eSign Blood Donation Consent Made Easy
Get the powerful eSignature capabilities you need from the solution you trust
Select the pro service created for pros
Configure eSignature API quickly
Work better together
Esign blood donation consent, within a few minutes
Cut the closing time
Keep sensitive data safe
See airSlate SignNow eSignatures in action
airSlate SignNow solutions for better efficiency
Our user reviews speak for themselves






Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.

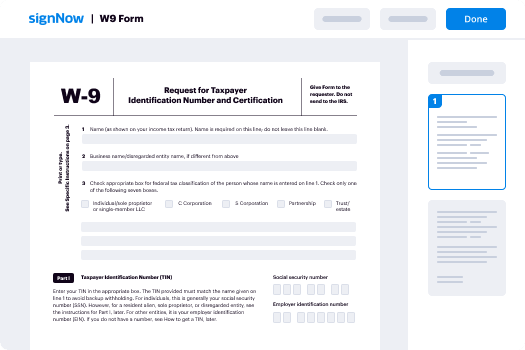
Your step-by-step guide — esign blood donation consent
Leveraging airSlate SignNow’s electronic signature any business can enhance signature workflows and eSign in real-time, delivering a better experience to customers and employees. Use esign Blood Donation Consent in a few easy steps. Our mobile-first apps make operating on the move possible, even while offline! Sign contracts from any place worldwide and complete trades in less time.
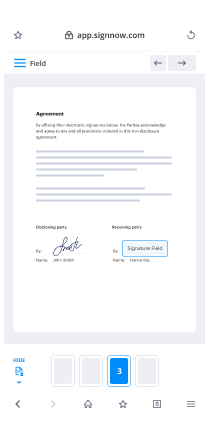
Take a step-by-step guideline for using esign Blood Donation Consent:
- Log on to your airSlate SignNow account.
- Find your document in your folders or upload a new one.
- Access the template and edit content using the Tools list.
- Place fillable fields, type text and sign it.
- List numerous signees using their emails and set up the signing order.
- Choose which recipients will get an completed copy.
- Use Advanced Options to restrict access to the template and set up an expiration date.
- Tap Save and Close when completed.
In addition, there are more innovative functions available for esign Blood Donation Consent. List users to your collaborative digital workplace, browse teams, and monitor collaboration. Millions of consumers across the US and Europe concur that a solution that brings everything together in a single cohesive work area, is what companies need to keep workflows functioning smoothly. The airSlate SignNow REST API allows you to embed eSignatures into your app, website, CRM or cloud storage. Try out airSlate SignNow and get faster, easier and overall more effective eSignature workflows!
How it works
airSlate SignNow features that users love
See exceptional results esign Blood Donation Consent made easy
Get legally-binding signatures now!
What active users are saying — esign blood donation consent
Related searches to esign Blood Donation Consent made easy
Esign blood donation consent
so thank you very much for inviting me and to the darwin college to give um a talk tonight my name is dr claire roddy um and i work at the ucl car t cell program and we look after a whole host of different patients with cancer giving them experimental therapies and using the immune system to target their cancer welcome to the 36 darwin college lecture series and the first to be presented entirely online this series began in 1986 as an evolution of the annual darwin lecture and since then over 270 talks have been given every year the college selects a topic usually a single word and identifies a series of eminent speakers from across disciplines to share their insights and thinking on that topic with us we try and ensure a balance between the arts and humanities and the physical biological social and technological sciences believing that an interdisciplinary approach to any subject is both the most stimulating and the most relevant to our audience normally the lady mitchell hall lecture theatre in cambridge is brimming with an excited audience live waiting in anticipation of the first of our eight authoritative entertaining and informative lectures spanning disciplines on topics of great fascination and importance to us all our guest speaker would have spent time with our students earlier in the day and would be joining the darwin college community for a formal dinner in college afterwards such socializing will return in future and we very much look forward to that in the meantime if there is an upside to this traumatic pandemic we're all experiencing it is that the technology for online presentation and our ability to use it has dramatically improved so we're able to continue to share these great talks with you recording speakers in this way is new for us so please bear with us if the quality is not what you're used to we're deeply grateful to our speakers this year for making the time to record their talks and we welcome an opportunity to share them with you online at this time in doing so we hope we will be reaching a global audience as well as our usual largely cambridge based community of cambridge college lecture devotees the lectures will as always remain online so please do share the details of our youtube channel with anyone you think might enjoy the lecture tonight the theme for the 2021 series is blood and what could be more important and fascinating a subject when we're in the middle of a global pandemic blood performs many important functions it supplies oxygen and nutrients to tissues it removes waste and it transports messages around our body by carrying hormones it regulates our body temperature and has a key immunological function to enable us to fight off diseases in this lecture series we will hear about blood as a specialized form of tissue its role in our health and that of other animals we will also explore its importance in literature history mythology and art we're in for an extraordinary and wonderful series of talks our first speaker tonight is dr claire roddy from the university college london she is currently on the front line of tackling the coronavirus pandemic working at the university college london hospitals we're very grateful to you claire for making time to deliver this lecture despite your clinical commitments clara is a consultant hematologist and an associate professor at the cancer institute in the faculty of medical sciences at ucl and she specializes in blood cancer and personalized medicine she's currently playing a leading role in developing the first in human trials for car t-cell therapy a treatment that's described as the beginning of the end of cancer it's my great pleasure to welcome and introduce dr claire rody whose lecture is entitled battle blood and so my title um of my lecture tonight is battle blood and uh it's uh talk about fighting leukemia i'm a hematologist by training and this is my daily job so um an inspiring quote by hillary bellock um reflects the experience of um hematologists at the beginning of the last century when they were faced with the prospect of treating leukemia and particularly leukemia and children and of course they celebrated hillary bellock and and people didn't really understand leukemia um it's certainly not in 1845 when john bennett um who's a scottish physician who managed all range of uh medical problems but he described an unusual case where he saw 28 year old slate layer and who presented to him with gross fatigue and a large tumor on the left side of his abdomen this patient developed fevers bleeding and abdominal pain and was rapidly developing other new tumors in his armpits is growing on his neck and you can see this illustrated here in an anatomic depiction of the lymph node areas in the human body now the treatment at the time in 1845 consisted of leeches and purging but sadly there was no response to treatment and a few weeks later the patient died but john went on to do an autopsy and when he looked at the blood he found it was full of white blood cells and the principal constituent of pus so bennett presumed that there was an infection but he couldn't find the source and so he concluded simply that it was a separation of pus with no clear cause so um virco described a 50 year old lady um with white cells that were explosively overgrown and who also had a large spleen but with no signs of infection so he concluded in the absence of infection it must be intrinsically the white blood cells that are abnormal and he just simply described this as isis blood or white blood in german um or leukemia and which is derived from the word lucos which is the the greek word for white and he and virgo went on to sort of further define um aberrant growth um in cells as hypertrophy which is an increase in in cell size or hyperplasia which is an