trial account or log into your existing one.
- Select the document you wish to sign or send out for signing.
- Transform the document into a reusable template for future use if desired.
- Access the document for any necessary edits: add fillable fields or input additional information.
- Add your signature and specify signature fields for the recipients.
- Proceed to finalize the setup and send out an eSignature invitation for your document.
By following these steps, you'll be able to effectively manage your documentation, making the process of overseeing weekly billing more efficient. airSlate SignNow not only simplifies the signing process but also saves both time and resources, all while maintaining transparency in costs.
Start your free trial today and discover how airSlate SignNow can transform your business operations!
How it works
Get legally-binding signatures now!
FAQs
-
What is a weekly billing format for supervision in airSlate SignNow?
The weekly billing format for supervision in airSlate SignNow allows businesses to effectively manage and track billing cycles on a weekly basis. This format ensures that supervisors can maintain clear oversight of payments and services rendered, leading to improved financial organization. -
How does airSlate SignNow support the weekly billing format for supervision?
airSlate SignNow supports the weekly billing format for supervision by offering customizable templates that streamline the process of invoicing. You can easily create and send documents, ensuring that all relevant billing information is captured systematically, enhancing overall efficiency. -
Can I integrate my accounting software with airSlate SignNow for the weekly billing format for supervision?
Yes, airSlate SignNow integrates seamlessly with various accounting software, enabling you to utilize the weekly billing format for supervision. This integration simplifies the workflow, as financial data can be transferred automatically, reducing manual effort and potential errors. -
What are the benefits of using airSlate SignNow's weekly billing format for supervision?
Using the weekly billing format for supervision in airSlate SignNow helps businesses improve cash flow management and ensures timely payments. It also facilitates better planning and forecasting, allowing supervisors to make informed decisions based on consistent billing cycles. -
Are there templates available for a weekly billing format for supervision?
airSlate SignNow provides a variety of templates that can be tailored to fit the weekly billing format for supervision. These templates are designed to simplify document creation, making it easy to generate professional invoices quickly and accurately. -
What features does airSlate SignNow offer for managing the weekly billing format for supervision?
airSlate SignNow includes features such as eSignature capabilities, automated reminders, and tracking functionalities, all of which enhance the administration of the weekly billing format for supervision. These tools ensure that all parties are engaged and informed throughout the billing process. -
Is airSlate SignNow suitable for small businesses using a weekly billing format for supervision?
Absolutely! airSlate SignNow is designed to be cost-effective and user-friendly, making it an ideal solution for small businesses implementing a weekly billing format for supervision. Its affordable pricing and ease of use help smaller teams operate efficiently without extensive resources.
What active users are saying — weekly billing format for supervision
Get more for weekly billing format for supervision
- Rent invoice template word for small businesses
- Rent Invoice Template Word for Teams
- Rent invoice template word for organizations
- Rent Invoice Template Word for NPOs
- Rent invoice template word for non-profit organizations
- Sample Business Invoice for Businesses
- Sample business invoice for corporations
- Sample Business Invoice for Enterprises
Find out other weekly billing format for supervision
- Easily add signature to PDF without Acrobat for ...
- Discover free methods to sign a PDF document online ...
- How to add electronic signature to PDF on iPhone with ...
- How to sign PDF files electronically on Windows with ...
- How to sign a PDF file on phone with airSlate SignNow
- Experience seamless signing with the iPhone app for ...
- Easily sign PDF without Acrobat for seamless document ...
- Easily email a document with a signature using airSlate ...
- How to sign a document online and email it with ...
- How to use digital signature certificate on PDF ...
- How to use e-signature in Acrobat for effortless ...
- How to use digital signature on MacBook with airSlate ...
- Discover effective methods to sign a PDF online with ...
- Effortlessly sign PDFs with the linux pdf sign command
- Easily sign PDF documents on Windows with airSlate ...
- Easily sign a PDF file and email it back with airSlate ...
- Effortlessly sign PDF documents on phone
- Sign PDF document with certificate effortlessly
- Easily signing a PDF document on my iPhone
- Sign PDF online with electronic signature easily and ...