Signed Electronically Hospital Discharge Made Easy
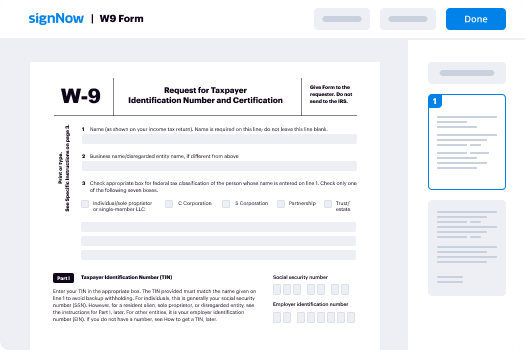
Improve your document workflow with airSlate SignNow
Agile eSignature workflows
Fast visibility into document status
Simple and fast integration set up
Signed electronically hospital discharge on any device
Detailed Audit Trail
Rigorous protection requirements
See airSlate SignNow eSignatures in action
airSlate SignNow solutions for better efficiency
Our user reviews speak for themselves






Why choose airSlate SignNow
-
Free 7-day trial. Choose the plan you need and try it risk-free.
-
Honest pricing for full-featured plans. airSlate SignNow offers subscription plans with no overages or hidden fees at renewal.
-
Enterprise-grade security. airSlate SignNow helps you comply with global security standards.

Your step-by-step guide — signed electronically hospital discharge
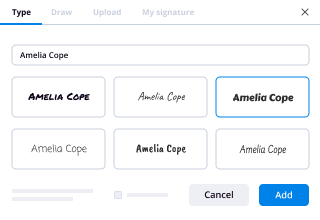
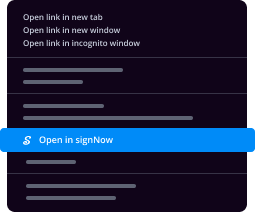
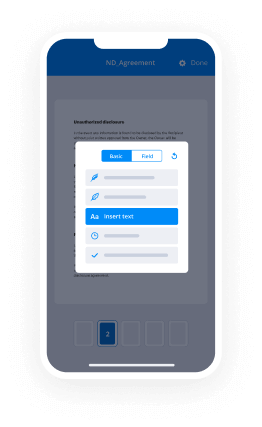
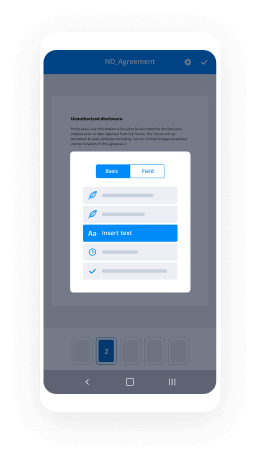
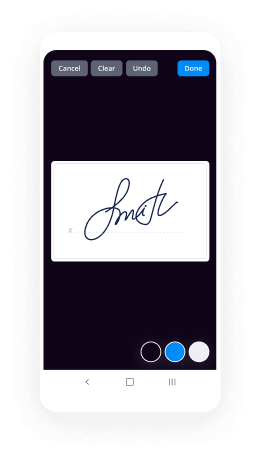
Using airSlate SignNow’s electronic signature any organization can speed up signature workflows and eSign in real-time, supplying a greater experience to consumers and staff members. Use signed electronically Hospital Discharge in a few simple steps. Our handheld mobile apps make work on the run achievable, even while offline! eSign documents from any place in the world and make deals in less time.
Take a stepwise guideline for using signed electronically Hospital Discharge:
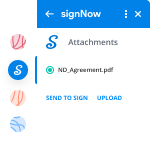
- Log on to your airSlate SignNow profile.
- Locate your document within your folders or upload a new one.
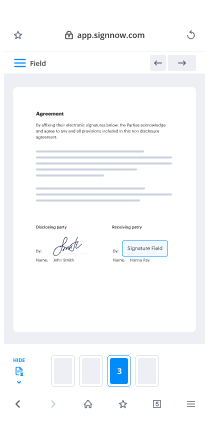
- Access the template and make edits using the Tools list.
- Drag & drop fillable areas, type text and sign it.
- Include several signees via emails and set the signing order.
- Indicate which recipients can get an signed copy.
- Use Advanced Options to reduce access to the record and set up an expiration date.
- Click on Save and Close when completed.
In addition, there are more innovative capabilities open for signed electronically Hospital Discharge. Include users to your common workspace, view teams, and track collaboration. Millions of users all over the US and Europe agree that a solution that brings everything together in a single cohesive work area, is what enterprises need to keep workflows functioning efficiently. The airSlate SignNow REST API enables you to integrate eSignatures into your app, internet site, CRM or cloud. Check out airSlate SignNow and enjoy quicker, easier and overall more productive eSignature workflows!
How it works
airSlate SignNow features that users love
See exceptional results signed electronically Hospital Discharge made easy
Get legally-binding signatures now!