increase in cell number and so he then went on to describe this leukemia or this excess of white blood cells as a pathological and abnormal hyperplasia where the cells had an unexplained drive towards growth and so this is really very much a novel inexplicable distorted cell growth that seems to come from the white blood cells themselves and so what is b cell acute lymphoblastic leukemia well essentially it's just an uncontrolled expansion of immature immune cells or blasts as we call them and these cells are unable to perform the function um of mature lymphocytes and the worst problem associated with these glasses that they completely destroy the bone marrow space and as a consequence and the normal architecture of the bone marrow is completely disrupted and the normal blood production um is abated as a result you can see this image of the um the bone marrow on the right hand side of the screen and that's a beautiful and healthy bone marrow image and the symptoms of leukemia um are the common symptoms that we see in the clinic include anemia where the low cells which help us stop bleeding when we cut ourselves an infection of course from catastrophically low white blood cells which are the cells that protect us from infection and you get a myriad other different symptoms relating to the high proliferation of these leukemia cells such as fever weight loss and bony pains and when we examine our patients we often see a large spleen lymph nodes increased in size in all the areas that we demonstrated in the previous slide and pallor and bruising and the view in 1950 wasn't particularly different and to the view in the 1840s and they're describing acute lymphoblastic leukemia as its palliation is a daily task it's cure a fervent hope and that was william castle but the man who really sort of changed the the whole landscape for acute lymphoblastic leukemia is this man this is sydney farber and he was working over in boston as a pathologist at the children's hospital and um during his time in that role he wrote a book on the classification of childhood tumors which is called the post-mortem examination now during that time he develops a scientific interest in what he describes as the hopeless condition of childhood leukemia now you have to understand at this time there was no cancer research strategy there was very limited treatment options which included radiation and surgery which of course for a circulating blood-borne type of cancer you can imagine how futile those options really are so he reasoned that in order to be able to understand cancer better given the research paradigms of the time and to begin any kind of scientific discovery that you need to be able to measure the cancer in question and that's where the beauty of leukemia comes in because it can be so easily measured in the blood and if you can measure cancer it means you can very easily investigate the impact or the potency of your intervention in living patients so if white cells die or they grow in the blood it's a measure of success or failure of the therapy now faber looked for inspiration across the board including to um normal healthy patient hematology and he he looked at the work of someone called lucy wills he was an english english physician who in 1928 she traveled to bombay and she was studying profound anemia that was observed in factory workers there and these factory workers were often malnourished and this anemia seemed to specifically affect um mothers and their children more so than other members of the population and by some surprising um turn of events she discovered that this anemia was cured with marmite and when they looked into this in more detail oleic acid and which is a vitamin that's found in fruit and vegetables and of course it stands to reason because when cells divide across the body and we need to make copies of our dna in order for that process to happen and folic acid is critical to this and when you think about the blood system and the fact that as healthy people we make more than 300 billion blood cells every day you can imagine how important it is and the folic acid levels are retained within normal range and of course deficiency leads to significant problems so sydney farber got the thinking about this and he wondered all of his leukemia patients with her acute lymphoblastic leukemia had no functioning normal blood cells so could he address this by supplying extra folic acid or a synthetic version of folic acid to overcome that problem he reasoned that the blasts or the leukemia cells were preferentially taking all the folic acid away from the normal blood cells so he basically instituted an early clinical trial looking at a synthetic version of folic acid in his pediatric patients but contrary to his hypothesis unfortunately the folic acid supplementation seemed to accelerate the leukemia growth so he then went back to the drawing board and he figured that if adding folic acid was causing a worsening leukemia picture then what about antagonizing or blocking folic acid to see whether or not it would have the opposite effect and he had a close collaborator and friend um a biochemist who was also a trained physician um called a yellow pergada subaru who is otherwise known as yellow and he made it his work in his laboratory to try to synthesize synthetic versions of compounds and and chemicals that exist within normal cells and he at the time was trying to create a folic acid and a synthetic version thereof but in the process of doing that had inadvertently created a range of folic acid antagonists including one called amonopterin so what farber did was he took this amenopterion and he designed a trial for childhood mball and lo and behold the first patient of robert sandler who is a twin um who had a horrible presentation with acute lymphoblastic leukemia with fractures from bony disease six signs of leukemia and he very quickly achieved a dramatic remission following amenoctrine which was really unprecedented in the field of b acute lymphoblastic leukemia for which at that stage there really were no treatment options at all now this resulted in this boy going back to school playing with his friends but unfortunately the remission was quite short-lived and he did relapse after several months now this was reflected i did start the process of exploring lots of different types of chemotherapy agents for this condition but of course chemotherapy alone in all is not always the answer and so this is the next important move in the field of acute lymphoblastic leukemia and that's the the development of allogeneic bone marrow transplantation and the picture here is in fact one of sydney farber's proteges a chap called um donald thomas who won a nobel prize in 1990 for his trouble um creating the paradigms for bone marrow transplantation and what he showed was that bone marrow could be transplanted from one individual to another and following an obliterative dose of chemotherapy or radiotherapy to get rid of the patient's immune system and he showed that those new cells could make a home in the patient and it was in 1956 where the first successful allergenic bone marrow transplant was reported and again this was in a boy who had leukemia and he received obliterative radiotherapy followed by a healthy bone marrow from an identical twin for acute lymphoblastic leukemia so taking this paradigm a step forward lots of other investigators look to do bone marrow transplantation also and dr george matthey gave um an allogeneic bone marrow transplant to six engineers who unfortunately following a nuclear reactor incident had developed a severe and debilitating bone marrow aplasia now he gave them bone marrow derived from an unrelated donor but unfortunately all of the patients suffered a debilitating wasting condition which we commonly now know as graft versus host disease and because these this was an unrelated donor unlike the previous boy who'd had his donation from an identical twin and unfortunately the unrelated nature of this donor meant that there was an immunological reaction and rejection of the patient cells as a consequence so the next really important discovery in this area um was by dr jean ducey who again won the nobel prize in 