eSignature Professional Physical Therapy Consent Template Made Easy
Do more on the web with a globally-trusted eSignature platform
Outstanding signing experience
Robust reports and analytics
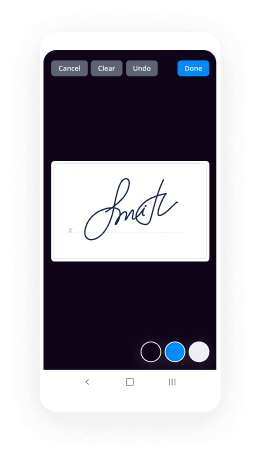
Mobile eSigning in person and remotely
Industry rules and conformity
E signature professional physical therapy consent template, quicker than ever before
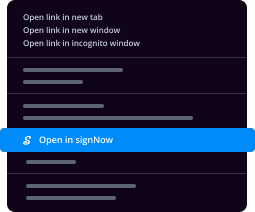
Useful eSignature add-ons
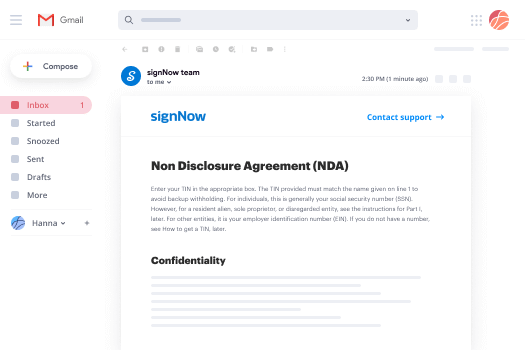
See airSlate SignNow eSignatures in action
airSlate SignNow solutions for better efficiency
Our user reviews speak for themselves






Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.

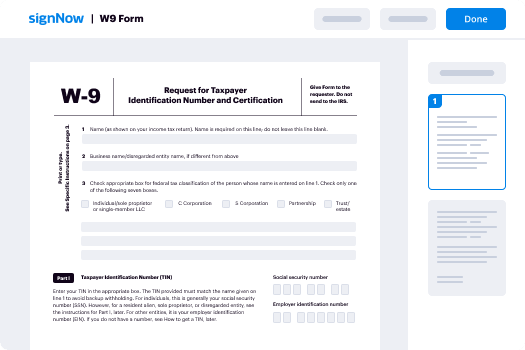
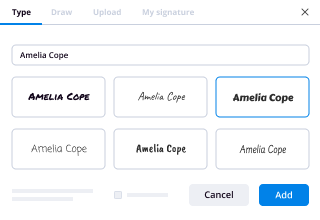
Your step-by-step guide — e signature professional physical therapy consent template
Using airSlate SignNow’s eSignature any company can speed up signature workflows and sign online in real-time, giving a greater experience to consumers and workers. Use eSignature Professional Physical Therapy Consent Template in a few simple actions. Our handheld mobile apps make working on the run achievable, even while off-line! eSign signNows from any place worldwide and make trades in less time.
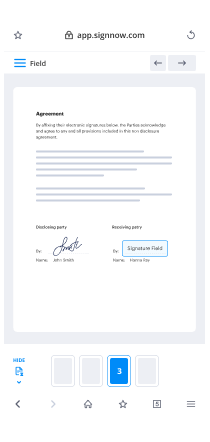
Follow the walk-through guide for using eSignature Professional Physical Therapy Consent Template:
- Log on to your airSlate SignNow account.
- Find your needed form within your folders or upload a new one.
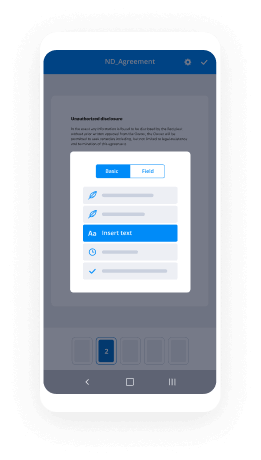
- Open the document adjust using the Tools menu.
- Drag & drop fillable fields, add textual content and sign it.
- Include several signers using their emails and set the signing sequence.
- Indicate which recipients will get an signed version.
- Use Advanced Options to limit access to the document add an expiry date.
- Press Save and Close when completed.
Moreover, there are more enhanced functions accessible for eSignature Professional Physical Therapy Consent Template. List users to your common work enviroment, browse teams, and track cooperation. Millions of customers across the US and Europe recognize that a solution that brings people together in one unified digital location, is the thing that businesses need to keep workflows working effortlessly. The airSlate SignNow REST API allows you to integrate eSignatures into your application, internet site, CRM or cloud. Try out airSlate SignNow and enjoy faster, smoother and overall more efficient eSignature workflows!
How it works
airSlate SignNow features that users love
See exceptional results eSignature Professional Physical Therapy Consent Template made easy
Get legally-binding signatures now!
