Pharmacy 101
Your Pharmacy Benefits Guide
This guide can
help answer your
questions and
clarify some
pharmacy terms.
05.03.376.1 A (9/10)
�Pharmacy glossary of terms
You may find yourself asking questions about your health care coverage. What
is a copayment? How do I know what drugs are covered? What should I ask
my doctor when he or she writes me a new prescription? This guide can help
answer your questions and clarify some pharmacy terms. If you have any other
questions, please visit www.aetna.com. Or call Member Services at the
toll-free number on your Aetna ID card.
Annual Notice of Change
Closed formulary
Deductible
A letter sent to members in certain plans
that tells them about any upcoming changes
to their prescription drug plan. The letter is
sent at the end of every year and affects
drugs in the next plan year.
A prescription benefits plan that does not
cover drugs on the Aetna Formulary
Exclusions list without a medical exception.
The amount you pay for prescriptions
before your health plan begins to pay.
For example, your plan might have a
$1,500 deductible.
Benefit
The percentage of the negotiated cost of your
prescription drug you pay after you have
finished paying your deductible. Your health
plan pays the rest. For example, you might
pay 10 percent of the negotiated drug cost.
The services, drugs and products covered by
your health benefits and health insurance
plan. This word is also used to describe your
health plan in general.
Brand-name drug
A drug that is marketed under a specific
trade name by a drug-maker. In most cases,
these drugs are still under patent protection.
This means that the drug-maker is the only
manufacturer of this medication.
Chronic condition
A condition that lasts or keeps coming back
over a long period of time. These conditions
may be treated with maintenance medications.
Coinsurance
Complex chronic condition
A chronic condition that may require you to
take specialty medications. Examples are
medications used to treat rheumatoid
arthritis and multiple sclerosis.
Copay/copayment
The dollar amount you pay for your
prescriptions after you have finished paying
your deductible. For example, your plan might
say that you pay $25 for brand-name drugs.
Aetna is the brand name used for products and services provided by one or more of
the Aetna group of subsidiary companies. The Aetna companies that offer, underwrite
or administer benefits coverage include: Aetna Health Inc., Aetna Health of California
Inc., Aetna Health Insurance Company of New York, Aetna Health Insurance Company
and/or Aetna Life Insurance Company (Aetna). In Maryland, by Aetna Health Inc., 151
Farmington Avenue, Hartford, CT 06156. Aetna Pharmacy Management refers to an
internal business unit of Aetna Health Management, LLC. Aetna Specialty Pharmacy
and Aetna Rx Home Delivery respectively refer to Aetna Specialty Pharmacy, LLC and
Aetna Rx Home Delivery, LLC which are subsidiaries of Aetna Inc. Each insurer has sole
financial responsibility for its own products.
Dependent
A family member who is covered by
your plan. It can be a child, spouse or
domestic partner.
Drug
A natural, live, or man-made ingredient
used to treat an illness. “Medication” is
another commonly used term.
Drug tiers
Tiers are coverage levels. Often, tiers
have different out-of-pocket costs.
Depending on your plan, you might see
the tiers grouped by generic, brandname, preferred or non-preferred drugs.
Exclusion
A drug, product or service that is not
covered by your plan.
�Flexible Spending Account (FSA)
Health Savings Account (HSA)**
Open enrollment
A way to set aside money to pay for your
health care or prescriptions while saving
money on taxes. Money is taken from your
paycheck and placed into a fund. You can
use the fund to pay for health care costs
throughout the plan year. FSAs have a time
limit. This means the money must be used in
the same plan year.
Part of a health plan that helps you pay for
prescriptions and other health care costs.
You and your employer can put money into
this account. Or you can save money in the
account for future health care costs. The
account grows interest.
The time period when you can make
choices about your health plan coverage
for the next year.
Formulary
Also known as the “Preferred Drug List.”
It is a list of medications preferred by Aetna
prescription benefit plans. The Preferred Drug
List is not a complete list of medications
covered under the benefit plan. Some benefit
plans may not cover certain medications on
this list, such as contraceptives, infertility
drugs and diabetic supplies.
Generic drug
A “copy” of a brand-name drug. It has the
same basic ingredients that a brand drug
does. Plus, the FDA has found that it is just
as safe and effective as the brand drug.
Generic drugs usually cost less than brand
drugs, which means you may save money
by choosing generics.