1980 for this discovery because he identified the reason for the graft versus his disease phenomenon he observed that there was if there was a mismatch in the protein signature on the surface of the blood compartment and these hla or human leukocyte antigens and then what that meant was that there could be immunological rejection not only of the incoming cells but also damage and graph versus whose disease of the patient so clearly hla compatibility is key to the success of this type of treatment for all conditions but equally for acute lymphoblastic leukemia but of course it acute lymphoblastic leukemia is difficult to treat and by the 1980s doctors were routinely using allogeneic transplantation for chemotherapy and radiotherapy refractory diseases so that's a sort of a brief history of where we're at with our therapies for acute lymphoblastic leukemia now but what's the current state of play um in therapeutics at the moment i mean there has been an incredible progress in this area for patients today standard therapy is generally chemotherapy based patients will have induction therapy that's where they come in newly diagnosed and will have multiple drugs as an inpatient in hospital over one to two months and during that time it's almost perceived that the treatment is worse than the disease because we render the patients and completely aplastic they have no functioning immune system and we have to effectively be the immune system for these patients by enclosing them in in protected and isolated rooms the next phase is consolidation again it's a lengthy process eight weeks of chemotherapy in order to consolidate the remission that is to its belt and braces approach to make sure that the leukemia doesn't come back but we know that if we don't treat patients beyond eight weeks and we leave them to go about their normal business that in a large proportion of patients the leukemia will come back there is a niche of leukemia stem cells that can repopulate the marrow at any given time and we know that by putting patients on a program of maintenance chemotherapy over a course of two years and sometimes three years in in boys and high-risk patients and that that can help to prevent relapse and we have to integrate into that specific therapies to try to stop the leukemia from going to what are described as sanctuary sites which is areas where our immunological responses are not capable of rejecting um tumors and leukemia and that's the brain and the testes and of course in some cases we do give what is now an optimized version of allogeneic bone marrow transplantation to those with high risk or relapse disease so one might ask is the battle with acute lymphoblastic leukemia finally over have we finally got there well not quite in terms of outcomes although in pediatrics as in in children and young adults um it's still quite common it's a communist childhood cancer but for those patients who do relapse which is about 20 the overall survival is about 40 to 50 percent and so that's not great these children have their whole life ahead of them and that's not seen as a good metric for success in adults it's even more challenging and it's reasonably prevalent as a condition and the prognosis is still poor and long-term remission rates are really limited to 30 to 40 percent of patients with our best care now as the 50 percent of patients who do relapse the outcomes are pretty dismal with a five-year overall survival of seven percent so it leads us to the whole question new paradigms about how we can treat leukemia that doesn't involve promote marrow transplantation and that doesn't involve chemotherapy because by the time the patients have got to this point they are usually refractory to those options so it leads us to think a little bit about the adaptive immune system and whether or not this in some way might be redirected to to see leukemia and to be able to target leukemia and so we know that in our adaptive immune system we've got b cells and we've got t cells and b cells um they secrete uh small proteins into the blood um called antibodies which label foreign particles and organisms for destruction and that includes bacteria and they can also neutralize viruses and they work in tandem with the blood dust bins if you want for a better word that's macrocyte macrophages and monocytes which can come along and gobble up and all of these either bacteria or or viruses t cells have a slightly different rule they selectively recognize cells that have been invaded by a pathogen usually viruses and they can even sometimes recognize cells with mutations and they kill them by binding to the cell and then punching little holes in the surface of the cell and then secreting toxic substances into those infected cells and of course researchers have long sought to harness this amazing it's a cytotoxic or pillar potential of these t cells and to see how that can be redirected towards cancer cells but t cells have been explored in this context before this is not new um cellular immunotherapy for virus-associated cancers and including virus-associated lymphoma which is a cancer again of the immune system and the lymph glands and this has been um trialled um over the last 20 years where blood is taken from the patient with the mars associated lymphoma the t cells are extracted from that blood they're grown up in the laboratory and then they're administered back to the patient and this is a little cartoon of what happens in the laboratory you essentially take the and the blood cells and from the patient or sometimes even from a third-party donor an unrelated donor and what you do is you expose them to these target cells that are expressing proteins associated with the virus in question and that's driving the lymphoma and with some growth hormone support this il2 or interleukin-2 you get enough cell numbers that you can introduce this to a patient and this is the pharynx it's the back of the throat of a patient who has an epstein-barr virus driven lymphoma you can see the white plaque um at the back of the pharynx here and all of the excoriation and redness but after the cells you can see that that's completely cleared so there is evidence that t cells can recognize tumors and kill them even if the context here is that it's a virus driven tumor so the next area that people have been interested in t cells is looking in solid tumors and the concept of immuno lymphocytes that have infiltrated tumor tissue directly or the so-called tumor infiltrating lymphocytes that's an area of a lot of um scientific endeavor you basically take the patient's tumor you excise it and then you can um separate out the t cells from within that tumor and grew them up using rapid expansion protocols in the laboratory to the sorts of numbers that may be associated with clinical effect if you infuse them into the patient and probably the best model in which to test tumor infiltrating lymphocytes is metastatic melanoma so the skin cancer because it's a very immunogenic tumor i.e it expresses antigens or or proteins on its surface that are recognized or can be recognized by the immune system as foreign and this image at the bottom of the screen shows um on the left it's a cat scan of a patient with metastatic melanoma this is a deposit in the liver and you can see on the right hand side of the screen this is an image of a patient with a large subcutaneous or under the skin deposit of melanoma and with infusion of tumor infiltrating lymphocyte therapy you can see the marked improvement in the focus in the liver and the significant improvement in the the area underneath the skin and so this tumor infiltrating lymphocyte therapy certainly has its part to play and it is potent for certain um types of cancer um but it only works for a small proportion of patients in a small proportion of of tumors and so it leads us to question how we can improve upon these success rates using other types of technology basically most cancers can't be recognized by the immune system because cancers arise from us and our immune systems are developed um to tolerate self and to tolerate our own tissues so there has to be something very unique and specific about the cancer cell that arises within us that allows