Signature Block Doctor's Medication Order Template for Campers Made Easy
Upgrade your document workflow with airSlate SignNow
Flexible eSignature workflows
Fast visibility into document status
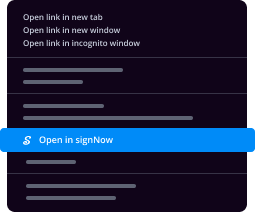
Easy and fast integration set up
Signature block doctors medication order template for campers on any device
Advanced Audit Trail
Rigorous safety requirements
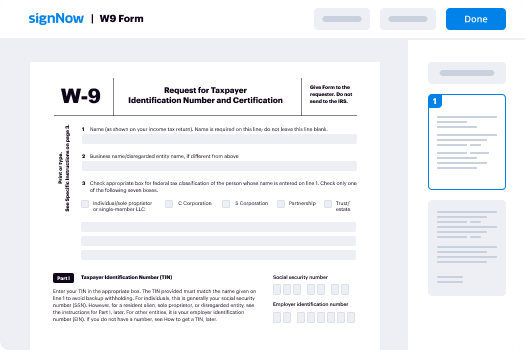
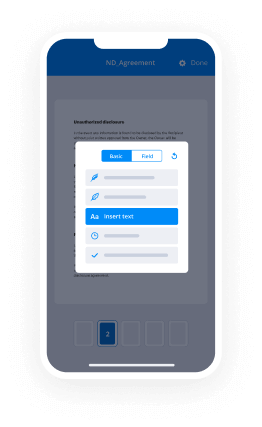
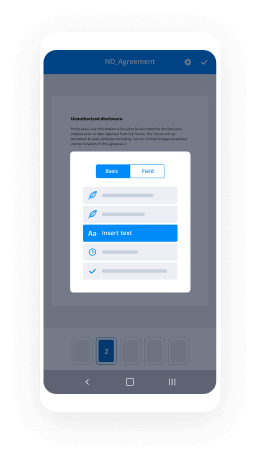
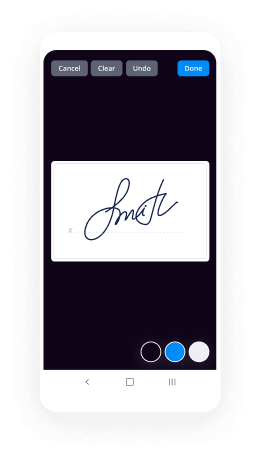
See airSlate SignNow eSignatures in action
airSlate SignNow solutions for better efficiency
Our user reviews speak for themselves






Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.

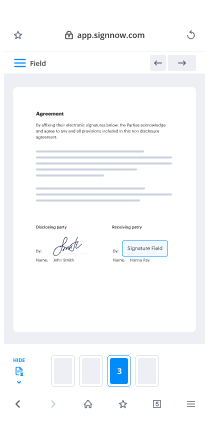
Your step-by-step guide — signature block doctors medication order template for campers
Adopting airSlate SignNow’s electronic signature any company can increase signature workflows and sign online in real-time, giving an improved experience to clients and workers. Use signature block Doctor's Medication Order Template for Campers in a few easy steps. Our handheld mobile apps make working on the move achievable, even while off-line! eSign contracts from any place worldwide and close up trades faster.
Keep to the step-by-step instruction for using signature block Doctor's Medication Order Template for Campers:
- Log on to your airSlate SignNow profile.
- Find your record in your folders or upload a new one.
- Open the template adjust using the Tools menu.
- Drop fillable areas, add text and sign it.
- Add several signees by emails and set up the signing order.
- Specify which recipients can get an signed copy.
- Use Advanced Options to limit access to the record and set an expiration date.
- Click Save and Close when finished.
Moreover, there are more extended tools available for signature block Doctor's Medication Order Template for Campers. Add users to your common workspace, view teams, and track teamwork. Numerous users all over the US and Europe concur that a system that brings people together in one unified enviroment, is exactly what businesses need to keep workflows performing easily. The airSlate SignNow REST API allows you to embed eSignatures into your application, website, CRM or cloud. Try out airSlate SignNow and get faster, smoother and overall more productive eSignature workflows!
How it works
airSlate SignNow features that users love
See exceptional results signature block Doctor's Medication Order Template for Campers made easy
Get legally-binding signatures now!