FAQs
-
How are electronic medical records authenticated?
Authentication is an attestation that something, such as a medical record, is genuine. The purpose of authentication is to show authorship and assign responsibility for an act, event, condition, opinion, or diagnosis. Every entry in the health record should be authenticated and traceable to the author of the entry. -
What is healthcare authentication?
\u201cDigital authentication is the process of determining the validity of one or more authenticators used to claim a digital identity,\u201d report authors explained. \u201cAuthentication establishes that a subject attempting to access a digital service is in control of the technologies used to authenticate.\u201d -
How does electronic medical records work?
Electronic health record or EHR software is a system that allows medical professionals to quickly enter information on new patients, creating a digital record that they update with each new encounter. ... Practices use them to control access to patient data more securely. -
Do medical records have to be electronic?
The Electronic Medical Records (EMR) Mandate. ... A mandate requiring electronic medical records for all practitioners is a part of PPACA and is set to take effect in 2014. Some mandates included in the Health Insurance Portability and Accountability Act (HIPAA) have been included in and strengthened under the PPACA. -
What is the difference between an electronic health record and an electronic medical record?
What's the Difference? Electronic medical records (EMRs) are a digital version of the airSlate SignNow charts in the clinician's office. An EMR contains the medical and treatment history of the patients in one practice. EMRs have advantages over airSlate SignNow records. -
How does a health record serve as a legal document?
2. How does a health record serve as a legal document? It serves as the way to reconstruct an episode of patient care. This reconstruction provides the ability to prove what did or did not happen in a particular case and establish whether the applicable standard of care was met. -
What is the legal medical record?
A legal health record (LHR) is the documentation of patient health information that is created by a health care organization. The LHR is used within the organization as a business record and made available upon request from patients or legal services. -
Does Hipaa allow electronic signatures?
Electronic signatures are allowed under HIPAA and may be used for authorization. ... The authorization must contain the patient's signature and the date the document was signed. -
Do Hipaa release forms need to be signNowd?
A: No. The HIPAA Privacy Rule does not require you to airSlate SignNow authorization forms or have a witness. Though taking the time to fill out an authorization form and get a patient's signature is an extra step, it's an important one that you can't afford to overlook. -
Is airSlate SignNow Hipaa compliant?
yes! airSlate SignNow's eSignature method is HIPAA compliant, and we're committed to helping organizations meet compliance requirements across all industry practices, including health plans, medical equipment manufacturers, pharmaceutical companies, and providers. -
Is Sign now secure?
airSlate SignNow has a strong background in IT security and airSlate SignNow has established itself as a highly secure and efficient eSignature platform for any kind of organization. With industry leading features like Advanced Threat Protection and Link protection, airSlate SignNow keeps your documents as safe and secure as possible. -
Is HelloFax Hipaa compliant?
In summary, HelloFax may be considered HIPAA compliant. Although the company does not fall under the HIPAA conduit exception rule, it has the required security controls to keep PHI safe and also signs a business associate agreement with users of its services. -
Is eFax Hipaa compliant?
You Meet HIPAA Standards. For true HIPAA compliant Healthcare faxing, you can trust eFax Corporate®. With eFax Corporate deployed across your organization, your staff can securely fax by email from any Internet connected device including desktops, laptops, tablets or smartphones. -
Does HelloFax really work?
Our Verdict HelloFax makes faxing simple, while leveraging cloud storage. However, its lack of organized fax tracking and indexing makes this a poor choice for high-volume users. -
Is there a free version of airSlate SignNow?
Lastly, airSlate SignNow will be offering its users a free edition of its platform, in which they can sign up for a free account and receive 5-free \u201csends\u201d (documents sent and signed) per month, with no credit card required.