What active users are saying — e signature professional physical therapy consent template
Related searches to eSignature Professional Physical Therapy Consent Template made easy
E signature professional physical therapy consent template
good morning welcome and thank you for joining us this morning for our Medicare conditions of participation home health COP overview this webinar is to get you ready for listening to the updates webinar that will happen this afternoon with mrs. Sean Hamilton wherein you will learn the functionality of the new features that have been introduced in Access agency core my name is Jennifer Gibson I'm a registered nurse and I've been in at-home health since November 1993 and I work here at access to help ensure that you have what you need to run your business properly along with the clinicians team that works here to access so today we're going to be learning about the particular Co PS that will affect the functionality that you see and help you to understand the whys of the functionality that we have introduced in our agency core platform please note that the slides that you see here are only meant to be cue points and of course they're not the complete list of conditions of participation requirements we do have an on-demand training series that you can access for the content simply by going to access comm look for the on demand button and then you'll see the library of seven COP training videos that you can access complimentary at anytime anywhere these slides are copyrighted as well and we want to make sure that you know that you shouldn't be sharing or distributing those without the permission of myself for access but the main thing to take away here is just to know that this is not an all-inclusive slide stack that everything I say today will not be in the in the handouts that you'll receive today we're going to look at some of the new regulations some overview and insight we're going to be covering parts of the patient rights standards from the revised Co PS we're going to cover the content or some of the content of the comprehensive assessment the plan of care that you'll see as far as functionality the coordination of care some written information to the patient and then infection prevention and control we want to talk briefly about notification of patient rights you'll see on the right-hand side here a table wherein we see the timelines for which patients legal representatives patient chosen representatives and/or the patient and representative have to be notified or written and or verbal patient rights the thing that I want to highlight here is that the patient rights is we're going to talk about them in just a moment you will see highlighted in the rights patients notify being notified of different things that will translate over into the care plan and coordination of care standards as well another thing to know is as you see here on the deadlines the patient and legal representative have to be notified of the patient rights before care is initiated and that has to be done in their written form a really good thing to think about when you're talking about before care is initiated this is to happen on the initial visit and the initial visit is where you first go out and find out what the patient's care needs are now in most cases this usually happens at the same time as a start of care visit but there will be times in some policies and some agencies whereas for example the physical therapist may go out and do the initial plan of care on a therapy only patient they may do the initial assessment I should say and then the RN may go out and do the comprehensive assessment which we are familiar with as the Oasis within that five day window of the Oasis assessment closing when that happens for example the patient and legal representative have to be notified of the patient rights on the PT visits before care is initiated we also see that the patient chosen representative must be notified in written form within four business days of the initial assessment the only time that really that's not going to be the case is when the patient lets you know and it's documented in your clinical documentation that the patient does not want this chosen representative to Seve a notification of patient rights and then we see that we have some coordination of care to do here because the patient also has to have a verbal translation of the patient right by the second skilled visit and I say translation because they've got a written copy but now we have to at least verbally explain in simple English form and in the language that they choose by the second visit so you may have to do some translation as well there so just wanted to highlight that before we get into the patient rights themselves now we're not going to spend a lot of time on the patient rights this morning but I do want you to see that the patient has the right to participate in be informed about and consent or refuse care in advance of and during treatment where appropriate with respect to completion of all assessments the care to be furnished based on the comprehensive assessment the establishing and revising of the plan of care the disciplines that will furnish the care the frequency of the visits and expected outcomes of care including patient identified goals and anticipated risk and benefits why am i bringing that up well because not only are we notifying the patient of their rights but you see in that opening statement that this is an ongoing process we are to notify them of their rights to participate in and be informed about all these different things who's going to furnish the care and how often they're coming and what the patient's goals are and so on that's to happen before care happens before on that initial treatment before care is delivered whether that be teaching or whether that be hands-on care the patient has the right to participate in and give their input as to what's going to happen with their care but this also has to happen during treatment as you see in the statement here when it's appropriate and we're going to talk about that more when we talk about the care plan and coordination of care so again I just want to let you know these are tied to multiple standards and when you think about the whys why is that important because search has found that patients who are more engaged in their care tend to have better outcomes if they know the whys if they know that they have input if they understand what treatments they're getting and why and how often and who's going to provide that treatment then they are more engaged which translates into better outcomes we also see that they have the right to be informed about and consent or refuse care in advance of and during treatment where appropriate with respect to any factors that could impact treatment effectiveness and any changes in the care that is to be furnished a new standard at four eight four point five zero C five tells us that the patient has the right to receive all the services outlined in the plan of care and we're going to cover this a little more in the plan of care section in just a moment but I want you to just let that sink in especially as we're developing plans of care we have to understand that whatever we put on that plan of care the patient now has the right to receive all of those services outlined in the plan of care and if that doesn't happen then we have a possibility of getting cited for this not happening okay when we look at for 84.5 5c we get into the content of the comprehensive assessment so let's take a moment and see what is it exactly that we need to do what do we need to collect on our comprehensive assessment again this is not an all-inclusive list in order to find the complete list you will need to refer to the new Co PS section for 84.5 5c but I did want to show you some new parts in the comprehensive assessment first of all you see that the patient's current health psychosocial functional and cognitive status is required and the two key takeaways there are the psychosocial and cognitive status that is new in requirement in the new Co PS psychosocial when you think about why that's important in a comprehensive assessment the patient might very well be have recorded their functional status but we're really trying to look at how they do in the community what is their support system like because those certainly can impact the patient's engagement their treatment and it can certainly impact their outcomes so you're looking at things here such as what kind of support system do they have what level of education do they have and are they able to get food and medicine that they need do they have transportation what is the home environment like do they have smoke alarms all of those things and I bring that up because in this afternoon's session when Miss Sean Hamilton goes through the functionality you're going to see some added sections in our oasis c2 tool and our assessments and that's necessitated by these requirements you also see in the cognitive status part of this new standard that