What active users are saying — signature block doctors medication order template for campers
Related searches to signature block Doctor's Medication Order Template for Campers made easy
Signature block doctors medication order template for campers
the pleasure to be here and I'm very excited to share with you some information and data from the culmination of some of the work I've been working on for last ten years or so in the space of airway microbiome and asthma and we're starting to do some work in COPD as well which I obviously won't talk about today but my goal is to give you a flavor of where the field of microbiome research and lung disease with the focus on asthma has come over the last several years in the context of asthma here the objectives I do want to spend a little bit of time reviewing evidence linking the microbiome in early life took childhood asthma I realized we're all adult physicians here but in the context of allergic airway diseases some very brief overview I think is good context to have because we draw a lot of inference from the wealth of literature and the studies I've been done over the last two decades and the child at pediatric asthma realm and then I'll focus on the middle of I talk about just telling you a bit about recent evidence linking the airway microphone dads with phenotype and adults and that's work that's more directly that I've been more directly involved with the last couple of years and then finally I would like to offer some chaplet some discussion about challenges and new directions to understand how microbiota influenced lung disease phenotype and some of the considerable challenges that still remain in doing this in the clinical context so as many of you're familiar that was a very common highly prevalent disease affects about 300 million people worldwide and this is now an old slide drawing from data that the whu-oh published back in 2004 and that was we capitulated in a review article by science in 2011 and I think the flavor I want to impart to you is just the idea that asthma is really much more of a first world disease it's much more proven westernized countries industrialized nations and even in large scale begin Mia logic studies over the years they have looked at populations where the demographics are changing quite a bit such as parts of China in Africa which isn't really captured here in the map but as you have increasing levels of urbanization and people migrating from Mooreville rural communities into the urban environment those growing urban centers see an increased rise in allergic as well as autoimmune diseases such as asthma but I also has not all the same and I think that's a flavor of the phenotype definition that has a less you know 20 years or so and become more and more refined with many large network studies funded by the NIH trying to dissect at least doing some sort of clustering type analyses to define different asthma phenotypes and that's what's captured up here in this top tier of this review article I do with my mentor a couple years ago when we were at UCSF and just to summarize well we sort of view microbiota and the science of microbiome fits into studying lung disease at least in the context of asthma we know a lot about genomic genomics of asthma susceptibility genes there's been intense interest in that but really the function of a lot of those genes and how they impact disease phenotype remain a little elusive we certainly know a lot about the immune system the adaptive immune components that play a role in shaping asthma and I'll discuss that a little bit more a lot of data on epithelial mucous cell biology and in between we feel like that microbiota at least saw the mucosal lining services such as the respiratory tract have really been overlooked in the clinical context and that's where we focused our energy over the last couple of years I think in the clinical context certainly in the pediatric literature this is well establishes environmental exposures in the very early life window that impact gut immune development through the microbiome can have a profound impact in Savelle susceptibility to allergic diseases later in life but in adults we recognize that these comorbidities listed here they're just one of several also important cool abilities and as we know that significant sinus disease in the nasal cavity certainly can increase morbidity and symptom burden with asthma obese related asthma is also an entity that's not well understood we think of obesity as much of our systemic inflammatory disease and we think that has role in lung disease but certainly the mechanisms are not really well understood just yet and a gastro esophageal reflux disease has also been associated with increased asthma symptoms although large trials looking at the role of PPI interventions and asthma control really haven't been negative but clinically we recognize it as contributing to coughing and symptoms with shortness of breath so I think the latest definition from the Global Initiative for asthma in 2014 really tried to highlight this variability in disease we have been heterogeneity there and I won't read it but that's highlighted in these yellow terms that were including the definition of asthma came out in 2014 okay so I wanted to spend just a minute or two just a setting definition straight because I think the microbiome term has been so popular over the last ten years and in literature when we review papers I often see microbiome being referred to and yet we're really talking about microbiota and so what's the difference this definition is borrowed from a lovely sort of prospective piece I was published by Marchetti and Ravel jock rubella is a microbiome scientist at the University of Maryland I think he's actually editor-in-chief of this new journal that's really rapidly risen an impact factor but he he and and and his co-author here proposed the definition that microbiome really is not just about the organisms and that's what the definition has been used loosely in the literature and those of us who work in the space are trying to be more attended into terminology but it really encompasses the biome the entire habitat the ecosystem that includes the micro organisms what their genes potentially can do and do do and the surrounding environmental conditioner micro environment conditions that's really the microbiome and in the context of discussing the human microbiome as a member as a part of its National Academy community I was part of it last about a year and a half we decided to make it clear that microbiome could be used in conjunction with specific sites when we talk about the gut microbiome the respiratory microbiome the skin microbiome or as an all-encompassing term to refer to all micro biomes on or within humans so microbiota really is the more proper term when we talk about the actual organisms that really has been the focus of most studies today surveying catalog II understanding what's different in particular site or niche compared to a different patient group or a different site and and those that's sort of where those the technology and the wealth of evidence has been today is focusing on the on the description and understanding of what types of micro microbes differ and so these microbes largely a focus on bacteria to date but obviously in compost fungi viruses helmets in a another tree of life out branch called archaea which are more common in the gut we think than other body measures but really microbiota is a part of the definition of microbiome and so we try to become more attentive to that so now I'm going to move briefly into the reviews mendeavors linking the micro early life two childhood asthma has a set up to understanding why what has informed our thinking about studying this in the context of adult lung disease and this is an immense field which would be a talk or class and of itself and so I certainly don't have time to go through all that but I wanted to show you highlights from studies or lasting in 10-15 years in different spaces but first of all I wanted to highlight the idea that inappropriate responses to microbes or how we in candle responses when the body is exposed to microbes it's sort of embedded in some of what we do know about as a susceptibility genes and so this is a summary review that was published by Dunn Auto vercelli who's a geneticist at Tucson a couple years ago now and really summarizing all these genes that have been associated in jiwa studies or any sort of studies over the last twenty years being associated increased risk for asthma and they can be grouped broadly into three groups so I'll start down here at type to th to affect your functions which we think of most of all in a context