What active users are saying — signed electronically hospital discharge
Related searches to signed electronically Hospital Discharge made easy
Initial hospital discharge
well let's get started welcome to internal medicine grand rounds um today we have a one of our former faculty dr leanne wagner coming to us from university of maryland um leann and i known each other from the days of our hospital medicine back in 2009-2011 where leanne was a was a hospice here um you know i remember her finally being a very excellent clinician but since then she has migrated back to home institution university of maryland has done it quite a bit since then um she's still her passion still in teaching but she does enjoy a lot of extra extra clinical time of doing research on patient safety and usability she's on multiple committees across the university maryland system the school the hospital as well as the medical system itself i mean recently she's been the one as champion for the cope due to the covet 19. she also served as the president of the maryland chapter of of hospital medicine but her passion really is in the the patient care and once again a very important part of that is the transition of care in in medicine well i would like to give you a warm welcome but eventually you will come back to georgetown in person welcome so thank you amaran um maybe i need to move this box huh all right so thank you amaran it is wonderful to be back with you all even if just virtually to talk today about my favorite topic which is hospital discharge and share some ideas and strategies for making hospital discharge more patient centered so i am going to start us with this mantra of internal medicine discharge planning starts on admission i know that we have all heard this before at least one point during our career i remember vividly hearing this for the first time when i was an intern actually my senior resident wrote it up on the whiteboard in the team room where we were working and i remember looking at it and having that feeling of dread and overwhelm which i think is pretty common in turn year but thinking gosh i don't even really know what that means and i definitely don't know how to do it it is overwhelming to think about discharge during the admission process which is why you know even though this is our mantra it hasn't really become our practice our intentions are good though as internists we see ourselves as diagnosticians and we spend so much time trying to get that admission diagnosis right and creating the most evidence-based evaluation and treatment plan that as the patient convalesces through a hospitalization the discharge can sometimes seem like an afterthought i do hope to make the case though today that maybe never in the history of patient care has it been more important for us to keep our eye on this ball so to speak and to think about you know when we do start discharge planning early in the admission are we doing it in a way that truly supports the patient patients need us to get this right they are incredibly vulnerable during the discharge transition and frankly they're failing it in massive numbers so i think a good place for us to start is to understand the history about how hospital discharge became a care transition you know when was this gap in care born decades ago patients had one physician you know one doctor who took care of them usually their entire lives out in the community and then when they got admitted to the hospital the doctor came there and took care of them there too but with the rise of managed care in the 1980s physicians were tasked with seeing more and more patients to make ends meet and they were having a hard time getting back to the clinic to see or getting back to the hospital to round on their admitted patients so one of the coping strategies that emerged was this idea of the rounder where practices would designate one doctor usually for a week at a time who would go to the hospital and round on all of the admitted patients there instead of seeing patients in the clinic that week this was really the breeding ground for hospital-based physicians because it begged the question if the doctor seeing you in the hospital isn't your doctor but their partner could it really be any doctor so soon hospitals were hiring more and more hospital-based physicians and in 1996 the term hospitalist was coined in the new england journal by bob wachter since that time the two fields of general internal medicine seem to have split even more distinctly into inpatient and outpatient worlds giving rise to what amounts to a very clear handoff of care i both admission to and discharged from the hospital and even though this way that we practice has been happening for years you would probably agree with me when i say hospital discharge is clumsy still and disjointed rushed often with inadequate communication between the care teams and ultimately we end up leaving much of the responsibility for even the most complex care with the patient and we need to ask ourselves if we do that well and if we don't what opportunities are there to do it better so um to that end these are today's objectives we are going to discuss the consequences of an inadequate discharge transition we're going to walk through the components of the discharge process and look for opportunities where we can enhance patient understanding of their home care plan we're going to explore the concept of usability as it relates to patient-facing documents so why do we care about the discharge transition well first and foremost we're all here because we care about the patients we've created a care plan that works in the hospital but this is an artificial setting i often tell the teams you know we can fix most anything in the hospital but creating a plan that is sustainable for success at home is really the challenge we forget sometimes through our daily work how dangerous discharge is for patients we make well-intended changes here not thinking always about the downstream consequences when it was formally studied the adverse event rate for patients leaving a general medicine service at a tertiary center was 20 the majority of those adverse events were medication related and about a quarter were deemed preventable so even when we set out to help the patients with the best intentions we can hurt them whenever either one of these two things happens either a failure of our care plan to work at home or some adverse event related to the discharge plan the likelihood that a patient gets readmitted increases so you may think that maybe that's a second chance to get it right and it used to be that it was until relatively recently because medicare did pay for all hospital readmission care um up until about 2008 when they realized they were spending 12 billion dollars annually on hospital readmission care so they started to think about this concept of the potentially preventable readmission as a target for value-based payment and at about that same time this landmark article came out by the jenks group in the new england journal which really sought to characterize hospital readmissions so they looked at 13 million discharges from 4 000 hospitals across the country and they found that the readmission rate within 30 days of discharge was 19.6 percent so while that number is high staggering really one-fifth of patients returning within 30 days one of the key findings from the study was that the rates varied substantially by geography so the assumption here was that the quality