we will have to do a better job assessing the patient's cognitive status and what they're really looking for here is whether or not the patient has the cognitive status to remember the instructions that are given and to follow procedures and processes that are taught to him or her we also see that the comprehensive assessment must include the patient's strengths goals and care preferences and information that can be used to demonstrate that patients progress toward achievement of the goals identified by the patient and the measurable outcomes identified by the home health agency so again this is new regulation where and we have to document in our comprehensive assessment the patient's strengths what do they have going for them maybe they have a higher socioeconomic status or perhaps they have a really good support system in place and then what are the goals that the patient hopes to achieve you may have goals the doctor has told you but the patient may actually have unrealistic goals and so there may have to be a little bit of a refocus and helping that patient understand that maybe those goals aren't quite what we need to look for but we'll do our best to engage those and we may even have to communicate with a doctor that you know the patient's bed-bound but they want to be able to walk to the mailbox which is probably not ever going to have for him because of everything that's going on so I'm just wanting to make you aware and we'll talk with the patient and help them set some more realistic goals perhaps but all of these things have to be documented in your comprehensive assessment their goal may be something as simple as you know getting my wound better but that will have to be documented in your comprehensive assessment okay let's move to the next slide the comprehensive assessment must also contain the patient's continuing need for home care and you're going to see in the functionality of the upgraded agency core that we have added prompts to that Nashawn Hamilton as I said is going to go over that this afternoon where you see that these prompts are added in to make sure that we cover all of these required points you also see that the patient's medical nursing rehabilitative Social and discharge planning needs have to be in your comprehensive assessment as well as the review of all medications the patient is currently using in order to identify any potential adverse effects and drug reactions including ineffective drug therapy significant side effects significant drug interactions duplicate drug therapy and non-compliance with drug therapy that's why we've always had a drug interaction check ready for our users and that will continue to be the case for you as well in the comprehensive assessment we must also record the patient's primary caregiver or caregivers if any and other available supports including their willingness and ability to provide care and the availability and schedules and then we also have to record the patient's representative if they have any now we realize that this can be quite often I know I should say this can be quite often difficult again I know working in the field for many years oftentimes the more visits you make the more information you get especially when that information may not come from the referral source for that reason we are trying our best to help prompt asking the right quest Asians way before that field clinician gets in to do the start of care or the comprehensive assessment so for that reason you're going to see already in your patient intake form or the new patient form as it's called prompts that ask for things such as the patient's primary caregiver or other support persons or their patients representative and if this is a legal representative or if it's a patient's chosen representative because that's a new philosophy that's been introduced in the new co Peas as well not only can the patient have a legal representative which we know as a power of attorney or a living will or medical durable power of attorney and so on but they can also choose non legal representatives such as a church friend or a neighbor or a family member to be their representative and the patient gets to choose how that representative will function for example they may tell the admitting clinician I want my neighbor to be in charge of my medications but you don't have to worry about giving them a list of my patient rights because they're not going to be worrying about any of that but any medication teaching that happens we want to make sure we engage my neighbor over here because they're filling my med box for me and so that would all need to be documented of course and so in our patient referral or intake form we are prompting that referral intake person to go ahead and be asking from the hospital or the other referral sources if the patient has caregivers listed and what their role is the reason that we do that is because we know that hospitals and other medical settings have their own conditions of participation or conditions of payment rules and by capturing that information often they may not know that we need that so if we start training them upfront that we do in fact need that information it will make our processes much easier we also see that the comprehensive assessment has to be updated and revised as frequently as the patient's condition warrants due to a major decline in I'm sorry a major decline or improvement in the patient's health status but not less frequently than the last five days of every 60 day period beginning with the start of care or within 48 hours of the patient's return from a hospital admission or at discharge so let's let's pull this apart a little bit and look at it now we already know those last three bullets that's pretty standard that has not changed we all know that once we have a start of care for a Medicare patient the last five days in that 60-day period if we're not discharging the patient we have to do a research assessment right that's not new we also know that we have to do a resumption of care within 48 hours of that patients return from a hospital admission and that we have to do a research I'm sorry and discharge oasis pardon me what's a little bit different that's really not new but it's new again is this part where we talk about revising the comprehensive assessment as the patient's condition warrants due to a major decline or improvement in their health status now back when PPS first came about we had what was called a skip a significant change in condition SCIC and those assessments happened when the patient had such a change that it was going to affect payment and then finally through the PPS evolution that went away we didn't get our payment adjusted when a significant change happened that was adjusted at the end when we sent our final bill so most of us agencies did away with doing significant change in condition assessments or follow-up assessments what we're seeing here is that this is reintroduced at four 84.5 5d when it talks about that comprehensive assessment being revised when the patient's condition warrants so basically if you have a patient who on start of care or when the last comprehensive assessment occurred and somehow they got a better or a lot worse and it was not expected we're going to have to do a follow-up assessment or what we used to know as ass-kick it will not change your payment but what it's going to do is change your plan of care okay and we're going to get into that a little bit more in a bit so again those of you that are familiar with Skip's they're back those of you who don't know you're gonna get used to them just like we did before and I promise it won't be that bad all right let's talk about the plan of care now we've talked about the comprehensive assessment and new elements that are introduced there you're going to see revisions this afternoon and our oasis-c to documents so that these different parts are included and then the next part of that of course will be the generation of the plan of care from the oasis-c - that's revised we see here at four eight 4.60 a that the patient has to receive the home health services that are written in an individualized plan of care that identifies patient specific measurable outcomes and goals now remember we just saw this back in patient rights so the patient's aware that they have to receive all the services now when we're creating the plan of care we must also be aware that first of all this plan of care has to be individualized the days of cookie cutter blanket statement plans of care are gone matter of fact I've heard from several different consultants this week where agencies are getting cited for cookie cutter standardized not specific orders on care plans so just know that when you're out doing your assessment you're really wanting to zero in on what is it about this particular CHF patient that we need to address not just a blanket statement on instruct CHF or instruct cardiac status instruct on all meds or instruct on all disease processes they're wanting us to zero in and write an individualized plan