the immune system to see it cancer-specific b cells are very difficult to grow in the laboratory and the as i said the immune system is designed to tolerate itself so this approach using um unmanipulated cells probably has limited scope and certainly in hematology so how to get over this well this is where the science fiction comes in can we create a synthetic immune system and we believe that the answers lie in gene engineering and synthetic biology to all of these problems and effectively what you do is you take what's already in existence that's b cells and t cells and you use those as the building blocks the b cells we know make proteins or antibodies which can target and bind bacteria with high specificity so they can find external targets and then we've got our t cells which are evolved to kill virus infected cells and they're incredibly cytotoxic and potent and they bind targets derived from inside the cells in their usual room but if we combine these two capabilities we could harness the t cell killing capability with the exquisitely specific and targeting of cell surface proteins through the b cell component and using molecular cloning we can insert b cell genes into t cells using a safety modified virus and often of hiv type and it's a bit like a trojan horse and being used to get past your t-cell immune restrictions and so synthetic biology and in its purest form here with chimeric antigen receptors and a chimera of course being from greek mythology and a mixture of a lion's head a goat audi and a serpent's tail and this is really the inspiration for for for generating the name for for this particular type of receptor because of course there's paradoxical expression of antibody which shouldn't really be there on the t cell so it's a chimeric receptor it's a mixture and the genetic transfer creates um something that you know we haven't seen before in in medicine or hematology and that's effectively supercharged killer t cells this is a living drug and a single infusion of these cells can divide and multiply into millions of cells inside the patient and the cells can stay alive and on the job for many years and we've got patients who are on our clinical trials here are two and beyond years out from their therapy and we can still see those car t cells in their bloodstream and they really i don't know if you describe this as punching above their weight but they're really very potent cells because one car t cell can actually kill a thousand tumor cells so that's preclinical you know in vitro data but it's a very impressive um capability and this is what a chimeric antigen receptor looks like it's a very very simple structure and it's very easy to design it basically comprises three portions you've got the derivative from the antibody that i described already and this is this extracellular portion here which you can really target any cell surface um protein and or even some non-processed molecules glycolipids for instance we've got a couple of cars targeting those and then you have to push this antigen binding domain off of the cell surface because there's a lot of noise although it's not depicted in this cartoon but you need to you really need to get that above the noise on the surface of the cell to allow it optimal um opportunity to bind its its target on the tumor cell and this is just called a hinge or a spacer region and this is a really important bit here you have to come on a journey with me this is inside the cell and this is the signaling endoderm and that sends a signal into that t cell telling it to kill and telling it to proliferate and the beauty of this system is as i say it's very easy to design it's not mhc restricted so there's no complications around matching and effectively you can just take a patient t cells and do a very simple gene transfer and you will end up with a car t cell product for them and this is i work very closely um with martin pulley who is a gene engineer um who and this is very much how he sees rt cells he sees them as little mini robots traveling around inside the patient with their little sort of circuit board or they're rewiring that allows them to do something completely normal and a completely novel function and to target cancer and this is what the process looks like and again you know it it possibly seems like science fiction maybe 10 years ago but now is very commonplace we just take blood from the patient or leukopheresis harvest and you take the t cells out you use a safety modified viral vector to introduce a new gene into those t cells and then you grow them up in the laboratory you expand them to the numbers that you think are important for clinical effect and then you inject them back into the patient and hope that they traffic to the tumor and a lot of what we've done so far is targeting a specific protein um on b cells and we've talked a lot about leukemia already and the protein that we're targeting is called cd19 and cd19 is a really really good target for car t cells and why is that well firstly it's expressed at really high levels on the cell surface and it's good to have lots of expression of antigen it gives your car plenty of target to bind and to try to ensure a good clinical response the other beauty of cd19 is the fact that it's very faithfully expressed on only the b cell lineage so it's not expressed on stem cells it's not expressed on the surface of the lung so you can be assured that your patient isn't going to get some nasty off-target toxicity that you haven't anticipated which has certainly been a problem with some other targets and particularly in the solid tumor field but i'm not going to say that the road to get to this point we're at currently was easy there was a lot of suffering and what is commonly described as the dark phase of car t cell therapy which is probably about 10 years ago now and people were using and again leukemia patients who were being recruited into clinical studies for car t cell therapy with the early cars and what these plots show you is it's the engraftment of the car t cell in the blood of the patient so forgive the grafts but effectively just what they're showing you is the car in the blood and they're measuring it by the presence of the the gene in the blood and you can just see here that it's such an underwhelming car expansion the the the the the fact that the pinnacle of car expansion is you know 10 copies per microgram of genomic dna that's almost nothing it doesn't really persist you can see that the levels fall away to zero virtually after a few days so these were really disappointing times of course none of these patients got good in graftman none of them got good clinical effects none of them got any toxicity as you would expect and it really um prompted the field to go and do quite a lot of soul searching and a lot of further pre-clinical work to try and understand what had gone wrong and i think the conclusions that people came to were that there are three really important facets and for the success of car t cell therapy that are illustrated in this venn diagram and we'll talk first about co-stimulation now again we have to learn the lessons of biology we have to learn the lessons of physiology if we're going to employ you know use these these um modules successfully and in a gene engineered or synthetic biology way and so if i'm asking a t-cell in its normal way to look for a virus-infected target cell well usually i have to give it two signals so first of all the t-cell receptor on the t cell we'll expect to see some derivative of the virus expressed on the surface of an antigen presenting cell that will be signal one but if signal one occurs in isolation then this t cell becomes anergic it essentially doesn't proliferate and it doesn't expand and it sort of switches off what's needed for a t cell to become active and this is a sort of a safety mechanism if you like is signal one plus signal two and signal two comes in many different flavors but when one will refer to here is cd28 this is a cool stimulatory receptor that is expressed on a t cell and when the co-stimulatory receptor cd28 ccd 80 or cd86 in tandem with the t-cell receptor signal that is what precipitates the expansion and the activation