Signature Nursing Visit Report Form Made Easy
Do more on the web with a globally-trusted eSignature platform
Remarkable signing experience
Reliable reporting and analytics
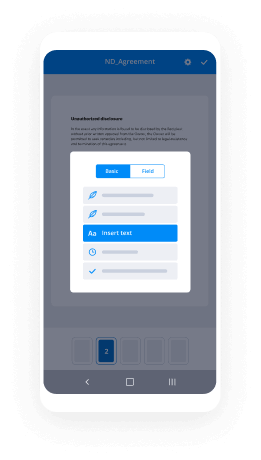
Mobile eSigning in person and remotely
Industry polices and conformity
Signature nursing visit report form, faster than ever before
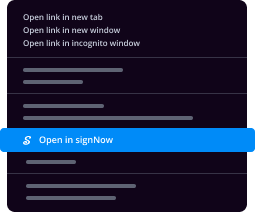
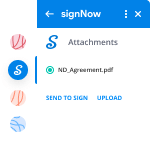
Helpful eSignature extensions
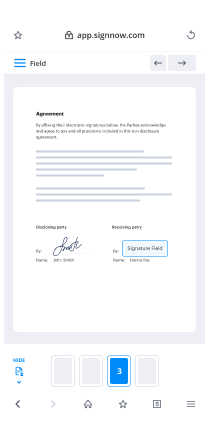
See airSlate SignNow eSignatures in action
airSlate SignNow solutions for better efficiency
Our user reviews speak for themselves






Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.

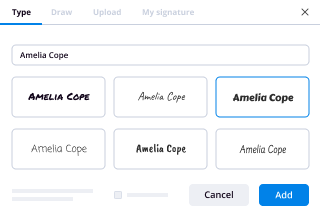
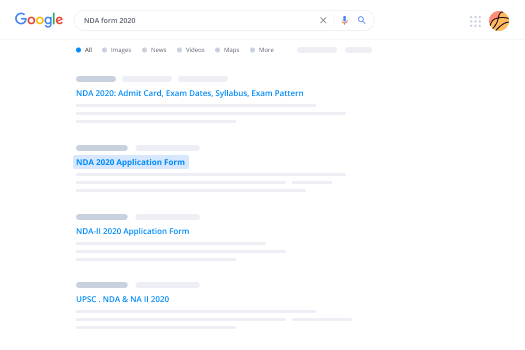
Your step-by-step guide — signature nursing visit report form
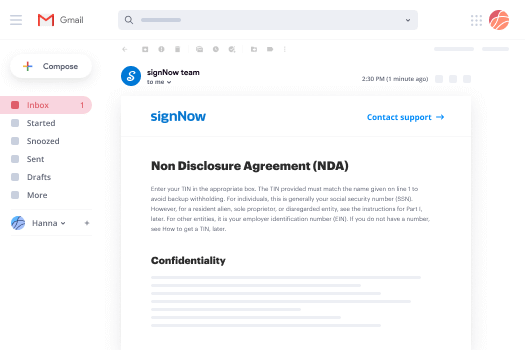
Employing airSlate SignNow’s eSignature any organization can speed up signature workflows and eSign in real-time, providing an improved experience to customers and staff members. Use signature Nursing Visit Report Form in a couple of easy steps. Our handheld mobile apps make working on the run feasible, even while offline! Sign documents from any place in the world and complete tasks quicker.
Take a stepwise instruction for using signature Nursing Visit Report Form:
- Log on to your airSlate SignNow account.
- Find your needed form in your folders or upload a new one.
- Access the record and edit content using the Tools list.
- Drop fillable areas, add textual content and eSign it.
- Add numerous signers via emails and set the signing sequence.
- Specify which individuals will get an executed version.
- Use Advanced Options to reduce access to the record add an expiry date.
- Press Save and Close when finished.