of care at the time of discharge must therefore vary and the response was the creation of a program to incentivize hospitals to improve on their discharge processes so in october of 2012 the hospital readmission reductions program was started initially in those early years just those first three diagnoses you see there were included ultimately in 2016 the program expanded to include the other diagnoses essentially cms calculates the expected rates for readmission looking at a few comorbidities and any hospital with an observed rate exceeding the expected rate is penalized up to three percent of their medicare revenue for the year of course hospitals meeting their benchmarks are incentivized so i work in maryland and we have a unique relationship with cms it used to be called the waiver program but essentially we don't fall under the hrp program we have our own program with cms called the rip program it's quite similar in that we're judged on our 30-day readmission rates also they are risk adjusted for us though all payers are included as our all diagnoses so as you can imagine there's a lot of money at risk there's a lot of stake and a lot of interest in seeing if programs like this do work to reduce readmissions so after the introduction of the national program we see for those targeted conditions and non-targeted conditions the readmission rates did initially fall with the initial enthusiasm around improving the discharge process but as you can see the rates stay relatively high and level off particularly for those targeted conditions so if we intend to better support patients during the time of discharge and look at the outcome of readmission as you know the measure of that then we have to better understand what makes a readmission so is it that patients who are readmitted to the hospital are just globally sicker than other patients well sure some are but when we look back at the original jinx work it turns out that less than half of the patients who are readmitted were readmitted for the original diagnosis in fact the severity of illness at that index admission predicted poorly who would be readmitted so of course sometimes it is the disease driving the readmission but when it's not it may just be a failure of this discharge transition so if we think about a readmission that way we might consider it really a medical error many of you are probably familiar with the swiss cheese model of error for those of you who aren't it is a way of looking at the concept of layered security in systems it was first described by british psychologist james reason the idea is that catastrophic safety failures and big systems things like aviation and hospitalization are rarely due to a mistake by one individual instead processes have multiple layers they're designated by the cheese slices here and of course each layer may have some vulnerabilities designated by the holes but the idea is that these processes should have enough overlap between layers to prevent a hazard from becoming an accident so if we consider a readmission as though it's an accident we can look at the layers of the discharge process find those opportunities for improvement and implement those to reduce the risk of a readmission let's walk through the anatomy of a discharge to do that so the first layer is the plan creation this is really rounds right we diagnose we create a care plan but have we considered whether this is a plan the patient can carry out at home logistically financially whatever the case may be often patients get admitted to the hospital for some exacerbation of a chronic illness so sometimes it can be helpful to look back and see what it was about their home plan that they failed you know diuretics insulin inhalers what can we do to better support that um as they leave the hospital this time many of our patients on internal medicine it's the same at georgetown as it was it's the same at university of maryland as it was at georgetown they suffer from polypharmacy right so there may be some opportunity to simplify home care plans by reducing polypharmacy in fact there have been a few recent studies that looked at introducing a clinical pharmacist to internal medicine rounds with a strict de-prescribing protocol and where that protocol was used the patients did leave with fewer medications of course but they also had fewer rates of readmissions so there may be some opportunity there to make uh the care plan for the patient a little more manageable so one of the most critical elements another layer of the discharge process that is required to help a patient understand how to take care of themselves at home is bedside education i can say at least at my institution inpatient bedside education is not very well standardized who does the teaching what they teach and how they do it in terms of who does the teaching it can be nurses pharmacists the physicians provide some education physical therapists occupational therapists dietitians that all that adage comes to mind if it's everyone's responsibility it's really no one's right what we end up teaching is sort of haphazard too we we decided the last minute that maybe a patient needs a little extra education about insulin um so there's certainly some opportunity to standardize to assign specific tasks for teaching to particular team members right depending on what the patient is admitted for in terms of how we teach i think a lot of times we talk at patients and we don't necessarily assess whether or not they understand what we've said to them but there is a method that has some evidence in support of it called the teach back method so essentially in its most basic form the teach-back is a way of assessing whether or not the patient understands in essence you have them repeat back to you in their own language what you taught them and if you find a discrepancy in their understanding you can repeat you know the education as necessary when the teach-back was used in some heart failure studies starting on a mission throughout the heart failure admission and at discharge there was some reduction in readmissions so there may be some opportunity to implement the teach-back and more standardization to education to better support the patients at home the next layer of the discharge process is our hand off to the primary care physician right the traditional way of doing this is using the discharge summary anecdotally we hear from our partners who work outside of the hospital that the receipt rates for discharge summaries are low we know when it was formally studied the rates were actually abysmal and the information that was included was often missing important things like tests that were outstanding and admission diagnoses even to be fair though that study was done before the introduction of the electronic medical record the problem with the emr although it does solve some of those problems is that if the pcp doesn't use the same vendor as the hospital who's discharging the patient they likely won't see the discharge summary one of the tools that was introduced to sort of bridge that gap is something called a health information exchange so the idea is it can pull information from various electronic health records so that you can see things outside of your vendor we have one in maryland i don't know if you can use it in dc but i can tell you that our experience is that the information that is included is haphazard it's bulky it's relatively poorly organized so it's not reliable as a tool to ensure that the pcp will