of that t cell but this had been ignored in the early car work where essentially the cars had been designed simply with the t cell receptor signal a first generation endodomine at this time nobody had considered the potential importance of co-stimulation and so thus it's no surprise that we see these car t cells or these first generation car t cells lacking efficacy and lacking the ability to grow and proliferate so a bit of molecular biology a bit of engineering resulted in these fusion domains where and the the tcr signal or the cd3 was fused onto a co-stimulatory domain such as cd 28 41 bb or 40 and again that's the second generation car t cells that we're commonly using now people have gone one step further third generation fourth generation fusing as many acoustic military and domains getting car t cells to concurrently secrete and synthesize and cytokines chemokines so there's lots of engineering developments that have occurred um in the last few years but um this is probably one of the most elegant experiments in the field and it was a lady called barbara savaldo when she published this back in 2011 she had a patient with an acute lymphoblastic leukemia and she really wanted to answer the question about why first generation versus second generation car t cells what the differences might be and whether second generation truly did afford significant improvement in outcome so she took that patient's t cells in the laboratory she split them into two halves one half she introduced the first generation car and the second half she introduced the second generation car and she infused them at the same time into the patient and monitored using different marker genes as to the expansion of the relative populations and what you can see here in the the graph below is the first generation car in the red has got a very low level expansion and seems to drop a way off to zero after four weeks you can see a significant difference with the the second generation car you can see a much better expansion and there seems to be persistence at four weeks it doesn't fall to zero and you get this increase again after dose two so this one piece of evidence was really very significant for the field and it prompted all the major groups and at this time it was really mainly in the us and to look at um the second generation cars okay so um in the previous um slide we've looked at the impact of co-stimulation and on car t cell design and potential expansion in in patients we then move on to a next um critical facet to car t cell um success and that is the use of lymph depletion and here we look at a historic precedent set by the till field and that's a tumor infiltrating lymphocyte therapy field and where they this this group of scientists really wanted to understand how they could improve outcomes for patients receiving this therapy and what they observed was that if one prepared the patient in advance by depleting and their endogenous immune compartment using either irradiation or chemotherapy that one could potentially enhance the expansion of the introduced cells through the tumor infiltrating lymphocytes and you can see that with this and kaplan-meier analysis here which is effectively showing us survival of patients who received till therapy for metastatic melanoma and you can see on the bottom here the lowest line on this graph where patients didn't receive any type of depletion and you can see that the proportion surviving is very small by um 36 and 42 months but you can see when you use non-myeloablative and conditioning and in this category we're looking at um chemotherapy you can see that that's led to an improvement in the proportion surviving and over the longer term and you can see similar improvements of the use of um higher doses of of total body irradiation and intermediate dose and higher dose so there seems to be a an impact um of depleting the endogenous immune compartments prior to the introduction of these new cells that precipitates an advantage in that patient and so this piece of work that's been done um over by steve rosenberg and mark bergen mark dudley's group um at the nih has really set the way um for the rest of the adoptive cell therapy field including for car t cell therapy where lymphodepleation is now used routinely prior to the introduction of the car t cells and how this works again there's lots of different sort of questions over this but it's thought that it contributes mainly by eradicating suppressor immune cells and that are present in the lymphoid structures and that will slow down the expansion of the car t cells when they're introduced it's also thought that it up regulates danger signals and endothelial markers that might help the car t cells and traffic and to sites of disease and there are other factors about um activating dendritic cells and so on and again talking about co-stimulation allowing the expression of co-stimulatory markers to help your t cells to really get all those activation signals that they need so that's the role of lympho depletion or preparing the way for the infusion of the cars then we need to think about how the car t cells are made in the laboratory and i think at the early phase people were just so delighted to be able to do something that appeared so complex that perhaps and you know that in itself was the uh that that in itself was a result however we've come to understand over the last 10 years that really the manufacture method and how one handles this cell seems to be really important to the clinical outcome so this is a little schema of what happens to the patient effectively you take their blood and when you get those cells into the laboratory there's lots of different ways that you can activate those t cells because without activating them um they tend to die so and you can use antibody coated beads and where you're fooling the t cell into thinking it's seen an antigen presenting cell once those cells are nice and activated you can then introduce your new gene via usually your viral vector or via genome editing again that's more recent development in our field and then after you've done that what you do is you grow the cells up in the lab until they all express or at least a good proportion of them express car t on your surface and then you freeze them down and you get your patient in to prepare them for the upcoming infusion and as i say we routinely use lympho depleting chemotherapy for the reasons that i outlined in the previous slides and then we keep our patients in generally for approximately 28 days to monitor for the potential toxicities from this treatment so if you want to make a product for a patient it's incredibly important that that's done in an absolutely sterile environment and in an absolutely sterile way and so we've spent a lot of our time um over recent years setting up um gmp or good manufacturing practice car capability and and that's down at ucl and you can see we've got an individual in the clean rooms here and fully dressed in the protective suit and the over sleeves and handling the products we use these um either an isolator or a cabinet to handle the cells and the materials and everything is done um in this type of environment with sort of careful error handling and careful temperature control etcetera um so there's the classic dynabead car manufacturer process that's and i've alluded to this already how we make the cells in the lab i just have to emphasize really from this slide that it doesn't look like very much but in actual fact it's um incredibly labor intensive and incredibly complicated and it costs a lot of money and the equipment um is very costly to maintain and the monitoring and training that's required for everybody is really it's really enormous so we basically so we're talking about the manufacturing is very complex and um and actually the health of the cells and the quality of the cells um is is really sort of paramount to the efficacy of the product in the patient and this um cartoon is supposed to demonstrate what happens to a normal t cell when it goes through the process of meeting an antigen or a target and it goes through this phase from naivety right the way through to terminal differentiation and terminal