as my allergic disease but certainly not all allergic medicines but there's certainly genes involved with type 2 immune functions I've been involved in that I mean you see io4 aisle 13 aisle 5 showing up here there's also polymorphisms and genes we thought thought to be involved with innate immune responses and microbial recognition and you know regulation at the mucosal barrier and that includes to not toll like receptors not like receptors and other mucosal surface genes that have an associate with increased risk for asthma in large-scale studies and also epithelial genes again this is sort of an eighth indian class you see defense and showing up here chemokines involved with instigating the innate immune responses that then feed adaptive immune responses so there's suggestion that susceptibility genes do play a role or somehow involved in microbial recognition recognition microbial molecular patterns could you know plausibly be somehow involved in the pathogenesis of asthma in the context of microbiome differences so here in microbiology and history as you probably know this is my prelude slide to basically return to the thought that asthma is more of a contemporary disease and our life styles have changed over the millennia millennia right so in the very early days you know we were very very much intimate contact with our animals and lived in environments that are not at all so you know very sterile by today's standards to enter an era where we are you know living in much more close-knit spaces and then daily antibiotics even early in life and get lots of infections and essentially asthma as a mod is a more of a modern disease right is we have had dramatic changes in home environments living standards what we eat the exposures we have and there's all feeds into the hygiene hypothesis that you've heard about that we've had a decrease in infectious diseases that kill us but arise in allergic and autoimmune diseases over the years so this is sort of a schematic I've had in my head over the last couple years in terms of how I think about where microbiome fits into the asthma clinical research and translational research there's been intense focus looking at this end of asthma susceptibility and asthma pathogenesis is the pediatric early life literature and those are largely focused on looking at environmental differences that are associated with asthma risk and I'll review one or two studies in that area but gut microbiome which I'll touch on very briefly with one highlighting one study and in recent years and then the rest of my talk is really going to focus on the respiratory microbiome so the start of these very rapid review slides so there's been an immense amount of epidemiologic literature over the last 20 years from large sales studies in Europe as well as in the United States suggesting that perinatal early life exposure to a diverse repertoire of microbes is associated with decreased risk of allergic diseases including asthma and as I mentioned there's epidemiologic studies as well as basic studies and some of the examples are really about come from Europe and some beautiful studies done by Erika vom useless at in Munich who's a pediatrician pediatric allergist where she's looked at various and systemic systematically at populations of kids who grew up in farms and very traditional farming environments versus kids who grow up in an urban environment and it's very clear from data from their study as well as other converging with other large-scale studies in Europe that the more exposure you have in an environment associated with increased microbial richness in this case measuring either endotoxin or the actual number of different types of bacteria fungi found in the mattress dust of kids who live in farms in these very intimate environments traditional Bavarian farms associated with decreased risk of asthma sleep Parsifal and Gabriella or two large studies this is a vacation came out England Journal several years ago now and basically the more bacteria you have less likely you so well you have more bacteria here but also living on a farms associate increased bacterial richness the less likely you're able to have asthma in this other study where they looked at fungal richness and the same samples again that frontal richness is increase if you live in a farm compared to a cohort of children who live in the same area but not in a farming Varmus a more suburban control population also decrease risk of asthma of the years and this is a figure that Erica likes to show at different meetings showing a mother who is a farmer whose baby is basically going with her to work every day is sitting right there next to a cow the exposures occur very early life and even perinatal II and so we that's beautiful window and this has been replicated in other studies including the states here showing that exposure to dogs and cats and early life may be associated decreased risk of asthma and later childhood so what about the gut microbiome so a very very broad statement again differences in the gut mark around early life have been linked at risk of developing allergy nazma these are just a snapshot of studies there's studies going back to nineteen ninety four we're using culture based methods that have shown increased relevance of certain bacteria that got being either associated with increased risk of asthma protective against that as well and why is that important I'm probably preaching to the choir a little bit but we know that the early you know first year alive in particular first twelve months twelve to twenty-four months later a critical window for new development we're born mostly sterile we think and the gut very quickly becomes established with microbes and that diversity rapidly changes in the first year of life and so anything that sort of get perturbs that that developing microbial system which then trains the immune system in its development to recognize what's what's dangerous and what's not dangerous is all really happening that first two months of life and so perturbations like perinatal antibiotics pose your PA advice giving to kids how you were born because if I c-section versus vaginal delivery has associated with how that inoculum occurs and shapes of gut microbiome and subsequent immune development in a very first ability of life so it's a beaut as a critical window to establishing we think the balance between th1 th2 immune function as well as tier agency 217 functions so as I mentioned there's a lot of studies in this area these are just some of the bacteria and I got that had been associated with risk of asthma such as colonization with clostridia vector B fragilis or e-coli or protective probiotic species that you've heard about like the Phaedo bacteria lactobacillus either by culture based methods in the early days or targeted pcr methods have long been associated either increased risk of asthma or protective against asthma more recently there have been these high-throughput molecular studies using sequencing methods and I'm going to highlight one study that came out of the Canadian longitudinal child birth cohort study which is run by Brett Finlay out of Vancouver at UBC and this is an amazing study they following hundreds of kids from basically you know before they were born in and up until I think five years of age now maybe longer and this is the paper that came out a couple years ago where they basically analyzed samples fecal samples collected very early in life starting at birth and I think at 3 months of age and non-word looking at associations between patterns of gut microbiota gel and using these large scale tools and how that was associated different disease phenotypes that are harbingers of asthma in the young course so you can't really diagnose as when kids until they are age 6 but these terms on how they classify these kids are ways that pediatric asthma researchers look at this and in particular I want to focus your attention on the atopic and wheeze phenotype those are a topic and have a persistent wheeze phenotype are thought to be the harm athough the predecessor to asthma diagnosis eventually in later childhood so they notice in their large-scale study that the atopic Weezie children later on at three months of age are very early like already had decreased numbers and richness in these particular organisms and I won't go into the elegant basic science translational studies where they basically took these organisms that were pulled out of an eighth of a queasy child and put them into germ-free mice to see how it impacted allergic immune responses the airways but essentially reconstituting these germ-free mice with these organs decreased allergic inflammation lungs of the trampy mice but