Health Reimbursement
Arrangement (HRA)*
Part of a health plan that gives you money to
pay for prescriptions and other health care
costs. Your employer puts money into a
fund. You can use the fund to pay out-ofpocket costs, like your copays, or
deductibles. Unused money is rolled over
and can be used in the next plan year.
ID card
The card you get that shows you are a
member when you join a health plan.
Show it to your pharmacist to access your
prescription drug benefits.
Limitations
Restrictions put into place based on the
coverage options chosen by the plan
sponsor. They define what the benefit plan
does or doesn’t cover or things that must be
done before something is covered.
Mail-order pharmacy
A convenient service that lets you get
medications through the mail. Aetna Rx
Home Delivery® is the name of Aetna’s
mail-order pharmacy. Often you can save
money by using a mail-order pharmacy.
Maintenance medications
Prescription drugs that are taken on a
regular basis. These drugs help treat chronic
conditions like high blood pressure.
Medicare Part D
A Medicare Prescription drug benefit.
*HRAs are currently not available to HMO members in IL and Small Group members in FL.
**HSAs are currently not available to HMO members in IL and CA.
Open formulary
A prescription benefits plan that
covers all eligible prescription drugs.
Out-of-pocket costs
Any costs that you must pay a portion
of for your health care. Copays,
coinsurances and deductibles are
examples.
Out-of-pocket maximum
A limit on the costs you must pay for
covered services after you meet your
deductible. Your plan pays 100 percent
of the costs of covered services for you
after you reach this amount. The limit
usually comes up yearly.
Over-the-counter drugs
Drugs that can be bought without a
prescription. They are not covered under
most prescription benefits plans. Aspirin,
ibuprofen, Prilosec OTC and cold
remedies are examples.
Participating pharmacy
A pharmacy that has a contract with
your health plan. You can use a
participating pharmacy to fill your
prescriptions.
�Pharmacy network
Specialty medications
Precertification
Each participating pharmacy belongs to a
pharmacy network. A network is a group of
pharmacies that has a contract with your health
plan. A network pharmacy provides services at
a special reduced rate for our members.
Drugs taken for complex chronic conditions
like rheumatoid arthritis or HIV. These drugs
are most often injected, given through an IV
or taken by mouth.
A process in which you must get prior
approval before certain drugs or services
are covered.
Prescription
Instructions given by a doctor or other
health care provider that directs the care for
a patient. Prescriptions may include direction
for the patient, caregiver, nurse, pharmacist
or other therapist.
Prescription drug
A drug that is regulated by the Food
and Drug Administration that requires
a prescription before it can be bought.
The term is used to separate it from
over-the-counter drugs, which don’t
require a prescription.
Retail pharmacy
A community pharmacy where you can
order and pick up prescription drugs.
Rx
A symbol that means “prescription” or
“pharmacy.”
These drugs can cost more and require more
monitoring than other types of drugs. And they
may not be available at retail pharmacies.
Specialty pharmacy*
A type of pharmacy that dispenses specialty
medications. Aetna Specialty Pharmacy® is
the name of Aetna’s specialty pharmacy. It
delivers specialty medications by mail and
offers in-depth patient support from a
team of nurses and pharmacists.
*� etna Specialty Pharmacy and the Specialty
A
Pharmacy Network may not be available to
California HMO members. Talk to your doctor
about the appropriate way to get the specialty
medications you need. Doctors may have
agreed to dispense and administer drugs to you
themselves. Or they may write a prescription so
you can fill them at any participating retail or
mail-order pharmacy you choose.
Quantity Limits
Limits placed on drugs so that they are
not taken in amounts that are higher
than recommended by medical
guidelines or the Food and Drug
Administration.
Step-therapy
With this program, trying one or more
prerequisite drugs is required before
other medications will be covered.
Therapeutic duplication
This happens when two drugs of the
same type are prescribed at the same
time. Rarely are two drugs from the
same category necessary to treat a
medical condition. Taking these drugs
at the same time may be harmful to
your health.
�Aetna terms
Aetna Formulary Exclusions List
Aetna Rx Home Delivery
The part of a prescription benefits and
insurance plan that names drugs that are
only covered if you have a medical exception.
Aetna’s mail-order pharmacy. Members may
be able to order up to a 90-day supply of
maintenance medications at a time.