differentiation you can imagine when a cell gets to that stage that that has limited proliferation capability it has um limited functionality and if you were to generate a car t cell product that was comprised comprised essentially all terminally differentiated cells then that really wouldn't be able to deliver much of a clinical response so a lot of our efforts in the laboratory have really gone towards trying to move away from that terminally differentiated product and trying to enrich products for more early effectors and more central memory phenotypes because we know that those phenotypes will persist in our patients and they will expand better in our patients and we know that that leads to better clinical responses so we have lots of different ways of doing that we can modulate the cytokines that we give these cells to grow in the lab we can shorten the manufacture process so there's lots of different things that we can do and to enable that and myriad factors really do influence car cardi different results that arise from having a different car t cell binder so if you use a different antibody fragment that may well lead to a completely different clinical outcome and as we've shown in some of our own academic studies compared with some of the commercial cars the type of vector that you use is it important you use a retrovirus versus a lentivirus in terms of persistence and in terms of that product and you know growing inside your patient there definitely is a school of thought that lentivirus and 401 bb endodomine seem to be associated with longer persistence and then of course you've got the production process that we've alluded to and then the clinical factors what's happened to that patient you know what kind of a hot t-cell harvest was it what conditioning did they have how much prior therapy have they had so all of these factors make it quite difficult to compare because no two patients are the same and the other big factor that we need to consider here is that this is it's not necessarily an easy therapy per se although one might argue that one infusion versus two or three years of treatment and with with chemotherapy that holds a lot of advantages however we have to bear in mind that car t cells because of their nature they distribute themselves around the whole body and they can cause problems with all of the organ systems so that is one significant problem that we face and probably the biggest thing that used to frighten me when i first um was starting in this program at ucl was something called cytokine release syndrome and basically this is the result of the car t cells being infused finding their target binding and secreting lots of inflammatory factors into the blood in order to try and kill the target but in doing that it activates the rest of the endogenous immune system and it can lead to a very severe um hyperpyrexia or high temperature that can often be associated with drop in blood pressure kidney failure respiratory failure and so on so these patients can get really sick and with multi-organ failure and so we monitor very closely for this syndrome now luckily for us we do have access to drugs that can interrupt this process um carl june who's really widely regarded as the sort of the father of car t cell therapy he started the program at university of pennsylvania in the us and he treated a patient back in the early days um of car t and that patient became very unwell um in the process of the treatment and he instigated the use of a drug um called tosalisimab fossilism that blocks interleukin-6 and he observed in his particular patient that interleukin-6 levels were very high in the aftermath of the car therapy now this was completely off license and tosylisimab was licensed only recently for um juvenile arthritis but it certainly wasn't licensed for experimental therapies such as carte but the science and the translation and that finding of the interleukin-6 drove him to apply to the institutional review boards and ethics boards at the university of pennsylvania and to get the permission of um the patient's um parents to use this drug off license and sure enough the impact was nothing short of miraculous essentially the fever the patient deaf revenge the fever came down and the patient then came off all of the um the organ support structures so it's really important that we sort of keep an open mind about the pathophysiology of all these sorts of um side effects and you know that we sort of think outside the box a little bit about what we can potentially do to to manage these these these side effects and in that case carl june and his decision certainly saved that patient's life there's a more difficult to manage syndrome neurotoxicity irritation of the brain which we um commonly see in our patients as well it's felt to be related to the overwhelming inflammation that comes from the car t cell expansion and it's not thought necessarily to be related to car t cells going up into the brain tissue per se it doesn't seem to be related to the presence of disease so for instance if you have leukemia in the brain it doesn't seem to be the risk of neurotoxicity doesn't seem to be worsened by that um but when it it does arise it can be quite challenging to manage um and the things that we warn the patient for in the clinic include word-finding difficulties there seems to be a real predilection for language centers and so we often find that patients will sort of repeat the same word multiple times without necessarily realizing it or in some cases have become completely aphasic and unable to speak at all we've had some patients who've had full-blown seizures and we've even had the occasional patient who's had a coma as a result of the car t cells and this is all very scary when you're having to sort of consent people in the clinic to undergo this treatment and luckily we have got experience now we have a feel for what we can do to try to help this syndrome and usually it's about suppressing the immune system drugs like corticosteroids for instance can be very helpful and there are other more experimental treatments like anakinra which allows us to block certain immunological pathways including interleukin-1 and that's proven to be helpful certainly in preventing severe neurotoxicity and then of course this is very predictable and we mentioned it at the beginning if you're going to target cd19 well cd19 is a protein that is expressed on b cells and a leukemia cell is just a b cell gun rogue and so uh the the cd19 that you see in your leukemia cell you will equally see it on your healthy b cells so the ones that aren't affected by the leukemia so of course you recover from your leukemia your car t cell is a living drug it's inside your system it will continue to pick off healthy b cells as long as those car t cells are still alive in your system and as a consequence of not having any normal b cells well what happens you can't really make your own antibodies particularly effectively of course that renders you much more susceptible to things like infection and infection of the chest and so on so there are certain situations where in our patients we will start immunoglobulin infusions to try to protect them from that side effect and this is another problem that we see because of the overwhelming inflammation inside the bone marrow space with this highly concentrated population of leukemia cells sometimes the car t cells seem to have an impact um on the even the healthy cells that are there and we sometimes see these prolonged low blood counts in our patients and you know patients do require transfusions support with their white blood cells hormones to support the production of white blood cells and and platelets to try to get them through that phase but it usually results within a few months after treatment and this is emily whitehead so this is the patient i was mentioning earlier that carl june had treated at the university of pennsylvania and she really is an exemplar case because she's the the perfect patient for this therapy she's chemotherapy and radiotherapy refractory leukemia the disease came back three times and in the pediatric setting that's incredibly poor prognostic sign she had advanced incurable leukemia