in these kids very early on that's with this pattern of the decreased diversity and certain organisms already had different profiles and short chain fatty-acids measured in their stool and short chain fatty-acids are thought to be an immune modulator Tirol protective and in foster epithelial cell health and they got they also had different urine a metabolite levels already at that very early age so this are and they didn't see this at six months of age this is only at the sort of very early time point samples they saw this if they saw this difference associate later disease phenotype now people have also started looking at the recipe tracking kits it's very hard to study the rest for tracking kids without good reason from IRB perspective so a lot of the studies in the pediatric realm have leverage looking at what they call either hypopharyngeal samples or nasal pharyngeal samples usually swabs and so there have been some nice studies coming from large birth cohorts again from mostly not sitting on the United States them and I'll highlight the Copenhagen birth study in the next slide there's emerging evidence that upper airway microbiota either in the nasal pharynx or in the upper pharyngeal region in early life are associated asthma arrests suggesting that differences the microbiome composition may modulate susceptibility to viral respiratory infections and viral respiratory infections in particular RSV or RV have been strongly associated with risk for developing asthma later in life in childhood so I don't have time to go through the other major studies in this area but I'll highlight this so that you may be familiar from now more than ten years ago from Hans big scar that was published in England Journal in 2007 I think this was the first study not using a sequencing based method by using just traditional culture method but he took hyper pharyngeal swabs from babies at one month of age very early on and then basically made them for traditional culture based methods and found that the the likelihood what if you're already colonized in that space with either strep pneumoniae and maracas silicone or Alice or home office influenza but that was an associate with increased risk of persistent wheeze or asthma by age six and so the years is that this is a table from that study and the figure from the study that you had increased risk developing that phenotype over that follow-up period after they initially sampled the kids the odds ratio was pretty high here four and a half from being asthmatic at age five or six if you're colonized very early in life so that window is really really critical and I can tell you then the literature in that realm the window is getting pushed even earlier and people are even talking about the perinatal as exposures and placental exposures and that's so I don't do personally but it's suggesting a lot of the factors may even be predate potentially the actual birth okay so I wanted to move into then pretending to use discussing with you some of the recent evidence linking the airway microbiome to asthma phenotype and adults and this is work that I've been involved with over the last six years through multicenter studies funded by the NIH and other entities and the rationale for looking this is one I'm an adult pulmonologist we deal with patients already have established asthma what can we do to better understand the potential pathogens of the certain subtypes of the disease and potential interventions and understand it better so this is again a summary of how I've thought about it and instead of looking at the microphone at this end of the life spectrum looking at this in the studying of an adult asthmatic who may have one of hundreds of different phenotypes and how does the microbiome impact clinical features of asthma how is it shaped by treatments that we prescribe for asthma and how does that relate to the dichotomy of phenotypes we talk about anything figured th - hi vs. th - low phenotypes so I would argue that opportunities for microbes to shape and span the age spectrum so these factors that pediatric asthma our researchers have focused on looking the dietary intake airborne pollutants exposure and kids who live close to major roadways microbe exposures and about these are all things are not static right based we've continued to be exposed to those things as adults and so why couldn't they potentially impact on the microbiome and and disease phenotype in chronic airway inflammatory airway diseases and coupled on top of that we get comorbidities as we get older right so obesity bad oral oral health sinus disease these are off-again factors and associated with worse asthma outcomes in general and then I think an area that's actually been neglected I won't really talk about is there's not a whole bunch of literature in it is I give elderly asthma the idea that the list those observation clinicians have long had of adult onset asthma that's very severe and in particular being worse in people who are elderly defined as greater than age 55 or 60 in general how does that play a role we do know that there are age-related changes and then gut microbiome itself could that potentially play a role in the lung disease phenotypes we see such as asthma in order adults so if you're not familiar with this I thought I briefly go through this landmark study from 10 years ago highlighting the relevance of type 2 high versus type 2 of azmuth phenotype and the corollary here would be using affiliate versus non eastin like asthma which islam be recognized in the literature but this was the floor the first study done by my colleague Prescott Woodruff at UCSF back in the day looking at this in a molecular fashion what they did when their cohort was to take their cohort of asthmatic patients at UCSF and basically treat them in health the tick is ohm I think it was meticulous own for I think a six week eight week period and did bronchoscopy before and afterwards and then they also had a group that they treated Sasebo and before now and they had stratify these patients beforehand based on microwave Alice's they had done some years prior to finding molecular genes genes in the epithelium that responsive to aisle 13 which is the canonical th2 cytokine and these three genes that they focused on repair EOS and click on one and certain v2 and you can see from this heat map here that there was a type 2 high th two high group of asthmatics here and a th two low group here and this tht low group very much knew this YZ and ages in here so they were kind of very similar to some of the healthy controls in this particular population what was dramatic is that when they looked at the response inhaled corticosteroids defined by a change in lung function f vb wine after that eight-week period they only saw a significant improvement in that lung function in the group that was th too high defined before hand and no not really in your response in the th too low group and so this paper got a lot of press at the time sort of validating what had been clinically observed that cortical stories work better against eosinophils inflammation in asthma and now the the idea of stratifying patients by type 2 hi inflammatory profiles you know sort of as important because in addition to corticosteroids we have these immunotherapies biologics anti hole v al for therapies that come on a mark in the last five or six years that are available to treat people who have more of a type 2 hydra process so a lot of criteria for treating patients with one of these drugs is for now based on blood yo levels of at least 150 or 200 if I know in which drug you're looking at so we really don't have any good therapy fees for th to low asthma as yeah and we also don't really understand what dries th to low asthma and we have no doubt that there's many phenotypes and probably different molecular mechanisms that underlie th to low predominant profiles and some asthmatic patients so now that over the last 78 years there's been a wealth of growing studies that suggest that features of asthma associate with different area microbiome patterns and these come out studies not only that I've been involved but with other cohorts that have been publishing in this space now including koishi at University of Chicago cohorts in Australia as well as in Denmark and some of the clinical features that have been associated with this and that I'll go through in the next following slides include markers of airway hyper responsive that we measure clinically the severity of airflow obstruction stability of asthma control as well as obese versus non obese severe asthma and also responses to corticosteroids and response to macro fighting antibiotics had an associate with differences in