Aetna Pharmacy Management
Aetna Specialty Pharmacy
The division that manages Aetna prescription
benefits and insurance plans.
Aetna Specialty Pharmacy is available for
members to fill their specialty medications. It
provides self-injectable, infused, compounded
and select oral drugs. Patients also get
in-depth support throughout their treatment.
Aetna Preferred Drug List
Also known as a “formulary.” This is a list of
medications preferred by Aetna prescription
benefit plans. The Preferred Drug List is not a
complete list of covered medications. Some
plans may not cover certain medications on
this list, such as contraceptives, infertility
drugs and diabetic supplies.
Secure Member Website
Visit www.aetna.com and log in to your
secure member website, Aetna Navigator®.
You’ll find tools and resources to help you
learn more about your pharmacy benefits
and claims.
�Pharmacy benefits in action
Pharmacy — the most accessed
health benefit
Chances are you use your pharmacy benefits
more than any other part of your health
plan. You may need to take medication every
day for high blood pressure. Or you may
need to pick up antibiotics for your child’s
ear infection. Either way, when medical
issues come up, you may need prescription
drugs. When this happens, you need to
consider a few things:
� hat should you know about these
W
medications before you get them
from a pharmacy?
■
� ow should you take your medication?
H
By mouth? Before bed? With food?
■
� hould you get your prescriptions through
S
the mail?
■
� hould you get a generic drug?
S
■
� re you paying the lowest possible cost?
A
■
As you can see, understanding how your
benefits work is important to know how
to get the most out of them.
What prescription drugs are
covered?
Many Aetna prescription drug plans offer
coverage based on our Preferred Drug List
(also known as a formulary). Depending
upon the benefit plan, the Preferred Drug
List may provide different levels of coverage
for preferred and non-preferred drugs. The
Preferred Drug List includes both generic
and brand-name drugs. The list is regularly
reviewed and may change in response to
new drugs to the market, medical guidelines
and information from the Food and Drug
Administration and drug-makers.
To see what your plan covers, log in to
www.aetna.com. Then look for Medication
Search. From there, you can enter the name
of a brand-name or generic drug. You can
see if your drug is covered, the tier your drug
is on and if a generic equivalent is available.
What should you do if your
doctor prescribes a medication
that isn’t covered by your plan
or is too costly?
When your doctor gives you a
prescription, ask him or her a few
questions about it.
■
� hat does this drug do?
W
■
�s it right for you?
I
■
� ould a generic be appropriate?
W
■
�s there a less costly alternative?
I
Choosing a medication on a lower tier
or a generic drug may help save you
money. If your plan has one, you may
want to bring a copy of your Aetna
Preferred Drug guide to your doctor’s
office. That way, you can see if the drug
is covered. Ultimately, decisions about
your care are up to you and your doctor.
Are generic drugs right for me?
Generic drugs can help you get more
for your health care dollars. They are
generally less expensive than brandname drugs, but they do the same job.
That’s why we encourage you and your
doctor to consider generic medications
whenever possible.
Generic drugs are approved by the FDA
to be as safe and effective as their
brand-name counterparts. They have
the same active ingredients in the same
dose. The difference is that they may be
another size or color.
�What do I have to do at the
pharmacy to get the generic
version of a drug?
Most pharmacies can substitute a generic
drug for a brand-name drug. In fact, many
will make the switch automatically, unless
your state law says they can’t.
However, your doctor may have written
“DAW” on your prescription. This stands for
“dispense as written.” It means that the
pharmacy can’t give you a generic drug
instead of a brand-name one without calling
your doctor. Your doctor may do this if he or
she believes that the generic medication is
not right for you.
How can I find out how much a drug
will cost?
Most people like to know how much their
medication is going to cost them before they
get to the pharmacy. If you have Internet
access, you can use our Price-A-DrugSM tool
on your secure member website to find out
your estimated medication costs. Log in at
www.aetna.com and click on “Prescription
Drug Costs”. From there, enter the name of
your prescription and your dose. The tool
will also show you how much you could save
by using our mail-order pharmacy.
If you don’t have access to the Internet, you
can always call Member Services. The
toll-free number is on your Aetna ID card.
How do I start using Aetna Rx Home
Delivery?