of care and amend those orders so that they don't look exactly the same for everyone they have to have patient specific measurable outcomes and goals on the plan of care we see also that that plan of care must include the following a mental psychosocial and cognitive status again we saw that in the standards for comprehensive assessment so that's now going to flow over on the plan of care again you're gonna see functionality change an agency core because when we capture this information on the comprehensive assessment it's now going to flow over on the plan of care and I want to pause just a moment and let you know that the plan of care will not be a 485 okay the plan of care will look very similar to but it will not be the standard format that we're accustomed to and there are reasons for that first of all your 485 plan of care does not have all of these specific areas highlighted or doesn't have a place to put things like psychosocial and cognitive status so for that reason the plan of care is going to evolve into a true plan of care where these sections can be added if you look at the last bullet point here on this slide you see that a description of the patient's risk for emergency department visits and hospital readmission and all the necessary interventions to address the underlying risk factors for emergency department visits and hospital readmissions has to be on the plan of care so again we are in we are now including in our comprehensive assessment a risk assessment for er ER and hospital readmission visits and such and then that will flow over to the plan of care in a designated area so that it's easily seen and obtained and you'll see that functionality in this afternoon's webinar the individualized care plan must also include the patient and caregiver education and training to facilitate a timely discharge now again we see because this is now tied to see Opie's that the days of keeping patients on services for extended periods of time and not having any kind of discharge planning documented is going to be an issue and I kind of laughed at when I was teaching the surveyors at Joint Commission on Monday I laughed because we talked about this a little bit and what their experience has been and what I've also seen as an auditor often times when you're looking at a chart you'll see how horrible this patient is you know that we're e'en here for this reason in that and they can't function they can't walk they can't talk they can't breathe and then all of a sudden here's this discharge kind of out of nowhere it's like a miracle occurred when you're reading a chart it's really funny and we all had a good laugh about that because true truly we're not great about actually documenting that process of when we first started seeing them how bad they were and they're getting better gradually and making progress toward their goals and then we have a timely discharge but the plan of care as we see here has to actually include what education and training we're planning to do to facilitate that timely discharge so discharge planning is going to be a huge deal we also see that patient specific interventions and education has to happen measurable outcomes and goals need to be identified by the agency and the patient and that's going to flow over on the plan of care as well and again you're gonna see this over and over where it says patient specific or individualized that tells you just how important that is for CMS and for your surveyors and then of course information related to any advanced directives we are accustomed to putting DNR orders on our plans of care usually an indicator 21 on a 45 but now we have to have any advance directives on that plan of care and so again the plan of care is going to have a designated area for that now in the plan of care we see at four eight four point six zero a three that all patient care orders including verbal orders have to be recorded in the plan of care and let's take a minute think about that when you're looking at a patient's chart currently and you're trying to find out what the most current orders are normally the plan of care is generated at start of care and then it research but it's not necessarily updated in between those 60 day period time nine points and I don't know about you but as a clinician in the field especially when you had a lot of INR orders or wound care orders it could be a little bit overwhelming to try and dig through all of these supplemental verbal orders to figure out what was the most recent so we see here in our new standards that all of those patient care orders including verbal orders have to be recorded in the plan of care and for those of you that are older nurses like I am this to me is the concept almost of a card X that we used to have on the nursing floor when orders would come in we would take off than ones that had been discharged and we would add the new orders that had come in so that we always had a one-stop shop to go over and look at the most recent orders that we have or the care plan that same philosophy will sort of flow into our new functionality whereas as verbal orders are included or supplemental order to some of us call those as they are ordered during this episode of care the patient care plan is going to have a cumulative cumulative list of those orders that are active and then below that you're going to see orders that are discharged and you'll also have the ability to see a summary of that and Miss Shawn's gonna get into that much better and do a much better job than I can in this afternoon session but just know that what it was what's gonna happen from all of that is that you won't have to dig through the chart as much because you're gonna have a care plan that's current at all times of course depending upon the documentation habits of your clinician so if they document timely then this plan of care will be accurate and so the care will be much better for our patient the individualized plan of care has to be reviewed and revised by the physician who is responsible for the home health plan of care and the agency has to promptly alert the relevant physician or physicians to any changes in the patient's condition or needs that suggests the outcomes are not being achieved and/or that the plan of care should be altered now again you see standards tied to care where it's basically telling us that as clinicians if we go out in the home and we see that this patient's not progressing well that we have to alert the physicians about those changes whatever relevant physician it is so if you've got a doctor ordering insulin changes or sliding scale for blood glucose levels and you see that that's not really handling the blood glucose it's still up too high and maybe the primary care physician is the one who is ordering and overseeing the the home health plan of care you're going to notify the endocrinologist needless to say about what's going on with this patients insulin but then you're going to communicate those changes to all the physicians that are writing orders toward that plan of care so that they understand and know what's going on with the patient so we're going to get into that a little bit more in just a few slides the revised plan of care must reflect current information from the patient's updated comprehensive assessment and contain information concerning the patient's progress toward the measurable outcomes and goals identified by the agency and the patient in the plan of care so this lets us know that as we do a new comprehensive assessment that we would be generating a plan of care that reflects that current information so basically your frequencies when they change that would be updated in the plan of care if medications change that's going to be reflected in this updated plan of care and it has to match that comprehensive assessment so for that reason when you do a resumption of care or you do a follow-up significant change in condition comprehensive assessment you're going to be able to generate a new plan of care and then you'll also have that plan of care summary in our system as well and again make sure you attend this afternoon's session so you see the functionality for all of this any revision to the plan of care due to a change in patient's health status has to be communicated to the patient the representative if they have any the caregiver and all physicians issuing orders for that agency plan of care now I think for me that's the one that makes me stop and take my breath in most often because that's kind of overwhelming when you think about it productivity wise and the stress on the clinician in the field so we're gonna have to think about the best processes and policies for which to do this and that will be an agency decision like many of these are but just know whenever we have any change in the plan of care that the patient and the representatives and all the doctors who are giving orders on our plan of care have to be notified you notice it doesn't say they have to sign that they were notified so we are not talking about sending things out that