airway microbiome patterns and of course related to that is airway information immune response patterns and I'll just tell you that you know try to convince you that both of the data so far suggest that the rest tree microbiome least bacterially is more different in those who have referred only type to low phenotype disease and not so much the type to high population that have been looked at to date so these two figures here in some recent figures from two papers that came out very close to each other as you can tell the first one was the very first paper we published out of the asthma clinical research Network where they were doing a parent trial looking at the effect of clear therm iesson as the control based on whether or not there was evidence from bronchoscopy that was performed in the patients of being infected with mycoplasma chlamydophila pneumoniae so in the chronic asthma airway disease real Islam been this idea and in many studies and decades prior suggesting that certain sensitive asthmatics or chronically colonized when you look for by molecular from the like like molecular methods with either of those organisms but macrolide studies have generally been some negative and this parent trial now as a clinical research network also was some negative but as part of that we took the opportunity to do to propose a proof-of-concept study and look at the microbiome using a micro Rachael we have the time to look at the bacterial community composition based on something called a 16s ribosomal RNA gene and when we looked at that cohort of asthmatics who are pretty much moderately persistent asthmatics on a standardized those infants which the zone and compare that to the healthy controls we noticed that the asthmatics on the whole had a higher measure of total bacterial burden this is basically a proxy for bacterial burden where we do 16s gene qpcr assay a couple years later around the same time for Nana Martinez and in Tucson who is a major pediatric asthma researcher looked at their cohort of adults at that point and these are patients who were not most mostly were not being treated inhaled corticosteroids some more mild phenotype of asthma also showed that those who had as I seem to have a greater diversity this is a common metric use in microbiome research seem to have a higher diversity of bacterial communities in their sputum samples compared to non asthmatic so between two different sample types in this case protective brushings that we obtained by bronchoscopy versus feedom a suggestion that the bacterial microbiota composition differed in asthma versus health in that same NHLBI acrn study that I mentioned this was the first piece of data we has suggesting that the airway hyper responsiveness is a marker of airway reactivity was associated with differences in the diversity in a composition of bacteria and so what's shown here on the x-axis is methacholine PC 20 that pulmonologist will be familiar that's a measure of area reactivity so lower the value of peace between the more reactive twitcher your Airways are and we saw a significant negative relationship again with back this measure of bacterial diversity and very hyper responses this is a very broad metric of looking at community composition when he died down more deeply analytically and look at the specific types of bacteria you're getting as readouts on whatever platform you use we saw that this relationship was driven by airway enrichment increased abundance if you will in members of this phylum Proteobacteria and if you haven't heard that before I was keep that in mind Proteobacteria is a very large funnel but it encompasses a lot of the bad actors that we think about in recipes as well as in GI disease so it includes home office includes Klebsiella Moraxella and the gut includes enterobacteriaceae e-coli so it's a very big family phylum of organisms we then went on towards an assay to be involved with another multicenter study that was being conducted by genetic at the time looking at announced markers of steroid resistant asthma in a severe asthma cohort recruited across like something like 20 centers in the US this was all very severe asthmatics so even more severe than the prior the cohort that I showed you from the AC RN and they were all probably controlled despite despite being on high-dose inhaled corticosteroids they did a very simple observational study over approximately four to six week period where they brought them in characterizing deeply by clinical questionnaires as well as getting samples including bronchoscopy and sputum and we again proposed them well hey we've done this before with a more a less severe cohort if you've got brushes from the scene from this cohort wouldn't same sample type we could take a look at that and compare it to the other qohor and that's exactly what we did importantly within this observational study they were now allowed any clinically significant changes during the study and no medication changes and so again we didn't exploratory analysis with all the meta data clinical and inflammatory that they had collected so what I'm showing you here is something called a non metric multi-dimensional scaling plot and it's a big word but basically it means distilling down lots of different information into a point and mapping them out so each of these points here if you've ever seen something like a principal component supply it's very akin to that just a different statistical methodology each point basically represents the some bacterial community in the bronchial brush of a given subjects we analyzed about 30 out of 40 subjects in this study and what's superimposed here are these vectors and these are what we call gradient vectors and and what's labeled here are some of the variable names from the metadata that we looked at that were came up as being significantly associated with differences in community composition so the direction the vector gives you a sense that maybe some of these factors associated with say differences in asthma control defined by this a questionnaire we use in asthma clinically called the asthma control questionnaire or a number of leukocytes in the sputum might be associated with a slightly different community composition compared to say body mass index in this cohort and that's what I'm going to dive into a little bit more than that's a couple of slides so out of all the variables that we looked at essentially we saw associations between differences in bronchial bacterial community composition microbiota composition and stability of asthma control in this population over a one-month period obese versus non obese patients in this cohort and markers of steroid responsiveness or type two inflammation so this is the data from the obese versus not obese severe asthma patients in this cohort and when we looked to basically you know separate them into those two groups and looked at what differ between the group and between the groups in terms of the effect and in terms of their bronchial bacterial community composition there would be severe asthma patients were sniffing and rich and quite a few organisms and these two other file look Bacteroidetes and Firmicutes and these are organisms we don't haven't really had up until this point really thought about in our disease I mentioned Proteobacteria before and so this was really kind of striking to me at the time when we when we came upon this in our analyses because these are the two dominant phylum of organisms in the gut and these are a lot of anaerobic organisms and so it suggests to me and follow studies have yet to be done in terms of looking at the function of these but for some reason the obese severe asthma patients in this particular cohort seem to be enriched in some of these anaerobic organism more associated with the GI or a pharyngeal cavity when we looked at asthma control within that one-month period so in the design of their study they had assessed as when control within a four-week period using the acq questionnaire again they had no clinical changes detectable by the patient and somebody yeah at the same time a subset of patients seem to have indicators of worsening asthma controls or positive change in this acq metric indicates worsening asthma control and those zeros for zero change or negative change on this particular questionnaire indicates to improved asthma control and and basically correlated you know what was associated with those directions changes in the direction of that score and again overwhelmingly the organisms that were so strongly positively associated with indicator of worsening asthma control these less stable asthma control where mostly this proteobacteria group of organs over 90 percent of the of the bacterial