Moreover, there are more enhanced features available for signature Nursing Visit Report Form. Add users to your shared digital workplace, view teams, and track collaboration. Numerous consumers across the US and Europe agree that a system that brings people together in one unified digital location, is the thing that organizations need to keep workflows functioning smoothly. The airSlate SignNow REST API allows you to integrate eSignatures into your application, internet site, CRM or cloud. Check out airSlate SignNow and enjoy quicker, smoother and overall more productive eSignature workflows!
How it works
airSlate SignNow features that users love
See exceptional results signature Nursing Visit Report Form made easy
Get legally-binding signatures now!
FAQs
-
How do you write a nursing report?
State your position clearly. Write the reason why you are creating a report. Provide an example or at least two to show your position. Support your decision with statistics and facts. As much as possible, keep your report short and concise. -
What should a transfer report include?
Capstone Review Funds List the pertinent information that should be included in a transfer report. \uf0b7 Age, Sex, medical diagnosis, recent vital signs and medications, allergies, special equipment, and code status. -
How do you write a good nursing report?
State your position clearly. Write the reason why you are creating a report. Provide an example or at least two to show your position. Support your decision with statistics and facts. As much as possible, keep your report short and concise. -
What is recording and reporting in nursing?
Report summarizes the services of the nurse and/ or the agency. Reports may be in the form of an analysis of some aspect of a service. These are based on records and registers and so it is relevant for the nurses to maintain the records regarding their daily case load, service load and activities. -
What is reporting in nursing?
REPORTS are oral or written exchange of information shared between care givers ( Health care team) in a number of ways. ... Nurses communicate information about client's/ patient's so that all health care team members can make appropriate decision making about client's care. -
What is the importance of report writing in nursing?
Report writing in nursing allows for the better provision of information about patients under the care of a particular nurse. The information on a patient in the chart records but it is more practical when it is in a brief synopsis showing situation, background and assessment of a patient. -
Why is nursing writing important?
Writing is essential in nursing and it reflects the activity of medical workers in the healthcare field. It helps them to organize their work properly and care about every patient with great attention and monitor his or her condition. -
How do you create a medical questionnaire?
The key steps in designing a questionnaire are to: decide what data you need, select items for inclusion, design the individual questions, compose the wording, design the layout and presentation, think about coding, prepare the first draft and pretest, pilot, and evaluate the form, and perform the survey. -
What is a health history questionnaire?
Health history questionnaire (online) Have your patients fill out this questionnaire template online prior to their first appointment. The form has sections for personal health history, health habits and personal safety, family health history, mental health, women only, men only, and other problems. -
How do you write a questionnaire?
Know your question types. Keep it brief, when possible. Choose a simple visual design. Use a clear research process. Create questions with straightforward, unbiased language. Ensure every question is important. Ask one question at a time. Order your questions logically. -
How do you write a survey questionnaire?
Use Simple, Direct Language. ... Be Specific. ... Break Down Big Ideas into Multiple Questions. ... Avoid Leading Questions. ... Ask One Thing per Question. ... Use More Interval Questions. -
Why is documentation so important in nursing?
Nurses document their work and outcomes for a number of reasons: the most important is for communicating within the health care team and providing information for other professionals, primarily for individuals and groups involved with accreditation, credentialing, legal, regulatory and legislative, reimbursement, ... -
Why is documentation important in health care?
Proper documentation, both in patients' medical records and in claims, is important for three main reasons: to protect the programs, to protect your patients, and to protect you the provider. ... Good documentation is important to protect your patients. Good documentation promotes patient safety and quality of care. -
Why is record keeping important in healthcare?
When caring for a patient, it is important to ensure good record keeping to promote patient care and better communication. Good record keeping is a product of good teamwork and an important tool in developing high-quality healthcare and reinforcing professionalism within nursing. -
What is effective documentation in nursing?
Clear, accurate, and accessible documentation is an essential element of safe, quality, evidence-based nursing practice. ... Documentation of nurses' work is critical as well for effective communication with each other and with other disciplines.