There are a few ways to get
started:
Aetna Rx Home Delivery is a convenient,
cost-effective way to get your medications
through the mail. And it might be part of
your plan. To start taking advantage of
Aetna Rx Home Delivery, just follow these
easy steps:
■
� ill out a Patient Profile Form. Then
F
send it in along with your prescription.
Visit www.AetnaSpecialtyRx.com
and click “Enroll” to access this form
and directions to submit it; or
■
� sk your doctor to fill out a
A
Medication Request form. Then ask
him or her to fax it with your
prescription to 1-866-FAX-ASRX
(1-866-329-2779). Doctors can visit
www.AetnaSpecialtyPharmacy.com
and click “Find our forms” to access the
needed form; or
■
� o transfer a prescription to Aetna
T
Specialty Pharmacy, have your current
pharmacy call our pharmacy toll-free
at 1-866-782-2779. Or, ask your
doctor to call or fax in your specialty
prescriptions to us.
� tep 1: Ask your doctor for a prescription
S
for each maintenance medication you or a
family member is taking (typically a 90-day
supply).
■
� tep 2: Complete and mail an order form
S
and new patient registration form, along
with your new prescriptions and method
of payment, to Aetna Rx Home Delivery.
■
� r: Have your doctor fax your prescriptions
O
to Aetna Rx Home Delivery.
■
For forms, mailing information and telephone
numbers, please go to www.aetna.com
and log in to your secure member website,
Aetna Navigator. Or call Member Services
toll-free at the number on your Aetna ID card.
How do I start using Aetna Specialty
Pharmacy?
If your plan includes Aetna Specialty
Pharmacy, you can get specialty medications
through the mail. You can also get support
from nurses and pharmacists for your
complex condition 24 hours a day, 7 days a
week.
What online tools can I use to
manage my prescription drug
benefits?
Your secure member website has many
different tools to use to take care of
your family’s prescription drug needs:
■
� enefits Summary Look through
B
—
your prescription benefits to find out
what’s covered.
� laim Search — Locate drug claims
C
and cost information in one place.
■
� rice-A-Drug — Find cost
P
information with just a few clicks.
■
� edication Search — Look up
M
coverage information about your drug.
■
� ind A Pharmacy — Enter your ZIP
F
code to find a participating pharmacy
near you.
■
� martSourceSM — Find personalized
S
information about your conditions,
treatments and costs.
■
�The term precertification means the utilization review process used to determine whether the
requested service, procedure, prescription drug or medical device meets Aetna’s clinical criteria for
coverage. It does not mean precertification as defined by Texas law, as a reliable representation of
payment of care or services to fully insured HMO and PPO members. Step-therapy and precertification
may not apply in all service areas. For example, step-therapy and precertification programs do not
apply to fully insured members in Indiana. Step-therapy is also not available for fully funded groups
in New Jersey. California HMO members who are receiving coverage for medications that are added
to the precertification or step-therapy lists will continue to have those medications covered for as
long as the treating physician continues prescribing them, provided that the drug is appropriately
prescribed and is considered safe and effective for treating the enrollee’s medical condition.
This material is for information only and is not an offer or invitation to contract. Health benefits
and health insurance plans contain exclusions and limitations. Aetna Rx Home Delivery and
Aetna Specialty Pharmacy refer to Aetna Rx Home Delivery, LLC and Aetna Specialty Pharmacy,
LLC respectively. Aetna Rx Home Delivery and Aetna Specialty Pharmacy are licensed pharmacy
subsidiaries of Aetna Inc. that operate through mail order. Aetna HealthFund HRAs are subject
to employer-defined use and forfeiture rules and are unfunded liabilities of your employer. Fund
balances are not vested benefits. Investment services are independently offered through JPMorgan
Institutional Investors, Inc., a subsidiary of JPMorgan Chase Bank. For Small Group, investments are
independently offered through HealthEquity, Inc. Aetna receives rebates from the manufacturers of
many drugs, including many that are on the Preferred Drug List. These rebates do not reduce the
amount you pay for an individual prescription drug. However, they help control the overall costs
of prescription drug coverage. Your pharmacy benefit provides coverage for many drugs that are
not on this list. Also, in some cases, if you need to pay a percentage of the cost of the drug or an
amount to meet a deductible, your costs may be higher for a “preferred drug” than they would be
for a “non-preferred drug.” You can find out more about the terms and limitations on your plan by
reading your plan documents. You can also contact Member Services.