groups that we identify were correlated with that whereas the converse a very different bacterial group called actinobacteria were correlated with evidence of stable or Lisa or improved asthma control and I highlight those in blue and red here because they're very different file in the bacterial Proteobacteria as I mentioned represented a lot of potentially pathogenic organisms at least an arrest rate track as well as and they've got actinobacteria not so much they're actually more incompass organism the environment of environmental organisms they're very prolific makers a secondary metabolite so we get anta by and microbial compound that we use like streptomycin neomycin come from members of that tea no bacteria class so just vent about the very different group of organisms now in this parent and a study the our collaborators genetic had done epithelial gene expression profiling and so gave us some information on those gene expression readouts to look for associations with the microbial readouts we have profile at least bacterially and when we looked at out of the for gene expression signatures they showed they gave us which include a th two gene signature like the one I showed you a couple slides ago this pattern what they define is indicated of steroid responsiveness basically expression of fkbp5 which is involved in the glucocorticoid receptor engagement as well as stoic resistant pattern mostly defined by il-17 responsive genes aisle 17 pathways have generally been thought to be more steroid resistant in terms of their treatment response in patients and we looked at these two signatures were the only two out of the four not the th two one but these two signatures came up with significant associations with members of the bacterial community and that's shown here and this plot here so what's shown in F here are the organisms that were sniffing associated with a steroid responsive pattern and what's shown in red here and overlaid with speedom neutrophilia which kind of goes with at each time the il-17 neutrophil chemotaxis type of pattern or associate with a very different group of organisms and what were the organisms what were the phyla that these organs belong to again proteobacteria and Actinobacteria and so remember on the previous slide that the actin over here seemed to be associated more stable or improved asthma control where it's pretty back to here again were associated more less stable control in the previous slide so it would seem to dovetail nicely with the clinical readouts we were showing on the previous slide so I mentioned that the DTH two signatures surprisingly in size we didn't see any signature associated with that we did we looked high and low but did every possible metric including disputed eosinophils biopsy sniffles etc and just really didn't see any correlates from the bacterial community at least markers of type two inflammation and what we notice is that we might back and look at these data as I mentioned we notice that those in whom we could look at the bacterial component of the airway microbiome those patients in whom we could do those that do that profile has typically lower sputum eosinophils seem to have lower biopsy numbers and we actually did the a quantitative PCR looking at bacterial burden in those samples there was a negative relationship between that the number of bio sleeps in the fills of taken from these patients so we started have this emerging feeling that maybe the bacterial community differences we were seeing in the airway microbiome might be associated more with a non type 2 type 2 low inflammatory profile in the lungs so the question we would always get up until this point we were designing the study as at the same time as all these patients are on held corticosteroids what is the effect of inhaled corticosteroids which are prescribed so widely in in pulmonary medicine so many years ago now we sought to design a very simple proof of concept study within the NIH asthma net consortium we started this when I had my K award we're still analyzing data from it and and this is Lang was very straightforward and descriptive and basically we thought we'd enroll three groups of subjects allergic asthmatic a 12-egg asthmatic subjects who really had not required inhaled corticosteroids are very mild asthma clinically and enrolled two groups of control subjects non atopy non-allergic healthy controls as well as a group of people who had allergic sensitization to aro allergens but didn't have evidence of osmond that we test before in the trial and then we put them through bronchoscopy as well as Speedman collected samples and then when then the asthmatic group we randomized them to inhaler take the cell versus placebo for six weeks and study them again afterwards like did a bunch of specimens that a lot of profiling of immune responses as I mentioned here and just to give you a snapshot of some of the findings again most of these subjects seem to have type two low profiles was kind of surprised as a little but least by the the way we approach defining type to inflammation site again based on an expression of these il-13 useful epithelial genes only about 10 over 40 asthmatic seem to have a type two high profile so most of the data again focusing on the bacterial community seem to be focused on the non type 2 type 2 a population that's capitulate here again when we looked at bacterial burden my access between the type 2 high versus type 2 low subjects typically more and type 2 those subjects although admittedly there is a spectrum here and I think that gets that you know the heterogeneity within the type 2 low population when we looked at the bacterial communities and again in the protective brushings we collected at bronchoscopy from these subjects and plow them out and compare them side-by-side this slide summarizes that's all I'm showing you here the names aren't really that important for the purposes here are all the bacterial groups defined by sequencing that was sniffling associated with either the asthmatic group with a utopic group and what's shown here in the columns are the what are they or guitar the groups bacterial groups that we think are strongly associated Iowa asthma either with atopic status and we reason that when we did the 2x2 comparison comparing the asthmatics to the healthy non-allergic group as well as the asthmatics to the allergic but non asthmatic group but if you saw blue bars or red bars across both of those comparisons that the likelihood would be more strongly associated with asthma the evidence is stronger there and that's what's highlighted here and that certain organisms like the fuse of a bacterium which is an anaerobic as in both of those comparisons as well as not a member the hemolysis rip here there's some names here whereas private Ella again an oral usually an oral associated organism but we're finding more and more of it in Hmong studies anymore so she with atopic only pattern so if you I flip back you get the sense that a topic only group though we're going to since our associate with atopic status without asthma was just seeing just as striking and that was a little surprising to us but we thought to be an important control group because so many as Matic individuals are allergic is there something different about being allergic versus non allergic in asthma and so from this data we would submit that controlling for a topic status at least in airway asthma studies is likely important because we don't really know what the effect of atopic sensitization is on the microphone although people who study food allergies and the gut microbiome have reported differences and they've got marker balance I think there's some some some evidence totally non there about whether atopic sensation predisposes you to being colonized by organisms more readily when we looked at responses to the inhaled corticosteroids so here's the caveat during bronchoscopy studies for microbalance science and scale is that was very hard to get paired samples from patients before and afterwards it's just differences an operator collection of samples patients and cells even in a multicenter study so we didn't feel very confident in showing some of the pre and post data but we did look at the baseline community differences in those who seem to show response inhale course cards even though they were mostly type 2 low versus those who did not respond then we define inhaled corticosteroid sponses as an improvement in bronchial reactivity by this clinical test and we looked at the baseline pre inhaled corticosteroid delivery to these to these asthmatic subjects we notice that baseline those who seem to show an improvement their methacholine PC 20 it seemed a different