will hold up billing but notifications and you'll have to be able to prove that that notification has been given right to the patient representative the care giver and all the physicians issuing orders toward that plan of care all right now we get into the actual coordination of care so we've seen the patient has rights what those rights are we see that those rights have been tied to the plan of care and the Comprehensive Assessment and now we're getting into coordination of care the agency must assure communication with all physicians involved in the plan of care now this is where the plan of care summary will come into play you will have for example if you have a significant change in condition and that generates a new plan of care clearly that plan of care will be sent to the physician who is in charge of the plan of care for that patient okay or whoever is providing care plan oversight that might be a primary care physician it might be a doctor at the hospital whomever signing your plan of care they'll get that copy to sign but in order to assure communication with all those physicians we have created an ability to do a plan of care summary and that summary can be generated and sent as an FYI document and that will help you to meet the communication with the physicians involved in the plan of care now of course just sending a fax or an email or a fax or whatever you're going to do in your policy that's not going to meet the standard itself your clinician or supervisor or whoever is doing the communication will need to document the fact that they have spoken with whomever or that they have notified them at this care plan summaries coming with some new orders that have evolved but again the Joint Commission surveyors that I've talked to you and the other surveyors and consultants say that just having a checklist or just showing that you have a fax confirmation sheet may not be enough we have to make sure that we've got the coordination of care documented and then we must integrate orders from all physicians involved in the plan of care to assure the coordination of services and interventions provided to the patient again what we're trying to achieve here is making sure that we're not delivering care in a silo we know currently that it's it's quite often a problem whereas physician a orders a drug physician B has no idea what that doctor is ordering and the patient may or may not take all of their prescription bottles with them when they go see the doctor and so the Med profile is not correct and so on so we are now taking on part of the responsibility to make sure that these physicians are communicated with and that they understand what the other doctors are doing and we're gonna see that happen in all healthcare settings in the next few years we'll see that get shored up so what I'm trying to say but this is a good first place to start so all the orders from all the physicians involved in the plan of care have to go to the central location and we have to coordinate and intervene on the patient's behalf the agency must integrate services whether those services are provided directly or under arrangement to assure that identification of the patient needs and factors that could affect patient safety and treatment effectiveness and the coordination of care is provided by all disciplines now this is where we get into the coordination of care and if you've read the CEO piece you know that they speak about doing this in a team approach and those of us that are familiar with hospice interdisciplinary teams they bring that up as an example but CMS does not mandate what your interdisciplinary team looks like but what they have mandated that all the different disciplines participate and when they talk about all disciplines they're not worried about whether or not these are full-time staff members whether these are part-time whether they're contract or whomever they all have to participate in identifying the patient's needs and making sure that the patient safety and treatment effectiveness is going on properly and that services are coordinated by all the disciplines regardless of their status so you're going to want to most likely include that in your job descriptions that's part of their job and we're going to get into that in just a minute too we see that the agency must coordinate care delivery to meet the patient's needs and involve the patient the representative the caregiver as appropriate in the coordination of care activities so as changes are happening in this patient's care plan and in their status not only are we required to make sure the physicians understand and are informed but also the patient and the patient's representative or caregivers and we're having to coordinate care within our interdisciplinary team and then when the patient and their support system and then the physicians as well and quite often we know we do this but we still do a really poor job of documenting that so you'll see in the functionality an agency core you're given a lot more prompt and you're given a lot more I should say functionality to make sure that this coordination of care can happen without as much pain as possible I should say you know I don't know what the right words are it's always going to be a pain to document all of these calls but as much as we can to help you do it easily and succinctly that's what our goal is so you're going to see that in the functionality that would present as well we must make sure is an agency that each patient and his or her caregivers receive ongoing education and training provided by the agency as appropriate regarding the care and services identified in the plan of care and that we must provide training as necessary to ensure a timely discharge again we see this tied directly to the contents of the comprehensive assessment and so we now see that it's part of coordination of care as well now one thing that we hear a lot about is written information to the patient at four eight four point six zero II there are new standards regarding written information to the patient and these standards were not in the original proposed Home Health Co P's rule as a matter of fact in the proposed rule they were talking about making sure that each patient had a copy of their plan of care when they were accepting comments at CMS several providers wrote in and said you know giving patients a copy of their plan of care is really not a good idea because there's a lot of jargon on those that they won't understand you know if we just give them a 485 for example how much of that's going to make sense to the patient and it's not going to achieve the goals that you're trying to achieve here so out of that came new regulation in the final rule at four eight four point six zero e and it's called written information to the patient so CMS is now mandating that the agency provide the patient and caregiver with a copy of written instructions that outline the patient's medication schedules and instructions and part of that includes who is going to give the medication well the medication be distributed by the patient or the caregiver or by home health agency staff you also have to have medication name dosage and frequency just like we've always done and then which medications are administered by the agency personnel as we just mentioned we also see that we have to give written information to the patient regarding any treatments that are going to be administered by agency personnel are you going to be doing a wound vac are you going to be doing labs are you going to be providing b12 injections or ultrasound with physical therapy or percussion from physical therapy so those treatments have to be given to the patient written information about which treatments they're gonna receive I should say and who's going to administer that we also see that you have to provide written information regarding any other pertinent information related to the patient's care and treatments that the agency will provide and it has to be specific to that patient's care needs so all of this has written information not everything here is going to be generated from an EMR whether that be ours or anyone else's but certainly you're going to have opportunities to give information to the patient as well some of this may be on your consent forms some of this may be on separate documentation for you as well and there's a new standard here at four eight four point six zero ie that tells you that we must give the patient the name and contact information of that home health agency clinical manager we know that this is a new role within the Co PS but this clinical manager you have to give them their business phone number and the business address and you can give their email address as well if you like but and then you have to instruct the patient on when they should contact this clinical manager for what reasons and all of that has to be given to the patient as far as when the interpretive guidelines say that by the time or soon thereafter when that comprehensive assessment is completed this information should