Policy forms issued in OK include: HMO OK COC-5 09/07, HMO/OK GA-3 11/01, HMO OK POS
RIDER 08/07, GR-23 and/or GR-29/Gr-29N.
Information is believed to be accurate as of the production date. However, it is subject to change.
For more information about Aetna plans, refer to www.aetna.com.
05.03.376.1 A (9/10)
©2010 Aetna Inc.
�
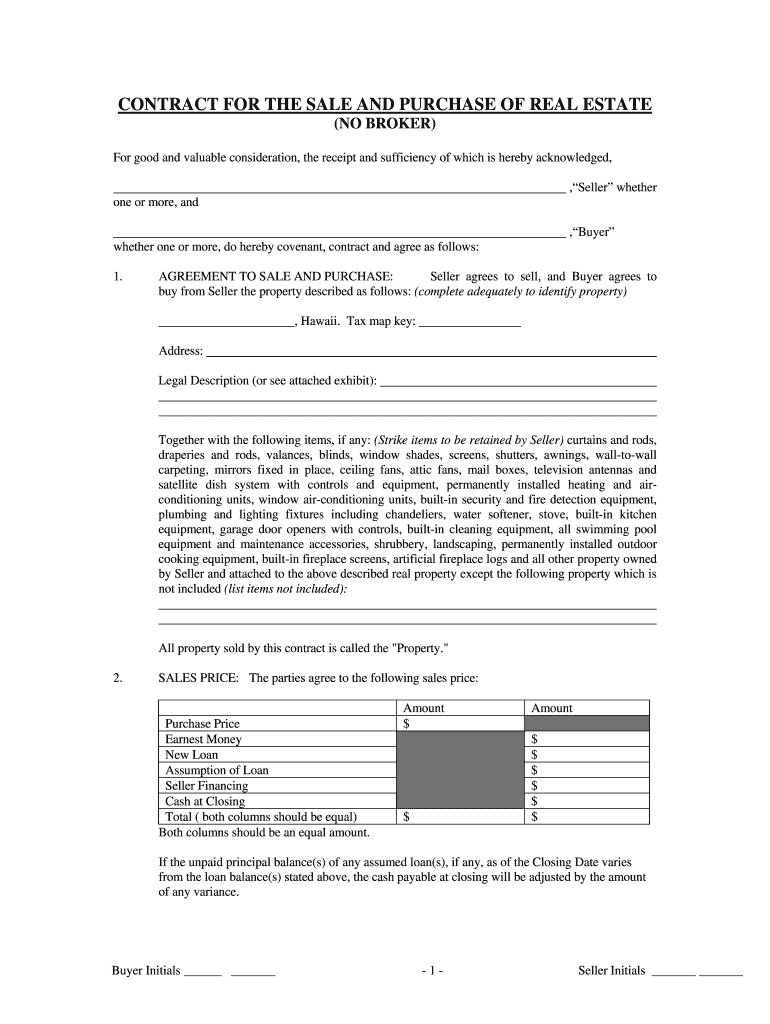
Useful tips on finishing your ‘Sale Land Agreement Form For Hawaii’ online
Are you fed up with the burden of handling documents? Look no further than airSlate SignNow, the premier eSignature solution for individuals and small to medium-sized businesses. Bid farewell to the tedious routine of printing and scanning documents. With airSlate SignNow, you can effortlessly complete and sign documents online. Leverage the comprehensive tools available in this user-friendly and affordable platform and transform your method of document management. Whether you need to authorize forms or gather signatures, airSlate SignNow manages it all effortlessly, with just a few clicks.
Follow this detailed guide:
- Sign in to your account or sign up for a complimentary trial with our service.
- Click +Create to upload a file from your device, cloud storage, or our form library.
- Access your ‘Sale Land Agreement Form For Hawaii’ in the editor.
- Click Me (Fill Out Now) to set up the document on your end.
- Add and allocate fillable fields for others (if necessary).
- Continue with the Send Invite options to request eSignatures from others.
- Download, print your version, or convert it into a reusable template.
Don’t be concerned if you need to collaborate with your colleagues on your Sale Land Agreement Form For Hawaii or send it for notarization—our platform provides all you require to achieve such tasks. Register with airSlate SignNow today and enhance your document management to new levels!