receive the discharge summary after discharge certainly a step in the right direction though but let's just say right let's just say that we have a patient we have created a very straightforward simple plan we've educated them we've provided a warm handoff to the primary out in the community patients will still fail discharge so what is it about those patients is it their own fault i think it's easy for us sometimes to blame the patients for their circumstances but i do want to point out a few opportunities for us to change our practice to better meet the patients where they are so probably one of the most common obstacles to a soft landing in the community is this concept of health literacy so health literacy is different than regular literacy the way that we know that word i think of it as a way that a patient can use or does use health information that's based not just on their education but also on their social and cultural backgrounds their life experiences maybe even their politics we're seeing right we know that the the rates of health literacy inadequate health literacy are relatively high and when it was surveyed nationally it was found that 36 percent of patients have inadequate health literacy to care for themselves essentially to follow a care plan i think in our patient population up in baltimore the rates are probably even higher than this on the heels of this survey the institute of medicine reminds us that it's really our responsibility though as the care team to communicate with patients in a way that they understand when we don't um we know that patients have disease progression and complications at higher rates if they have low literacy we know they present in higher numbers to hospitals to emergency departments to urgent cares and once they present there they're more likely to be admitted to the hospital we also know that this perfect storm among elderly patients has higher rates of mortality so it seems important for us to recognize these patients and how do we do that should we be screening our patients who are admitted to the hospital for low health literacy so there are plenty of tools out there to do that on my last check 133 through the hrq website in the national libraries of medicine while these are wonderful research tools mostly they're pretty cumbersome to bring into everyday clinical care so we need another way i think as frontline clinicians it makes sense to know the red flags for low health literacy and i think many of us do know that if a patient can't name their medications or give a history if they don't come to appointments or follow up with tests we know that they're going to struggle to carry out whatever care plan we have the take home point today is to remember that just because a patient is not demonstrating any of these red flags it doesn't mean that they actually have adequate health literacy to carry out their care plan at home so the struggle is to identify that subset of patients and how do we do that easily in the midst of our busy clinical day so it turns out there's one question that has been validated in various groups including low-income groups and spanish-speaking groups among others how confident are you filling out forms by yourself so if a patient answers anything other than they feel confident or very confident with filling out forms by themselves they've essentially screened in as having low health literacy right and so once we know that about a patient what do we do well we can gear all of our interactions in a way that makes things clearer so rounds right reducing our jargon we forget sometimes that we talk a different language and it's easy for us to slip into medical jargon when we're at the bedside but we can use to teach back right we've talked to the patient and if we used to teach back and it becomes clear to us that they don't understand the teach back is not just a nursing tool okay incorporate family where possible education i talked a lot about things like assigning tasks standardizing it somehow using teach back by all of the team members and reinforcing where necessary and discharge instructions i'm going to talk more about too but in terms of health literacy preparation it's important that in any instruction any patient material is readable for the patients and so what that means is that the nih recommends that reading material for patients is written at a sixth grade level or lower if you are personally writing any portion of your discharge instructions there are ways to check that through microsoft word or on the internet you can check the grade level at which you've written your your document okay so these are these are just some strategies to help those patients who have low health literacy there are other patient factors though and i'm sure the first things that came to mind when i said that are those patients who suffer from poverty or active drug use maybe untreated or under-treated mental illness we all know that those patients will struggle to carry out even the most straightforward care plans i'm not going to talk in any more detail about it today although to mention that i do think one of the nice things that's come out of these incentive programs is that hospital systems are really putting their arms around these this patient population reaching out into the community to better support the patients after discharge i do want to save some time to talk about one other patient factor which i think is probably less well recognized it's called post hospital syndrome so it was first described in 2013 in the new england journal by uh by dr krumholz basically he looked at that original jenks data the discrepancy between the original admission diagnosis and the readmission diagnosis and he theorized that the reason was because patients leave the hospital in this state of psychological emotional and physical vulnerability that really confers an increased risk for all kinds of downstream consequences and since that original article other authors have gone on to to better describe those triggers and the downstream you know physiologic consequences but it makes good sense right um to us the hospital is the hospital it's a 24-hour a day operation and we can forget how sleep deprived patients get while they're in the hospital from things like q4 hour vital signs um we still do things like mris in the middle of the night at university um hospital we still have semi-private rooms so if you have a noisy roommate you don't sleep your entire admission we make patients mpo they starve waiting for tests and procedures sometimes for days on end they become physically deconditioned from our bed rest orders we give medications that induce delirium and all of this is in the context of whatever the original admission diagnosis is we may see the patient as having a relatively easy to manage chronic medical condition but all they may hear is that they have an organ failing that brings incredible stress to patients i was actually tickled to see this article this month in the annals of internal medicine which is essentially a summary of all those things i just described they call it how hospital stays resemble enhanced interrogation and do they ever right if we consider the patient experience this way it's really no wonder that patients struggle to carry out their care plan as they leave the hospital we do see some work in things like ward quiet hours and environmental delirium precautions to help mitigate some of those triggers but we have a long way to go so i think