be given to the patient so you know you have a five day window to complete your comprehensive assessment and while we have no final interpretive guidance out I would suggest that this is done within five days or less or when the comprehensive assessment is completed whichever comes first all right we see from the draft interpretive guidelines once that comprehensive assessment is completed here's where I just pulled the guidance that I talked about the documents mentioned must be provided to the patient clear written communication between the agency and the patient representative ensures that patients and families understand what to expect and that's really the goal of why we're doing all this communication in the written form to the agency I'm sorry from the agency to the patient is so that they understand what to expect the written information has to include the most current written visit schedule that needs to be provided to the patient and that it's consistent with the most current plan of care I want to make a point here that informed consent when you're talking about your patients rights and remembering the patient rights how the patient has the right to be informed of changes realize CMS is talking here that informed consent does not just happen on admission in other words you consent form on admission where they initial and sign everything that is not the only time that CMS is looking for documentation and proof that informed consent happens when you have changes to the plan of care you're gonna have to document that you have explained that to the patient and that they gave consent if there's a new treatment there needs to be documentation that that clinician explain to the patient what the treatment is why it's been ordered that they said yes I consent to that and keep moving on now that may be according to your policy you may have a form you want to fill out it may be something as simple as documenting in your narrative but you're going to have to show evidence that the visit schedule matches for example the most recent comprehensive assessment or the written schedule if there's changes in that schedule due to a verbal order that the patient has given written information that is current to that new visit schedule and so on it also says here that written medication information has to be in plain language and should avoid using abbreviations now with Joint Commission standards we haven't been using abbreviations and mid profiles for a long time but for other agencies who may be licensed and certified only this is going to be new for you so you're gonna have to write out bureaus imide one tablet daily by mouth you can't use abbreviations when you're giving this medication information all right let's keep moving here we still have quite a bit to go over when it talks about the draft interpretive guidelines as I said you have to give the name and phone number of that clinical manager their email address and you should explain when that clinical manager should be notified now I want to take a few minutes here toward the end to talk about infection prevention and control and then the duties of the skilled professionals because oftentimes and I understand having been a clinician in the field for many many years clinicians can get overwhelmed and/or you may have clinicians who have a make a visit mentality and I think that these are exceptions to the general rule that most of us clinicians who are in home health are there because we love what we do and we care about our patients and we want to do a really good job and most of the time when we're given the tools to do so we will do so I want to make sure that you administrators and upper management persons who are listening understand that you're going to need to train your staff and help them understand the whys just as you're learning the whys today so that they can do a good job for you so infection prevention and control is one of those areas where CMS has told us we have to maintain and document an infection control program which has as its goal the prevention and control of infections and communicable diseases there are three different standards here you've got prevention and of course we have to follow accepted standards of practice including standard precautions to prevent infections and communicable diseases you're going to want to make sure that every clinical note documents the fact that the staff member is making the right what am I trying to say here that they are actually practicing standard precautions to prevent infections we of course have in the functionality the ability to easily document that on all of our nodes we also see that there's a control standard we have to maintain a coordinated agency-wide program for the surveillance identification prevention control and investigation of infectious and communicable diseases and that has to be integral in your H home health agencies QAPI program again agency korres always integrated and the clinicians notes the ability to document infection prevention and control standards when they identify an infection there's a button they can click on and go ahead and fill that out immediately while it's fresh on their mind rather than putting that off for a later date and then forgetting it right and then of course you have reports in our system so that you can run those infection reports and get the information you need to investigate and use this in your QAPI program for the infection control program you also see there's new standards that we have to include a method for identifying infectious and communicable disease problems and a plan for appropriate actions that are expected to result in improvement in the disease prevention that may not be as new but certainly what you see under the education standard here at four eight four point seven zero C this is new the agency has to provide infection education to staff that's not new but to patients and caregivers as well and when we see this in the co P regulation and interpretive guidance they're not just talking about you know a blanket statement here they're talking about getting in the Nitty Gritty here and really teaching patients and caregivers on appropriate patient specific infection control measures such as the use the transport storage and cleaning methods of patient care equipment and some of us you know we're trained well and we do that anyway but I have certainly had experiences where I go in after another nurse or I'm reviewing a record and you see a patient with a glucometer and there's literally just blood smeared everywhere or the patient is throwing away their lancets directly in the trash or they're throwing their inr strips in the trash so they're not really showing that they understand infection prevention and control and so we have to provide education and document that it's included in our documentation rather the appropriate use transport storage and cleaning methods of patient care equipment like glucometers INR machines oxygen tanks nebulizers you know are we teaching the patient when they've had an upper respiratory infection to change out their oxygen tubing or how often to clean their nebulizer machines and mouthpieces and all of that we're getting really specific in the CEO piece here as to that being a standard now this for the staff this means that you have to do jobs specific infection prevention education and training this will need to be documented in your HR files at the your staff members whether they are full-time part-time or contract staff that they have had training on infection prevention education and training then is job specific and then you also have to have processes that ensure all healthcare personnel understand and are competent to adhere to this education so you're gonna have to have some competency check offs as well lastly I want to just give a brief highlight of the skilled professional services and what's expected from those persons of course our skilled professionals are our skilled nursing our ends and lVN's or LPNs our physical therapists our PTAs our SLP speech-language pathologists our occupational therapists and medical social workers the skilled professionals and it says whether that's directly hired or under arrangement must participate in coordination of care I can't stress that enough it doesn't matter if it's part-time full-time per visit contract whomever they must participate in coordination of care again if I were an agency director today I would be writing this into my skilled professionals job descriptions and any therapy or other contract agreements that we have and of course for qualifications to perform skill services in the home health setting each of these professionals have a set of qualifications and that spelled out at four eight four point one one five we're not going to go through that today but that's where you see the regulation as far as what the qualifications are to be a skilled professional and home we also see at 4:8 4.75 B 1 B 2 and B 3 that the skilled professionals assume responsibility for ongoing interdisciplinary