and in april 2012 um she received just the one car t cell infusion and by day three she was admitted to the intensive care unit with renal lung and cardiac failure and a very high fever with no obvious infectious cause and when they screen the blood for the cytokines they find the elevation of the interleukin-6 that i mentioned a thousand times the normal levels and this was what prompted carl june to use tosylisimab and as a consequence of that she recovered and we also now have access to tussle-ism lab because it's now approved for use for all of our patients and these are just some images of um this patient uh again just sort of the the journey pre-car t um which was really very painful for her and her family and then they've done i mean this is the sort of american um standard they get their patients back every year for a photograph opportunity just to sort of celebrate the fact that against the odds and particularly for this girl who was super prognosis that she's done so well and she's very much she's she's really the poster girl and for car t cell therapy for this indication but it wasn't just her you know the the effect was seen um across a huge um population of of pediatric patients um and this graph depicts the um the event free survival or the outcomes for for patients 59 patients but they went on to recruit way more patients than that um and these are the sort of patients who don't respond to any kind of treatment and all of them are expected to go on to palliative pathways and they all received a single dose of cartese and 93 percent of them achieved complete responses at month one and what's really um special and what stands out about this treatment is the fact that in 50 of those patients the responses were maintained at 12 months you can see that by this flattening of the curve here so we're not getting any further relapses at this point so it's just a question of whether or not if you get patients to the sort of 9 or 12 month mark whether or not that really represents uh potentially long-term remission or even cure the word that hematologists rarely utter and this is another um patient history which just gives us a feel for how severe these sorts of syndromes can be and it's a 34 year old lady who had um a type of cd19 expressing lymphoma and she had the chemotherapy that we've discussed and she had the one dose of car t cells literally within 24 hours she had a fever of 39.5 which of course we knew that physiologic temperature is 37.4 so she's significantly feverish and this was just called a grade 1 cytokine release syndrome and she started antibiotics and was watched very closely but then she dropped her blood pressure and she needed bonuses of intravenous fluid and we gave her the drug that carl june trialled in emily whitehead the tussle is a nab to counteract this this syndrome but unfortunately then she deteriorated further her oxygen levels dropped she ended up with a great um ongoing grade two and cytokine release syndrome needed oxygen got another further dose of tosalisimab but what was surprising was then two days later um she gets this inability to write and she becomes quite disorientated and she was still had a high fever so she got more tolerable and she didn't have steroids at that time but within the next four days and this is the sort of rapidity of the growth of these cells and also the rapidity of the recovery she was able to be discharged home and this slide just shows us what we routinely do with our patients and the words we routinely get them to write a sentence and we ask them it's a neural cognitive assessment that we do every day twice a day um and you can see that the writing at day four of the treatment seems to be preserved but by day five this is very typically what we see the patient can't write anything logical or sensible really struggling with a tremor um but thankfully by day six it seems to have resolved so this is the writing seems to be a very sensitive indicator of neurotoxicity and we find it very useful in clinical management on the wards and for this particular patient this is a pet ct scan where we inject labeled glucose into the patient and the labeled glucose goes to the area and where the lymphoma or the leukemia is active and here you can see that it's active in the abdomen and in the pelvis and then you can see by day 30 that that's completely gone and this is just an indication of what we look for when we're we're looking for the car t cells in the blood we do check by um flu cytometry but we also look at the level of dna in the blood um and you can see that in this case this is a a patient who was actually treated in the u.s but you can see that the transgene or the car and gene that's detected within the blood has expanded to very high levels within this first 40 days and seems to persist up to 180 days and probably beyond and this flu cytometry plot here on the right hand side shows us this is cd19 so this is our target these are the bad cells of the leukemia cells and this is before treatment and then we can see after treatment that that population has completely disappeared through the potency of this treatment it's just like um the sydney farber measuring things in the blood is so rewarding and when you're a hematologist and you're working with experimental therapies it's it's very tangible and very rewarding to see these results and so quickly and i think you know we're all aware of the the publicity that this therapy has generated across the world and the media have really um embraced this whole story and thankfully so have the fda and uh nice and the ema and the fda did license the first car he sell products and for use in the us in 2017 and then we got the license to go ahead with on the national health service um at the end of 2018. now the problem is that patients do relapse we know that there are some patients in fact who don't even respond at all and that's about seven percent of patients and we think that that's probably related to the fact that the product just isn't very good and that's usually related to heavily pre-treated patients or patients who've got lots and lots of bone marrow disease and it's very difficult to get the number of t cells that you need to make a good product we sometimes see this cd19 positive relapse so the disease comes back and it's still expressing cd19 and what that usually tells us is that the car t cell has failed in some way um it means that it's failed to persist in the peripheral blood now the i think the working hypothesis with that it's sometimes the car t cells can become exhausted and sometimes that's driven by the tumor itself the tumor can have um intrinsic mechanisms that mean that it is resistant to death pathway induction so when you try to kill the cartesian when the car t cell tries to kill the tumor cell um it shows some resistance to the mechanisms by which the car t cell can do that and that can induce exhaustion in the car which then becomes unable to perform its normal function the other thing that can happen is remember the car the the protein structure on the surface of the cell it's derived from an antibody and of course most antibodies are neuron derived you know they're usually achieved through vaccination of rodents and the the immune system when it recovers from the initial limbo depletion sometimes it can see those differences and it detects the car as foreign and you can get an immunologically mediated car rejection so that would explain why we see ccd 19 positive relapses of course there's lots of research efforts going on to try and figure out you know how we can overcome those sorts of problems so for instance one can fully humanize the car and again you do that through sort of protein engineering in the laboratory um in order to reduce the risk of the patient's immune system seeing it as foreign and you can also do lots of clever things in the manufacturing process and using different um substrates and reagents to to make the car t cells more was more able to proliferate um in the face of adversity and in the in the face of factors that might otherwise induce t cell exhaustion now our biggest problem really probably in car t cell therapy is the cd19 negative relapses and