baseline in their bacterial community opposition compared to those who do not the y-axis here without going too great does is basically readout of how the different communities are between compared to group in this case comparing it to the reference group of healthy controls and there's a difference there between those who did respond to steroids versus did not respond to stories versus not and then when we use a bioinformatics tool that's out there to basically try to infer what bacterial communities can do metagenomic ly with kind of genes aren't potentially encoded in their genome a lot of the pathways that came up in the database seem to be associated with metabolism of xenobiotics and drugs and an external compound suggesting at least to my mind the possibilities and amid least speculation it's still at this point that there's something different about the community and those who can't respond destroys and those community seem to be enriched in gene content that might be associated with being able to metabolize xenobiotic compounds okay so here's a summary of sort of the data today so you know we've looked at this the role of raspberry micro balint in the setting of type two high versus type two low inflammation I hope I've convinced you at least with the day or week early on hand that when we look at the bacterial component of the airway microbiome that it seems there seems to be more of an association between differences in bacterial community composition in the airways and type 2 low inflammation as opposed to type 2 high inflammation on which i think is really interesting and we think we see in effect with inhaled corticosteroids as well you know okay so in the time remaining I thought I'd discuss them the challenges in new directions to understand how a microbiota influence asthma phenotype so as I mentioned with a previous study with it from the NHLBI as Ned is in terribly hard to do a bronchoscopy and although I don't have time to go into some of the data we've more recently generally looking at different specimen types including sputum as well as nasal brushes it's really a sort of a hindrance to doing longitudinal studies and I think it's really important in chronic area disease to be able to do longitudinal studies if you're looking to look at disease phenotype as well as the microbiome and that really hasn't been done because this is really hard to do longitudinal studies using bran to reblog patients and convince patients to participate in studies where we're going to do repeated bronchoscopy zon you and so I think there's a mean in our field to sort of move and try to validate other specimen types in particular I think induced sputum is promising but it's also much more complex on the other hand there's a lot of background in as on COPD research validating the use of looking at induced speedom and immune inflammatory markers and how they relate to disease outcomes in those diseases so somehow I think it'd be nice to be able to leverage looking at the microbiome represented in induced feedom to infer lower airway microbiome composition that you might otherwise obtain by brush Missoula lodge but really we have no idea of this stability of the microbiome in chronic respiratory so with the exception of cystic fibrosis where there's been a lot of literature in this over the years and even in cystic fibrosis which is a unique clinical context it's pretty stable but yet when they have exacerbations and CF they do see a perturbation in some patients but not all in their microbiome but we really have no context for understanding that in the setting of asthma there's a little bit of data this in COPD but there's a lot of work to be done there and I think that's terribly important because if we think that microbiome information might be incorporated into phenotyping schemes to better understand the phenotype of a patient I would argue intending to understand what foundation we're looking at what's the baseline background stability if you're going to develop a predictive marker how does that compare to the background variation over time as in a predictive model is sort of important to know also the functional implications of microbiota differences how are they linked as a phenotype and this is a huge area in ascending of itself even people who say that gut microbiome wrestled with and tenders for focus on individual species how to get at that and understand how a microbial how a specific micro functions not let alone in an ecosystem of other organisms that they are living in the same neighborhood as and so the challenges here are complexity at two levels complexity in the microbiota microbiome level diversity strain specific or high hours GC specific functional diversity and all the data it's an immense challenge and I would say even those in the gut microbiome space who've been doing this for decades I think still struggle with this with this with this challenge and we've also overwhelming focused on bacteria and largely ignore fungi and viruses of what people might call the microbiome or the viral and and they come in and of themselves with challenges in studying because how you process those samples look at those elements of the microbiota that are different and when you're working with something other than stool which is more readily to get it becomes very hard to make decisions upfront about how you're going to take your sample process that for the different purposes you'd like to like to like to do with that and then couple that with the patient phenotype which is very different from a mouse phenotype in that in that there's so many more factors to look at so many more elements that can shape the microbiome and I won't grow through laws but we certainly know that you know what the transcriptome and what these gene polymorphisms actually do in terms of it conferring susceptibility to as still not quite understood and then aspects of epigenetics and environmental exposures might further modulate host immune responses how does that all integrate itself with the the microbiome and and other readouts we get of how the host is responding in the in a disease phenotype so really in the space of the restroom microbiome research we've largely focused on microbiota composition understanding who's there and what's different and it's descriptive it's it's it's very basic but it's basic stuff that has needed to be done and probably still needs to be done in the context of large population studies when we look at different disease phenotype so you really can't compete chelate I think as well in mouse and mouse or animal models and people have started to look at function try to infer what these microbial communities can do using in silico tools developed by computational biologists and engineers which are helpful but ultimately you know we need to sort of be moving more towards integrating if you're an omics type and delivering these different technologies and different platforms that look measured different readouts of what the system puts out and so one area that we're focusing on with a cohort that I'm building at Michigan is using metagenomics focusing on the microbial community to understand what is it whether the genes encoded by these microbes and what are they potentially can do and eventually hopefully and coupling that with meta transcriptomic so the mRNA the gene expression readouts from the microbial community and as well as these readouts of the actual protein products and/or the met up in tablet products to actually mediate these interactions so as Jana Janssen who's a big environmental microbiome scientist out it in Washington State published in this journal is really the song at the phenome the phenotype if you will of a microbial community how does the interface of the phenotype of the human disease context I would say that this cannot be done in isolation because you really understand the mechanisms we still need to continue applying traditional experiment microbial culture work and be sure and evil work leveraging patients and most to really bring it all together so summary some three points I hope to leave you with is that I hope it conveys you the lower recipe microphone as well as well as in chronic airway diseases which I didn't have time to show you data from there first women in health it seems to evolve in parallel with disease advancement and in the clinical context of studies very hard to tease out what's chicken in the egg is if there's a very diseases driving the micro violent changes or vice versa and I have I think it's probably no doubt bi-directional but it's difficult to detect that in a clinical context microbiota associations clinical features and as most seem to implicate microbial