assessment of the patient the development and evaluation of the plan of care and partnership with the patient the representative and the caregivers and for providing services that are ordered by a physician as indicated in the plan of care now why am i bringing that up because quite often unfortunately we get our hands on sometimes some skilled professionals who just want to make a visit they have that mentality of going in I'm gonna go in I'm gonna give the insulin and I'm gonna go into my next patient and no one ever hears from them they don't give report or they don't want to develop a plan of care I've seen agencies who allow their clinical staff to go and do a start of care and turn in the Oasis and someone at the office actually does the plan of care and we see here at 480 4.75 the skilled professional is assuming responsibility for developing and evaluating that plan of care with the patient and the representative and the caregivers so what we're seeing here is again lining up what the job descriptions are how the clinician in the field is to function and how this process is happening from the comprehensive assessment on up and that they have to provide services that are ordered by a physician as indicated in the plan of care so again we all know we've seen these bad habits where and I will tell you from a personal experience going behind one of the nurses that has done this to me before for example you have a wound care patient you go out and you have your most recent physician order you start performing the wound care and the patient says oh my gosh that's not what the last nurse has been doing what are you doing and I look at my order and I double-check the chart and this is the order I have so we're gonna do what the order that I have is and then I called that other nurse and she says something like oh well that wound care went really working so I've changed it to something else and we're gonna try it and then if that works then I'll write the order okay that's not how this is supposed to go needless to say and now we have a standard that will tie things like that to a standard level deficiency so we have to make sure that all services are ordered by the physician and that they're in the plan of care skilled professionals also assume responsibility for patient caregiver and family counseling that's not news to most most of us who provide services in the home we do that routinely anyway but it is now tied to a standard we're also assuming responsibility for patient and caregiver education preparing clinical notes and communicating with all the physicians involved in the plan of care and other health care practitioners as appropriate related to the plan of care and again when they talk about skilled professionals they don't care what their employment status is they want to make sure that they are aware that they are responsible for all of these things in a home health setting they are also required to participate in the agency's QAPI program and participate in agency sponsored in-service training so the days of your staff being able to say up I can't come to that training I got a patient to see they're required here under the CEO PS to participate in that agency sponsored in-service training so you may have to get creative as to how many times you have that in-service or what different times you're having them to make sure all your staff can attend lastly we see that the skilled professional services have to happen under supervision of course nursing services have to happen under the supervision of an RN the rehab services have to happen under supervision of the OT or the PT and the medical Social Service services have to happen under supervision of the social worker so again just note that the functionality and agency core will continue to give you the ability to do your suit visits as indicated by these standards that functionality will still be in the system the contents of the clinical record at four eight four point one one zero a we see that the record has to include the patient's comprehensive assessment including all the assessments from the most recent admission clinical notes plans of care physician orders all interventions and responses to the interventions all medication administration all treatments and all services and then the record must also include the goals in the plan of care and the patient's progress in achieving them and we hear this all the time your clinical record really should paint the picture of the patient status when you first started seeing them and how they progressed to the status that they are at the time that you're seeing the patient now and that now includes their goals and the patient's progress toward the goals here's a little bit that I wanted to tell you about some new functionality here the record must also include the contact information for the patient that contact information for the patient's representative if they have any and the contact information for the patient's primary caregiver and again we've included this in our patient intake or new patient form because we know that it has to be in our record and it can be difficult to get this information and by trying to prompt even at referral getting this information the better off we're gonna be because by the time we get the record completed hopefully we will be able to include all of this information or at least document the multiple attempts that we've tried to get the information from the referral source and/or the patient as well now I will say and you'll see this in Shawn's functionality webinar this afternoon these prompts are there but they are not mandated so if you get this information at referral it will flow over to your Oasis but if you don't it will not hold you up okay you can still put your referral in the record also has to include the contact information for the primary care practitioner or other health care professional he's going to provide care and services to the patient after the home health agency discharges that patient and what it's talking about here is if the patient identifies an attending physician who's going to resume care after the agency episode or after the discharge that contact info should included in the medical record and you're going to have the ability to document and designate who the primary care physician is and that doesn't matter if they're the responsible agency physician or not as far as signing orders they still want this attending physician to be documented so that after discharge you can send a summary to this physician letting them know what has happened and that again is for continuity of care we want to make sure that we're not working in a silo that after our work is done in the home that the physician he's going to be taking care of that patient afterwards understands what we've done to maintain this patient from being in the hospital again and from going to the ER so that they can resume that care as well and continue that we also see that the record has to include a completed discharge summary and that that discharge summary has to be sent to that primary care practitioner or other healthcare professional who's responsible after discharge from the agency and we have to send that DC summary to the PCP within 5 business days of the patient's discharge the discharge summary typically includes the following items you have your admission and discharge dates the physician responsible for the home health plan of care the reason for admission to home health the types of services provided in the frequency of services any lab data any medications the patients on at the time of discharge the patient's discharge condition the outcomes and meeting the goals and the plan of care and then the patient and Families post discharge instructions and again Shawn is going to tell you about some functionality for that discharge summary this afternoon again make sure that that discharge summary is sent to the PCP within 5 business days from the date of the order from the responsible physician for discharge now pay attention in that draft interpretive guidance they're not talking about 5 days from when the discharge summary was completed they're talking about 5 days from when you got the order to discharge that patient so that's a timeline you're gonna have to pay attention to as well you must also have if it's applicable a completed transfer summary that needs to be sent to the transferring facility within two business days if it's a planned transfer and they're going to continue to get health care in this facility you have to send that out within two business days again that just reiterates how we must keep our clinical documentation up to date and of course an EMR is going to help you do that much easier than being on paper right paper and all of the things that go along with that including new regulation that your documentation has to be legible plus the quick turnarounds that we see here within notification of transfer and discharge helps us to understand that really paper is gone by the wayside and that EMRs