of all of the relapses that we see this comprises two thirds of them and that's effectively where the leukemia is smarter than the therapy and through either mutation or splice variation and epigenetic phenomenon the the the leukemia cell loses the target the car continues to circulate it continues to kill normal b cells but the leukemia sadly can repopulate the entire bone marrow and this is an example of a patient who had just that so a patient who had disease in their marrow this was a patient with a lymphoblastic lymphoma and they had disease in their groin at the beginning here in the little red box you've seen that that seems to have been eradicated at month one however there's overt relapse um at month two and when we looked at the original biopsies of the site of disease what you can see here is a part of this lymph node and the brown stain that's so clear is the expression of cd19 on that tumor um but the next slide what you can see is when we went in after these patients relapsed that they completely lost expression of cd19 there's no ground stain to be seen at all and so of course if you lose the target for a targeted immunotherapy the disease can come back and so the working hypothesis here is that if you target more than one antigen on the surface of the leukemia cell or the lymphoma cell can you overcome this antigen escape mechanism so of course we and others are looking at combining cd19 and cd22 targeting cd22 is another protein that's expressed on the surface of both malignant and normal b cells and just to see whether or not we can overcome this the as really is the achilles heel um of of of cd19 car t cell therapy so i suppose from the point of view of ourselves at the ucl programme i mean really car t cells are a major part of how we treat leukemia and lymphoma they're not without toxicity i hope that's come through um but a significant proportion of the patients that we treat can achieve long-term responses following a single dose and to that and really this therapy is unprecedented and we're really excited by the rapid pace of development and you know we're moving not just further into the cd19 space but also into other hematologic malignancies and solid cancers and it's really the beginning of the journey i mean most car t cell groups are working to try and understand how we can make our therapies better uh more effective and greater numbers of patients including addressing antigen loss and i think you know on the right hand side you can see the concerns that we have about the therapy it's expensive um you know and does the cost justify is it justified with the current outcomes i think as we get more efficient at delivering the treatment as we get more efficient at the manufacturing and as we get better at managing the side effects as we get more sophisticated with our cars you know we've got low and toxicity cars that we generate at ucl that have a lower sort of cytokine secretion profile and lesser crs i think that these we're going to be able to address these cost issues downstream [Music] and of course to look at this overall the car story really is one full of setbacks and if you go back to 2008 2009 and the first generation cars we could have lost the whole technology at that point um but it's just thanks to the kind of resilience and perseverance of the researchers who went back to the drawing board went back to the lab to to move things forward we have them to thank for this huge paradigm shifting treatment that we're able to give our patients today and the future is really exciting in this field i mean it's just a great privilege to be part of it all and you know we're at the moment we're looking at lots of different areas of research we're looking really towards third-party products we quite like the idea that we didn't have to go to the patient every time to make car t that one could just reach a product off the shelf we've got lots of innovative ways and to try to do this we're really interested and i specifically am very interested in in car t cell application to solid tumors i think it's really the elephant in the room i think we've had a real paucity of good targets for solid tumors but i i think that we're getting more sophisticated and with bioinformatics and the kind of the detailed analysis that's coming off of the out of the solar tumor space i i think that we will be able to address that um and the optimized car manufacturing i've talked about is clearly so important to the growth potential of the product and if we can make all of our products you know much more aligned and streamlined we may be able to get more predictable clinical responses improve our outcomes for patients and of course at the bottom here we're talking about it's not just a car t cell field lots of exciting work going on in the tumor infiltrating lymphocyte field as well as um alternative gene engineered t cell approaches such as tcrt cells so with that i'd like to thank you very much for listening um to this talk and i'd be very happy to take any questions thank you so much claire for a really fascinating and stimulating lecture it was a wonderfully clear history of leukemia and how it can be treated culminating in some incredibly exciting developments of new therapies that you're pioneering we're deeply grateful to you as i said at the beginning for taking the time out of your front line work on the wards to share with us both your research and some reasons for us all to be hopeful in the years to come i would like to say a very special thank you to the organizers of this year's darwin college lecture series professor martin jones the george pitt rivers professor of archaeological science and emeritus fellow at darwin college and dr josefina foskulu the patrick sissons evelyn trust research fellow at darwin for so brilliantly putting together this lecture series and they're holding their nerve during the difficult times we've had in knowing whether we are going to be able to deliver these lectures in person in the lecture theatre or having to do them online i'd also like to thank our education and research committee rit team and our registrar janet gibson for supporting the whole lecture series process next week our speaker will be dr sarah reed she's a lecturer at loughborough university who is both a specialist in early modern culture literature and medicine with a specific focus on women's reproductive health and she's a novelist as well please join us for what i'm sure will be a very different but no less fascinating perspective on blood thank you and good night you
Show moreFrequently asked questions
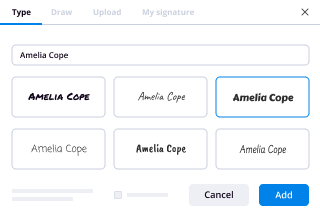
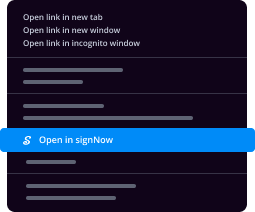
How do I eSign a document before sending it?
How do I add an electronic signature to my PDF using a Signature Field in airSlate SignNow?
What's my electronic signature?
Get more for esign Blood Donation Consent made easy
- ESignature on msft
- Prove email signature Release of Information
- Endorse eSign Event Satisfaction Survey
- Authorize digital sign Video Production Quote
- Anneal signatory Prenuptial Agreement Template
- Justify eSignature Resignation Agreement
- Try digisign Gala Reservation Confirmation Letter
- Add Interest Transfer Agreement mark
- Send Travel Agency Proposal Template signed
- Fax Summer Camp Certificate digi-sign
- Seal Sponsorship Letter digital sign
- Password Real Estate Purchase Agreement initial
- Pass Food Service Contract Template signature
- Renew Lease/Rental Agreement countersignature
- Test Alumni Chapter Annual Report digital signature
- Require Form W-4 electronically signed
- Send proof signature service
- Accredit cosigner signature block
- Compel guest esign
- Void Rental Receipt Template template eSignature
- Adopt paper template autograph
- Vouch Itinerary Planner template digital sign
- Establish Interior Design Quote template signed electronically
- Clear Tripartite Agreement Template template electronically sign
- Complete Food Allergy Chart template countersignature
- Force Mobile Application Development Agreement Template template electronically signing
- Permit Basketball League Registration Event template mark
- Customize Computer Service Contract Template template signed