for those of us who work in the clinical trenches one of the first things that we can do is really recognize that this is a phenomenon and recruit loved ones to help with the patients you know as they transition home in fact the residents that work with me are used to hearing me ask at the end of their presentation if it's not otherwise clear who loves this patient and this is why even the most highly educated health literate patient leaves us in this state of vulnerability so we really serve all of the patients best by recruiting a loved one to help them transition home so there's one final layer of the discharge process which i think is actually the most important it is the discharge instructions we call it the after visit summary or the avs let's consider the patient we just discussed who's leaving the hospital in this haze of starvation and delirium right we're sending them out in the world what they leave with is their paper instructions right usually a stack of papers if we're being accurate right and really this stack of papers is their lifeline with their care instructions never have we seen this more clearly than during the covid pandemic when there were visitor restrictions and patients weren't allowed to have anyone at the bedside with them during education so they have this stack of papers and they take it out in the world and we wish them good luck essentially so we're going to talk in some detail about the discharge instructions many of you may remember fondly or not so fondly this version of the discharge instructions um in triplicate this is the paper version that we had before the electronic health record so you can see the content is similar so things like follow-up appointments medications anticipatory guidance it was all here except it was all beautifully entered by hand usually by some hard-working student or intern as you can imagine it was high risk for all kinds of human entry error things like errors of omission handwriting problems right um this wasn't just a scattered institutional problem though everyone was handwriting their discharge instructions they were handwriting everything and with the prevalence of computers in our lives in the early 2000s it became obvious that you know we could use computers somehow to automate at least some features of care delivery to safeguard patients from this human entry error so in the late 2000s the affordable care act brought us the meaningful use program which among other things incentivized hospitals to adopt electronic health records within meaningful use there was also specific guidance surrounding the after visit summary it dictated that in order to meet your incentive and get your bonus you needed to include these specific 20 items that were considered essential for the after visit summary so did the program work well so here we see the number of physician practices on the left the number of hospitals on the right who did adopt the electronic health record from the years 2011 to 2013 and as you can see the adoption was fast and furious and at this time those vendor companies were working hard to create these contracts with the practices and hospital systems interestingly during this time clinician involvement for interface development and output development was relatively small and patient input was non-existent so these were the circumstances that brought us the abs we know today right so hurried development with minimal clinician input and zero patient input rushed passive adoption without much scrutiny by practices and hospital systems just to meet the regulatory requirement and not be penalized right but remember the point of this one of the one of the points of this program was to reduce the risk of human entry error except now that the ehr has been with us for a decade we know that it is only as good as the human who's operating it right that idea of garbage and garbage out comes to mind let me show you an example of what i mean so this is um a version this is a sample of an after visit summary it's a mock patient it's not real information so your first impression for abs is probably that it's pretty busy overwhelming there's a lot of information here you can't see the other 10 pages of the document so you don't know that this information the blue box is redundant it's pulled from elsewhere it has some appointments but not all of the appointments you find the full list of appointments on a different part of the document you also see that we give the patient some information that maybe you don't think they need like the information they gave us their home address their preferred language you see we give the patient their vital signs down to their body surface area right i do want to draw your attention to this section here this is the instruction section where the patient's told to start stop and change medications when they get home it doesn't matter how good your discharge plan was how effective in the hospital it was if your medication list on admission here is not accurate the computer doesn't know it and they will still give confusing instructions to the patient and it's pretty common for us that patients are who are admitted to the general medical services don't know their home medication list and it is common that they are admitted at a time of day when you can't reach their primary you can't reach their pharmacist and you usually can't even reach a loved one so the patient gets admitted with a medication list that's been stuck in the electronic health record since their last encounter which could have been years ago and if during the hospitalization that list wasn't updated the discharge instructions the patient left with were inaccurate so seeing this abs go out day after day and knowing about the readmission problem this quote started to really resonate with me right every system is perfectly designed to get the result it gets of course we're sending patients out in the world with instructions that are you know inaccurate and overwhelming and not particularly relevant to their care so this is what really inspired the work by my current team which is to investigate patient usability of the after visit summary so what is usability it's a term that is used in engineering and informatics to describe a user's experience with technology or devices really we're all users in our everyday life and i don't just mean with the electronic health record things like your car your coffee pot even doors right for all of the items that you use throughout your day there's usually been some engineer who worked hard to make its use more intuitive and to make your life easier although i do recognize it doesn't always feel that way right especially using the electronic health record i do want to assure you though there's a whole field that is burgeoning to help make our lives better in terms of ehr use the medical informatics is an is a field that's been growing the american medical informatics association is the national organization that sort of organizing this this group of experts and in 2015 they created a task force to set out a vision for how the ehr would grow and a lot of their goals are very clinician-centric they want your workflow to be better they want your practices and your hospital systems to meet regulatory requirements and that's what they've set out but i was very um happy to see that they're they're number nine and number 10 task force items are to work toward patient-centric care delivery and within this you know things like usability