are the way to go now if you don't know that this patient ended up transferring and we certainly have that happen sometimes patient goes to the hospital and they're actually discharged before we knew that they were ever transferred in the first place when that happens we still have to send a transfer summary within two business days of becoming aware of an unplanned transfer if they're still at the facility if not you don't have to do the transfer summary and again it tells us in the draft interpretive guidelines here that the contents of the transfer summary typically contains the same components as a discharge summary authentication we see at four eight four point one one zero B and we're getting ready to wrap up so just be patient I'm almost done we see here and as I was just mentioning with the paper charting that all entries in the clinical records have to be legible it has to be clear it has to be complete and it has to be appropriately authenticated dated and timed authentication must include a signature and a title or the occupation or a secured computer entry by a unique identifier of a primary author who has received reviewed and approved of that entry what does that mean in our system and agency core each user has a unique identifier which is your email address and the password that you create current functionality in our system in the QA Center is going to be affected by this standard and Shawn's gonna talk about the functionality of that I don't know if that'll be in today's webinar or it will come later but you're going to see in the QA Center if a clinician has turned in an oasis for example and another supervising clinician goes behind her and changes something in that document you're now going to have that reflected in the signatures you'll see the original clinician signature and followed that following that will be that person who made the amendments signature as well so that's going to meet this requirement where they have a unique identifier of the primary author who has reviewed and approved the entry and so you're gonna see that functionality change a little bit as well lastly again just to help you understand that EMRs having that up to date having it ready to go is the way you're going to have to function in the new environment we see at four eight four one one zero e the patient's clinical record must be available to the patient on request this can be done hardcopy or it can be electronic but it has to be given to that patient free of charge here's the caveat when the patient requests their record you have to get it to them by the next home visit or within four business days whichever comes first here's where that continuity of care and coordination and communication comes in because if you've got two visits scheduled the same day the patient mentions to the aide who's at the patient's home that morning that they want a copy of their clinical record you have to be able to deliver that before the next clinician goes out in the afternoon so you're gonna have to know what their visit schedules look like you're gonna have to be able to coordinate that care and of course you're gonna have to be able to print out that EMR and give them their record as soon as possible so again there's lots and lots and lots to think about with the Co PS we certainly have not covered everything in today's webinar but we have covered those things that will help you understand the functionality of agency cool when you listen in to the subsequent webinar this afternoon certainly any time you have questions or comments you can contact us here and access give me just a moment we're not gonna do those questions now if you have questions and comments right now if you will put those in the portal in the go-to meeting and we will make sure that we review those questions and comments as they come in I'll see if we have any just now we probably since we're out of time will not be able to answer all of these questions now but just be aware we do have subsequent sessions coming up we also will have these recorded and on-demand are there handouts we're gonna send out handouts to the emails that you used to register today you will get the handouts from this webinar later on and within the next couple days and then again feel free to reach out to us we have all kinds of stuff on demand we have the COP training series on demand we will have subsequent emails and then questions about functionality I won't be answering those right now but you will see all these functionality questions answered in the webinar this afternoon so we will continue to go through the questions as we go and make sure we get back to you I'm gonna scroll through just a few of these real quick let me expand the question box on my view so I can see them a lot of these have to do with functionality so those of you that have questions about how the system is gonna function whether or not we're gonna have certain assessments or whether or not we have certain things in the medication profile all of that really you're going to need to tune in to this afternoon's webinar to get those answered you can also send questions of course to my email address you see it here at Jay Gibson and access comm I'm sure miss Shawn will also be and Shawn is our product manager clinical product manager she's gonna have a lot more answers for you as far as functionality than I do but certainly you can always send these questions to us here at access also know that we have a robust Help Center that we're going to be using and we are already using it now we will continue to update that in the future as well with all of these questions that have come in we want to make sure that you have what you need in order to be compliant and that is our sorry that's our goal the webinar that this afternoon will be going on at 1:00 p.m. you should have received in the same link that you got for this particular I'm sorry it's not one it's three o'clock Thank You Steven three o'clock this afternoon Central Time the link for that webinar should be in the same email that you received earlier as well as your login page when you go in to access comm and you go to your login page you should see the Medicare Co P webinar popup on the right hand side where it shows how you can register there as well those two webinars but the one that I'm conducting now and the functionality overview webinar will occur again tomorrow and Monday we've yet to put that up but it is coming very soon and so you'll have multiple opportunities to attend both live as well as you'll be able to attend these recorded webinars series very soon as well yes they will go into on-demand can a do n be the clinical manager of the agency yes they can several questions again we will make sure that all of these questions are answered in our Help Center and again you can always reach out to me anytime you need to I've got an email address a phone number here as well and continue to let us know how we can help you in the future again my name is Jennifer Gibson I do appreciate very much you taking the time out of your very busy schedules to be with us today and because I know very few people get the things that they need I just want to remind you that no matter what your job is and the home health agency we do appreciate the fact that you're there doing that job because the patients that you serve get the care that they need because work that you do and that should never go unacknowledged and thank so have a wonderful day we will see you again soon and thank you again for being in our webinar today
Show moreFrequently asked questions
How do I eSign a document before sending it?
What counts as an electronic signature?
How can I get someone to sign my PDF?
Get more for eSignature Professional Physical Therapy Consent Template made easy
- Print signature service Advertising Agency Agreement Template
- Prove email signature Honeymoon Reservation Record
- Endorse eSign Thank You For Interview Letter
- Authorize digital sign Event Management Proposal
- Anneal signatory 1099-MISC Form
- Justify eSignature Accounts Receivable Financing Agreement
- Try digisign Operational Plan
- Add Governance Agreement electronically sign
- Send NGO Project Proposal Template countersignature
- Fax Evaluation Form digital signature
- Seal Lien Release Form signed
- Password Loan Agreement digi-sign
- Pass Auto Repair Contract Template esign
- Renew Late Rent Notice initial
- Test BMI Chart signature
- Require Form W-8BEN email signature
- Send onlooker esigning
- Accredit seer byline
- Compel receiver electronically signed
- Void Job Quote Template template electronically signing
- Adopt deed template mark
- Vouch Plane Ticket template signed
- Establish Graphic Design Quote template autograph
- Clear Distribution Agreement Template template digital sign
- Complete Soccer Camp Registration template initial
- Force Speaker Agreement Template – BaseCRM Version template signed electronically
- Permit PC Voucher template electronically sign
- Customize Motion Graphics Design Contract Template template countersignature