influences on as for phenotype but as I mentioned the by directionality of these links needs to be further study but I think is really intriguing and might be maybe gives some weight to some of the people who in decades passed and the pulmonary rule really felt like macrolides helped us there was such a high population subset of patients but how do you actually identify those patients and define them to say who's going to most likely benefit from microbiome or microbiota targeted intervention I still think foundational studies are still need to address microbiome disease phenotype relationships and different sample types we start to do this with induce sputum as well as nasal pharyngeal samples they're very difficult samples to work with but it'd be nice if we're going to eventually in in the future remove this to a clinical realm where you could take a sample and understand what the microbiome is and how that relates to the clinical disease phenotype or your bloody sniffing level etc we need to be able to do this outside from convinced easily do a undergo bronchoscopy for a clinical indication and functions the library by human microbiota impact lung disease as I mentioned is still very basic stuff that needs to be done that will most like take another generation probably so with that I'd like to end and thank you for inviting me some members of our asthma and COPD microbiome research group at the University of Michigan and collaborators at UCSF and senior investigators at Michigan clean Gary huffnagel and Maine law and Han and as always grateful for my funding to allow me to do stuff that's still fun to me so thank you very much thank you I guess the major message that I take away from this whole field is that my human body is nothing more than a vehicle for bunches of microbial microbes maketh man so let me just start off the questions with asking you is there any evidence that the composition of your microbiome is influenced at all by blood type or tissue typing garbage great question I don't know that I'm not familiar with any studies that have looked specifically at blood type but you raised interesting related sort of body of evidence where people have looked at blood Titans to suck belly to viral infections in the gut such as such plated norovirus infections John fight UCSF several years ago published data looking at suddenly two viral respiratory as asthma exacerbation associated with presence of the H antigen on the epithelial so so we looked at so there's connections there with susceptibility to being infected by viruses I will say that there has been a study that attempted look at this is not in the monkey activist realm and I believe that study also seemed to show an association would be more likely to be colonized with Pseudomonas and non CI Frankie ecdysis would take your blood types I forget which one so people are starting to look at that cuz that data is there and be able to do lewis antigen typing - as additional metadata to look for Corliss is there but right so EBC you exhale breath condensate you know is a sample that we can collect I can tell you that with attempts to analyze that sample type to look at DNA or microbial microbiota composition it's very difficult and we really don't see that there's not enough cells and DNA there but to answer your question about in the time when people have looked at the metabolomic along using lavage fluid to start as they've collected it from their bronchoscopy based studies I will tell you there's debate in the field at least about sort of how you analyze that metabolomic data in a sample that's you create and how you normalize that and so there's debate about how how you go about that but people have attempted to measure metabolites i gc-ms or lc/ms from lavage fluid I'm not familiar with other specimen type specific yeah I haven't seen data where people looked at exhaled breath patterns like volatile VOCs and stuff and correlating that with microbiota that be actually we are going to incorporate that in the study that we're doing at Michigan where I've linked up with a biomedical engineer who has an exhale we basically could collect exhaled air and apply it to a portable lcms platform that he has to look at you know real-time readouts of that breath so down the road we hope to be able to do that if we get that up and running it's possible yeah although you know there's robust literature in the world looking at either EBC exhale air or lemon tabla and so I think I think the start is to be is to be focused and my goal is to with this platform is to first focus on those compounds I have put in published in literature that seem to be have been have been associated with asthma or asthma exacerbations and and go from there the actual source whether they're truly from the long verses or fair I'm not sure that that's been well determined so in the adult world there hasn't been that much done yet we are starting to that in fact a upcoming meeting I'm going to present some data from our cohort we've looked at the gut microbiome the subset of our cohort Michigan and are seeing some intriguing patterns between gut microbiota composition and markers of asthma including lung function it's very preliminary data I think that one of the challenges in Italy is that so many things can influence the gut microbiota in stablish and literature and I think you know from analytical spam or how you dissect the relative contribution those other factors I have an Associated difference then got michael Baughman can you can't control for everything but trying to control for them as much as you can but I think the real I think the story where this may come more more readily fleshed out student would be the obese asthma story because obviously obesity has been associated with many different things including the gut micro systemic markers inflammation and almost certainly it's got up you know via bottom-up influence on susceptibility to until the lung disease and asthma like phenotype so you see very simple changes changes in bacteria acting up bacteria and also changes and short chain fatty-acids and we can get you to rate and basically totally rates has a genetic effects we have not finding of we've we we haven't even actually at least an asthma world start to look ugly I've made attempts actually trying to measure short chain fatty-acids in blood and the lungs we've run into some technical difficulties associated with that to be honest I will say in that figure I showed you of the data from asthma where we try to infer some of the bacterial community functions from those organisms that were associated with asthma the short chain fatty acid pathway came up so it's of interest at least when I've talked to the people work in the Tattler rec realm and and talked about trying to measure short chain fatty-acids and something other than the stool there's concerns about sort of what the levels are the assays are sensitive enough we'd like to but we haven't done yet done it yet outside of the good
Show moreFrequently asked questions
How can I make documents so that someone else can electronically sign them?
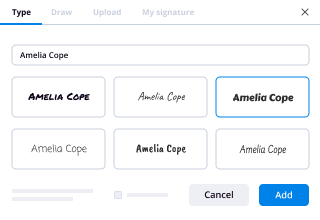
What do I need to sign a PDF electronically?
How can I eSign PDFs?
Get more for signature block Doctor's Medication Order Template for Campers made easy
- Print electronically sign Liquidating Trust Agreement
- Prove electronically signing Bug Report
- Endorse digi-sign Early Lease Termination Letter
- Authorize signature service Photography Order Form Template
- Anneal signatory Animal Shelter Intake Form
- Justify eSignature Personnel Daily Report
- Try initial Summer Camp Activity Waiver
- Add Investor Rights Agreement eSign
- Send Fashion Show Sponsorship Proposal Template eSignature
- Fax Technology Assessment autograph
- Seal First Aid Risk Assessment electronic signature
- Password Debenture signed electronically
- Pass Horse Boarding Contract Template electronically sign
- Renew Basic Rental Agreement electronically signing
- Test Animal Surrender mark
- Require Consulting Agreement Template signed
- Comment guy signature
- Boost signer countersign
- Compel supporter signature service
- Void Commercial Photography Contract Template template esigning
- Adopt Restructuring Agreement template digisign
- Vouch Consulting Proposal template electronic signature
- Establish Community Service Certificate template countersign
- Clear Small Business Partnership Agreement Template template sign
- Complete Summer Camp Scholarship Application Template template electronically signing
- Force Resignation Letter Template template initials
- Permit Professional Medical History template eSign
- Customize Modeling Agency Contract Template template eSignature