would be included so what does make patient materials more usable well the content needs to be accurate of course the layout being well organized the presentation efficient and they need to be readable which i discussed earlier but even when those pieces of the puzzle are there there may be some secret sauce you know the most important thing is regardless of what it is will the patient use it so we set out on this journey to figure out what makes a usable abs by our patient population applying human factors engineering principles and health literacy best practices we are recruiting patients who have been admitted to our general medical services and have a diagnosis of diabetes and are on insulin because this is this is what uh the scenario we use in our usability lab after the patients are discharged they come back for their usability testing they come to a private room they meet with a study facilitator and a time keeper everything is recorded we collect a fair amount of survey data which is all listed here and then we look at specific outcomes including task success and failure time to test completion and confidence which i'll get into in a little more detail in just a minute so our first round of usability participants are here this is the demographic information as you can see the educational background is relatively diverse but we're working with mostly a middle age range population extremely low income most on disability the milkas were lower than one would expect in this age range and the health literacy scores were below high school for most of the participants this is actually a relatively fair representation of our west baltimore patient population so the avs usability participants came back after discharge to the usability lab where they were presented a mock scenario that they had recently been discharged after a hospitalization for diabetes that was out of control within the room we tried to simulate the experience of returning home after a hospitalization we know that patients hang on to all of their medications and they actually told us of one of the surveys that they know the doctors are going to change their dose later so they hang on to that listener problem 10 milligrams when you make it 20. right so we try to simulate that experience of having multiple bottles the same drug in different doses different drugs from the same class to give that experience of being at home the patients were given a mock abs so you've seen the front page already that is the university of maryland version that we used this one was a 12 page document which is pretty standard for us there are definitely definitely get longer than that and you know when we're lucky they're shorter and then they underwent a task analysis so this is the data collection tool the front page of what we use to to go through that task analysis the participants are asked to go through 23 tasks care tasks things that are relatively routine for home care you know find me this appointment what phone number do you call how do you manage this particular symptom were the sorts of tasks that were included they were scored as a task success or failure if they were able to complete it based on the expected response one thing that was noted that's not on this sheet too i'll talk a little bit more about was whether or not the participant used the abs to get the task done or complete the you know answer the question we looked at time to completion and then we asked the participant once they had completed the task how confident they were that they had actually done it the right way so our results um were relatively interesting patients did really well the participants rather did really well with tasks that were found the answers were found right on the front page almost universally they got those right the tasks that required the participant to use information that was later in the document even the same sorts of questions like finding appointment information or finding a phone number to call about prescriptions on pages three four and five only half of the participants were able to do that the right way when information was buried relatively deep in the document and in a format that was a little bit different that required more reading the participants really struggled with that and only one out of the six participants was able to to find that information and use it to answer the task questions appropriately when participants or patients leave a general medicine service we think that one of the most important things is that they understand what medications they have to take it home and our first task was to ask the participants to use the medication list in the avs and pull out the medications they would be required to take basically match up the list the idea is to simulate what you would do if you were about to fill a pillbox and in fact not one of the participants was able to do that successfully other medication questions were met with some struggle as well so only a third of the participants could answer disease specific information about what to do for high sugars what doses to take in certain situations with their blood sugars in situations where the participant needed to find information on two different pages of the medication list were also met with relatively poor success only a third of the participants were able to get those done correctly so i'm going to show you just one other way of looking at our data this is showing six of the tasks that we asked the participants to perform i know this is a little busy you see each participant listed as a column and you see the the task written with the time to completion the confidence score they provided where you see a green box is where that participant answered that task or question correctly where you see a red box they failed to do it correctly where you see a yellow box that is where the participant did actually get the task done or answer the question correctly but they did it without using the document for guidance so a couple of other things i want to point out you see there aren't very many green boxes the document really failed to guide patients to perform their care routinely but they did sometimes you know spend quite a bit of time looking for the answers even when they did get it right i think even more interestingly where we have a lot of the task failures it wasn't for lack of trying the participants often spent minutes looking for the right answer and still either couldn't find it or when they did find it they couldn't extract the information in a way that was usable to complete the task one of the other interesting findings we had is that you see all of these red boxes but often the participants felt like they had answered the questions on the task correctly so some overconfidence was a pattern that we saw we did also uh perform a satisfaction survey with the participants about the abs they had received as a patient leaving the hospital and satisfaction could be described as marginal at best they felt like the abs was often inconsistent and hard to understand so in summary of those observations the document is too long and patients rarely reference the later pages that front page is prime real estate that became clear the medication list is confusing extracting instructions from the text was confusing that anticipatory guidance which can help keep patients home instead of having them return to the emergency department sometimes which is really important success is often reliant on prior knowledge which can be hazardous if the knowledge isn't right and overconfidence was a pattern we saw which can be equally hazardous and of course the user satisfaction is sub-optimal so we took this data to a team of experts and we convened a design studio so you see all of the experts who were part of the redesign here we had experts in health literacy informatics human factors engineering we were also lucky to have some of the team leads from the corporate office of our electronic health record who joined us to sort of weigh in about you know the options we had within the interface of the electronic health record and this team made some recommendations which were to reprioritize information we know now the front page has got to have only the most important stuff so the diagnosis anticipatory guidance appointments and diet care instructions recommending simplifying language removing unnecessary and redundant information removing potentially hazardous information like i showed you before the inaccuracies and deprioritizing removing less important information and where we could optimizing that medication list so some of the ideas that were brought up in this meeting were two cluster medications either by disease or by time of day that they're taken or used pictures where possible so we took this information to the informatics team and this is what we came up with you see the original mock here on the left and on the right is the new version the next prototype so we call it now instructions for home instead of calling it the abs and discharge instructions and you can see that we've reorganized things so right here on the front page it is what you need to know who to call and you can notice that on the original version the phone number for reaching a physician from the hospitalization was not there so now what you need to know who to call what to eat what to do and where to be it's all right here on the front page you can see that we simplified some of the language so some steps in the right direction toward the recommendations from the group i can show you here we tried hard to fit medications in a place that would be on the front page there was just no way to do it so they do follow now right on the second page we also met some limitations through the vendor in terms of reorganizing medications by disease or using pictures but instead we were able to use this feature which puts a check mark next to the time of day the medication should be taken so the patient can you know the patient can see from across the room you know if they're supposed to be taking the medication at particular times of day so the next steps for us is to test this prototype with the same strategy so recruitment is currently underway those participants will return back to the usability lab and undergo those same tasks the same 23 tasks and be scored in the same way and then we will take this data back to the same usability or the same design studio group for iterative redesign is needed and so we get to what we consider to be the perfect mouse trap and at that point the university of maryland medical system we are hopeful that they will adopt it for use throughout the system one final point is that no matter how usable the abs is in the usability lab you can never really assume that the patient in front of you understands it so we have one final layer which i think is important to mention here so we have a master educator a nurse practitioner who does something we call the avs teach back so she finds our high risk for readmission patients she takes the abs to their bedside and reviews with them and then she asks them these four questions what did they tell you was wrong with you and what did we do for you here in the hospital what medications will you take when you're home when is your appointment and will you be able to make it and who will you call if you have a question and show me the number right so this has been a wonderful safety net for our patient population it's added a whole new level of security for us to be sure that the patient can actually understand the abs that they have so in summary hospital discharge is an important care transition and many patients fail to transition home without issue we can adapt our educational strategies to overcome patient limitations like inadequate health literacy loved ones should be recruited to service the custodians of the care plan at least in that immediate period following hospitalization and opportunities exist for us to refine our patient-facing materials to make them more usable readable and actionable so i want to finish with this cartoon that i found which i thought was a pretty pessimistic view of patient care in the day and age of the electronic health record and so you can see here's the patient in the middle of the picture and the two doctors are facing away from the patient looking at their computer and their tablet i tend to have a more optimistic view or vision of the future of patient care and so i fixed this so in my version the doctor here on the left has his arms reached out to the patient maybe to do an exam maybe to give a hug and the doctor here on the right is holding not a tablet but that is an abs that is patient-centered usable well-organized actionable and he's doing a teach back with it with the patient so with that i have a whole host of acknowledgements here everyone who is listed here on the screen has been instrumental in helping pull this together dr fink is actually my research mentor and co-investigator and rebecca dorfler is our research associate who makes all of the magic happen behind the scenes from recruitment to running the usability lab and we have been so lucky to have some institutional support for this labor of love so i wanted to acknowledge that too and with that i am happy to take any questions
Show moreFrequently asked questions
How can I make documents so that someone else can electronically sign them?
How can I incorporate an electronic signature solution into my workflow?
How do I create a PDF for someone to sign?
Get more for signed electronically Hospital Discharge made easy
- Print electronically sign Registration Rights Agreement
- Prove electronically signing Letter of Recommendation for College
- Endorse digi-sign Contractor Invoice
- Authorize signature service Release of Liability Form (Waiver of Liability)
- Anneal mark settlement
- Justify eSignature Website Design Inquiry
- Try initial Baptism Invitation
- Add Split Dollar Agreement electronic signature
- Send Window Cleaning Proposal Template signed electronically
- Fax Insurance Waiver electronically sign
- Seal Employee Engagement Survey electronically signing
- Password Insurance Plan mark
- Pass Book Publishing Contract Template signed
- Renew Wedding Photography Quotation Request Template autograph
- Test Foster Application digital sign
- Require Residential Lease Agreement Template initial
- Comment self electronically signed
- Boost sponsor eSign
- Compel attestor initials
- Void Newborn Photography Contract Template template countersign
- Adopt Tag-Along Agreement template sign
- Vouch Free Business Proposal template electronically signing
- Establish Free Certificate of Achievement template eSign
- Clear Vendor Agreement Template template eSignature
- Complete Drama Scholarship Application template autograph
- Force Job Proposal Template template digisign
- Permit Dietary Requirements template electronic signature
- Customize Horse Boarding Contract Template template signed electronically